Monoclonal Antibodies As Tools to Combat Fungal Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FINAL RISK ASSESSMENT for Aspergillus Niger (February 1997)
ATTACHMENT I--FINAL RISK ASSESSMENT FOR Aspergillus niger (February 1997) I. INTRODUCTION Aspergillus niger is a member of the genus Aspergillus which includes a set of fungi that are generally considered asexual, although perfect forms (forms that reproduce sexually) have been found. Aspergilli are ubiquitous in nature. They are geographically widely distributed, and have been observed in a broad range of habitats because they can colonize a wide variety of substrates. A. niger is commonly found as a saprophyte growing on dead leaves, stored grain, compost piles, and other decaying vegetation. The spores are widespread, and are often associated with organic materials and soil. History of Commercial Use and Products Subject to TSCA Jurisdiction The primary uses of A. niger are for the production of enzymes and organic acids by fermentation. While the foods, for which some of the enzymes may be used in preparation, are not subject to TSCA, these enzymes may have multiple uses, many of which are not regulated except under TSCA. Fermentations to produce these enzymes may be carried out in vessels as large as 100,000 liters (Finkelstein et al., 1989). A. niger is also used to produce organic acids such as citric acid and gluconic acid. The history of safe use for A. niger comes primarily from its use in the food industry for the production of many enzymes such as a-amylase, amyloglucosidase, cellulases, lactase, invertase, pectinases, and acid proteases (Bennett, 1985a; Ward, 1989). In addition, the annual production of citric acid by fermentation is now approximately 350,000 tons, using either A. -

Turning on Virulence: Mechanisms That Underpin the Morphologic Transition and Pathogenicity of Blastomyces
Virulence ISSN: 2150-5594 (Print) 2150-5608 (Online) Journal homepage: http://www.tandfonline.com/loi/kvir20 Turning on Virulence: Mechanisms that underpin the Morphologic Transition and Pathogenicity of Blastomyces Joseph A. McBride, Gregory M. Gauthier & Bruce S. Klein To cite this article: Joseph A. McBride, Gregory M. Gauthier & Bruce S. Klein (2018): Turning on Virulence: Mechanisms that underpin the Morphologic Transition and Pathogenicity of Blastomyces, Virulence, DOI: 10.1080/21505594.2018.1449506 To link to this article: https://doi.org/10.1080/21505594.2018.1449506 © 2018 The Author(s). Published by Informa UK Limited, trading as Taylor & Francis Group© Joseph A. McBride, Gregory M. Gauthier and Bruce S. Klein Accepted author version posted online: 13 Mar 2018. Submit your article to this journal Article views: 15 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=kvir20 Publisher: Taylor & Francis Journal: Virulence DOI: https://doi.org/10.1080/21505594.2018.1449506 Turning on Virulence: Mechanisms that underpin the Morphologic Transition and Pathogenicity of Blastomyces Joseph A. McBride, MDa,b,d, Gregory M. Gauthier, MDa,d, and Bruce S. Klein, MDa,b,c a Division of Infectious Disease, Department of Medicine, University of Wisconsin School of Medicine and Public Health, 600 Highland Avenue, Madison, WI 53792, USA; b Division of Infectious Disease, Department of Pediatrics, University of Wisconsin School of Medicine and Public Health, 1675 Highland Avenue, Madison, WI 53792, USA; c Department of Medical Microbiology and Immunology, University of Wisconsin School of Medicine and Public Health, 1550 Linden Drive, Madison, WI 53706, USA. -

Perspectives on in Vitro Diagnostic Devices, Regulated by the Office Of
1 2 “This transcript appears as received from the commercial transcribing service after inclusion of minor corrections to typographical and factual errors recommended by the Technical Point of Contact.” 1 PERSPECTIVES ON IN VITRO DIAGNOSTIC DEVICES, 2 REGULATED BY THE OFFICE OF BLOOD RESEARCH AND REVIEW 3 4 FOOD AND DRUG ADMINISTRATION 5 WHITE OAK CAMPUS 6 BUILDING 31 7 10903 NEW HAMPSHIRE AVENUE 8 SILVER SPRING, MARYLAND 20903 9 10 TUESDAY, JULY 16, 2019 11 8:30 A.M. 12 13 APPEARANCES: 14 MODERATOR: TERESITA C. MERCADO, MS 15 16 WELCOME: 17 JULIA LATHROP, PHD, DETTD/OBRR 18 19 INTRODUCTION: 20 WENDY PAUL, MD, DBCD/OBRR 21 22 PRESENTERS: 23 KIMBERLY BIGLER, MLS(ASCP)CMSBB, DBCD/OBRR 1 ANNETTE RAGOSTA, MT(ASCP)SBB, DBCD/OBRR 2 ZHUGONG "JASON" LIU, PHD, DRB/DBCD 3 4 CONFERENCE 5 TUESDAY, JULY 16, 2019 6 8:30 A.M. 7 DR. LATHROP: Okay, everybody. Thank you for coming to the second day of 8 our workshop which is going to be focused on considerations for IVDs regulated by the Division 9 of Blood Components and Devices in OBRR. 10 Again, the slides will be available on the website in about two weeks, so take a 11 look for them there. And moderating today’s session is Teresita Mercado from the Division. 12 MS. MERCADO: Good morning. Welcome to session three of the IVD 13 workshop. Our first speaker will be Dr. Wendy Paul. She is the deputy director of DBCD who 14 will give us an introduction to devices in DBCD. 15 DR. -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Fungal Infection in the Lung
CHAPTER Fungal Infection in the Lung 52 Udas Chandra Ghosh, Kaushik Hazra INTRODUCTION The following risk factors may predispose to develop Pneumonia is the leading infectious cause of death in fungal infections in the lungs 6 1, 2 developed countries . Though the fungal cause of 1. Acute leukemia or lymphoma during myeloablative pneumonia occupies a minor portion in the immune- chemotherapy competent patients, but it causes a major role in immune- deficient populations. 2. Bone marrow or peripheral blood stem cell transplantation Fungi may colonize body sites without producing disease or they may be a true pathogen, generating a broad variety 3. Solid organ transplantation on immunosuppressive of clinical syndromes. treatment Fungal infections of the lung are less common than 4. Prolonged corticosteroid therapy bacterial and viral infections and very difficult for 5. Acquired immunodeficiency syndrome diagnosis and treatment purposes. Their virulence varies from causing no symptoms to death. Out of more than 1 6. Prolonged neutropenia from various causes lakh species only few fungi cause human infection and 7. Congenital immune deficiency syndromes the most vulnerable organs are skin and lungs3, 4. 8. Postsplenectomy state RISK FACTORS 9. Genetic predisposition Workers or farmers with heavy exposure to bird, bat, or rodent droppings or other animal excreta in endemic EPIDEMIOLOGY OF FUNGAL PNEUMONIA areas are predisposed to any of the endemic fungal The incidences of invasive fungal infections have pneumonias, such as histoplasmosis, in which the increased during recent decades, largely because of the environmental exposure to avian or bat feces encourages increasing size of the population at risk. This population the growth of the organism. -

Phage Display-Based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed Against Human Pathogens
Int. J. Mol. Sci. 2012, 13, 8273-8292; doi:10.3390/ijms13078273 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Phage Display-based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed against Human Pathogens Nicola Clementi *,†, Nicasio Mancini †, Laura Solforosi, Matteo Castelli, Massimo Clementi and Roberto Burioni Microbiology and Virology Unit, “Vita-Salute” San Raffaele University, Milan 20132, Italy; E-Mails: [email protected] (N.M.); [email protected] (L.S.); [email protected] (M.C.); [email protected] (M.C.); [email protected] (R.B.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-2643-5082; Fax: +39-2-2643-4288. Received: 16 March 2012; in revised form: 25 June 2012 / Accepted: 27 June 2012 / Published: 4 July 2012 Abstract: In the last two decades, several phage display-selected monoclonal antibodies (mAbs) have been described in the literature and a few of them have managed to reach the clinics. Among these, the anti-respiratory syncytial virus (RSV) Palivizumab, a phage-display optimized mAb, is the only marketed mAb directed against microbial pathogens. Palivizumab is a clear example of the importance of choosing the most appropriate strategy when selecting or optimizing an anti-infectious mAb. From this perspective, the extreme versatility of phage-display technology makes it a useful tool when setting up different strategies for the selection of mAbs directed against human pathogens, especially when their possible clinical use is considered. -

Bats (Myotis Lucifugus)
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln The Handbook: Prevention and Control of Wildlife Damage Management, Internet Center Wildlife Damage for January 1994 Bats (Myotis lucifugus) Arthur M. Greenhall Research Associate, Department of Mammalogy, American Museum of Natural History, New York, New York 10024 Stephen C. Frantz Vertebrate Vector Specialist, Wadsworth Center for Laboratories and Research, New York State Department of Health, Albany, New York 12201-0509 Follow this and additional works at: https://digitalcommons.unl.edu/icwdmhandbook Part of the Environmental Sciences Commons Greenhall, Arthur M. and Frantz, Stephen C., "Bats (Myotis lucifugus)" (1994). The Handbook: Prevention and Control of Wildlife Damage. 46. https://digitalcommons.unl.edu/icwdmhandbook/46 This Article is brought to you for free and open access by the Wildlife Damage Management, Internet Center for at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in The Handbook: Prevention and Control of Wildlife Damage by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Arthur M. Greenhall Research Associate Department of Mammalogy BATS American Museum of Natural History New York, New York 10024 Stephen C. Frantz Vertebrate Vector Specialist Wadsworth Center for Laboratories and Research New York State Department of Health Albany, New York 12201-0509 Fig. 1. Little brown bat, Myotis lucifugus Damage Prevention and Air drafts/ventilation. Removal of Occasional Bat Intruders Control Methods Ultrasonic devices: not effective. When no bite or contact has occurred, Sticky deterrents: limited efficacy. Exclusion help the bat escape (otherwise Toxicants submit it for rabies testing). Polypropylene netting checkvalves simplify getting bats out. None are registered. -

Therapeutic Monoclonal Antibody for Sporotrichosis
REVIEW ARTICLE published: 28 November 2012 doi: 10.3389/fmicb.2012.00409 Therapeutic monoclonal antibody for sporotrichosis Sandro R. Almeida* Faculty of Pharmaceutical Sciences, Department of Clinical e Toxicological Analysis, University of São Paulo, São Paulo, Brazil Edited by: Sporotrichosis is a chronic subcutaneous mycosis that affects both humans and animals Carlos P. Taborda, University of São worldwide. This subcutaneous mycosis had been attributed to a single etiological agent, Paulo, Brazil Sporothrix schenckii. S. schenckii exhibits considerable genetic variability, and recently, it Reviewed by: was suggested that this taxon consists of a complex of species. Sporotrichosis is caused Carlos P. Taborda, University of São Paulo, Brazil by traumatic inoculation of the fungus, which is a ubiquitous environmental saprophyte Augusto Schrank, Federal University that can be isolated from soil and plant debris. The infection is limited to cutaneous forms, of Rio Grande do Sul, Brazil but recently, more severe clinical forms of this mycosis have been described, especially *Correspondence: among immunocompromised individuals. The immunological mechanisms involved in Sandro R. Almeida, Faculdade de the prevention and control of sporotrichosis are not well understood. Some studies Ciências Farmacêuticas, Departamento de Análises Clínicas suggest that cell-mediated immunity plays an important role in protecting the host e Toxicológicas, Universidade de against S. schenckii. In contrast, the role of the humoral immune response in protection São Paulo, Avenida Prof. Lineu against this fungus has not been studied in detail. In a previous study, we showed that Prestes, 580, Bloco 17, São Paulo, antigens secreted by S. schenckii induced a specific humoral response in infected animals, Brazil. -

MM 0839 REV0 0918 Idweek 2018 Mucor Abstract Poster FINAL
Invasive Mucormycosis Management: Mucorales PCR Provides Important, Novel Diagnostic Information Kyle Wilgers,1 Joel Waddell,2 Aaron Tyler,1 J. Allyson Hays,2,3 Mark C. Wissel,1 Michelle L. Altrich,1 Steve Kleiboeker,1 Dwight E. Yin2,3 1 Viracor Eurofins Clinical Diagnostics, Lee’s Summit, MO 2 Children’s Mercy, Kansas City, MO 3 University of Missouri-Kansas City School of Medicine, Kansas City, MO INTRODUCTION RESULTS Early diagnosis and treatment of invasive mucormycosis (IM) affects patient MUC PCR results of BAL submitted for Aspergillus testing. The proportions of Case study of IM confirmed by MUC PCR. A 12 year-old boy with multiply relapsed pre- outcomes. In immunocompromised patients, timely diagnosis and initiation of appropriate samples positive for Mucorales and Aspergillus in BAL specimens submitted for IA testing B cell acute lymphoblastic leukemia, despite extensive chemotherapy, two allogeneic antifungal therapy are critical to improving survival and reducing morbidity (Chamilos et al., are compared in Table 2. Out of 869 cases, 12 (1.4%) had POS MUC PCR, of which only hematopoietic stem cell transplants, and CAR T-cell therapy, presented with febrile 2008; Kontoyiannis et al., 2014; Walsh et al., 2012). two had been ordered for MUC PCR. Aspergillus was positive in 56/869 (6.4%) of neutropenia (0 cells/mm3), cough, and right shoulder pain while on fluconazole patients, with 5/869 (0.6%) positive for Aspergillus fumigatus and 50/869 (5.8%) positive prophylaxis. Chest CT revealed a right lung cavity, which ultimately became 5.6 x 6.2 x 5.9 Differentiating diagnosis between IM and invasive aspergillosis (IA) affects patient for Aspergillus terreus. -

WO 2016/176089 Al 3 November 2016 (03.11.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/176089 Al 3 November 2016 (03.11.2016) P O P C T (51) International Patent Classification: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, A01N 43/00 (2006.01) A61K 31/33 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (21) International Application Number: KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, PCT/US2016/028383 MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (22) International Filing Date: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 20 April 2016 (20.04.2016) SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of regional protection available): ARIPO (BW, GH, (30) Priority Data: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, 62/154,426 29 April 2015 (29.04.2015) US TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, (71) Applicant: KARDIATONOS, INC. [US/US]; 4909 DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, Lapeer Road, Metamora, Michigan 48455 (US). -
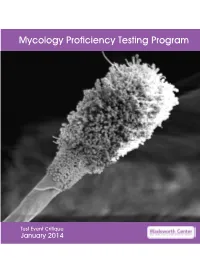
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Sporothrix Schenckii and Sporotrichosis
Anais da Academia Brasileira de Ciências (2006) 78(2): 293-308 (Annals of the Brazilian Academy of Sciences) ISSN 0001-3765 www.scielo.br/aabc Sporothrix schenckii and Sporotrichosis LEILA M. LOPES-BEZERRA1, ARMANDO SCHUBACH2 and ROSANE O. COSTA3 1Universidade do Estado do Rio de Janeiro/UERJ Instituto de Biologia Roberto Alcantara Gomes, Departamento de Biologia Celular e Genética Rua São Francisco Xavier, 524 PHLC, sl. 205, Maracanã 20550-013 Rio de Janeiro, RJ, Brasil 2Instituto Oswaldo Cruz, Instituto de Pesquisa Clínica Evandro Chagas Departamento de Doenças Infecciosas, Av. Brasil 4365, Manguinhos 21040-900 Rio de Janeiro, RJ, Brasil 3Universidade do Estado do Rio de Janeiro/UERJ, Hospital Universitário Pedro Ernesto Av. 28 de Setembro 77, Vila Isabel, 20551-900 Rio de Janeiro, RJ, Brasil Manuscript received on September 26, 2005; accepted for publication on October 10, 2006 presented by LUIZ R. TRAVASSOS ABSTRACT For a long time sporotrichosis has been regarded to have a low incidence in Brazil; however, recent studies demonstrate that not only the number of reported cases but also the incidence of more severe or atypical clinical forms of the disease are increasing. Recent data indicate that these more severe forms occur in about 10% of patients with confirmed diagnosis. The less frequent forms, mainly osteoarticular sporotrichosis, might be associated both with patient immunodepression and zoonotic transmission of the disease. The extracutaneous form and the atypical forms are a challenge to a newly developed serological test, introduced as an auxiliary tool for the diagnosis of unusual clinical forms of sporotrichosis. Key words: sporotrichosis, diagnosis, epidemiology, drugs, cell wall, antigens.