Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Allergic Bronchopulmonary Aspergillosis Revealing Asthma
CASE REPORT published: 22 June 2021 doi: 10.3389/fimmu.2021.695954 Case Report: Allergic Bronchopulmonary Aspergillosis Revealing Asthma Houda Snen 1,2*, Aicha Kallel 2,3*, Hana Blibech 1,2, Sana Jemel 2,3, Nozha Ben Salah 1,2, Sonia Marouen 3, Nadia Mehiri 1,2, Slah Belhaj 3, Bechir Louzir 1,2 and Kalthoum Kallel 2,3 1 Pulmonary Department, Hospital Mongi Slim, La Marsa, Tunisia, 2 Faculty of Medicine, Tunis El Manar University, Tunis, Tunisia, 3 Parasitology and Mycology Department, La Rabta Hospital, Tunis, Tunisia Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disorder caused by hypersensitivity to Aspergillus which colonizes the airways of patients with asthma and cystic fibrosis. Its diagnosis could be difficult in some cases due to atypical Edited by: presentations especially when there is no medical history of asthma. Treatment of ABPA is Brian Stephen Eley, frequently associated to side effects but cumulated drug toxicity due to different molecules University of Cape Town, South Africa is rarely reported. An accurate choice among the different available molecules and Reviewed by: effective on ABPA is crucial. We report a case of ABPA in a woman without a known Shivank Singh, Southern Medical University, China history of asthma. She presented an acute bronchitis with wheezing dyspnea leading to an Richard B. Moss, acute respiratory failure. She was hospitalized in the intensive care unit. The Stanford University, United States bronchoscopy revealed a complete obstruction of the left primary bronchus by a sticky *Correspondence: Houda Snen greenish material. The culture of this material isolated Aspergillus fumigatus and that of [email protected] bronchial aspiration fluid isolated Pseudomonas aeruginosa. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -

Rapid and Precise Diagnosis of Pneumonia Coinfected By
Rapid and precise diagnosis of pneumonia coinfected by Pneumocystis jirovecii and Aspergillus fumigatus assisted by next-generation sequencing in a patient with systemic lupus erythematosus: a case report Yili Chen Sun Yat-Sen University Lu Ai Sun Yat-Sen University Yingqun Zhou First Peoples Hospital of Nanning Yating Zhao Sun Yat-Sen University Jianyu Huang Sun Yat-Sen University Wen Tang Sun Yat-Sen University Yujian Liang ( [email protected] ) Sun Yat-Sen University Case report Keywords: Pneumocystis jirovecii, Aspergillus fumigatus, Next generation sequencing, Case report Posted Date: March 19th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-154016/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/12 Abstract Background: Pneumocystis jirovecii and Aspergillus fumigatus, are opportunistic pathogenic fungus that has a major impact on mortality in patients with systemic lupus erythematosus. With the potential to invade multiple organs, early and accurate diagnosis is essential to the survival of SLE patients, establishing an early diagnosis of the infection, especially coinfection by Pneumocystis jirovecii and Aspergillus fumigatus, still remains a great challenge. Case presentation: In this case, we reported that the application of next -generation sequencing in diagnosing Pneumocystis jirovecii and Aspergillus fumigatus coinfection in a Chinese girl with systemic lupus erythematosus (SLE). Voriconazole was used to treat pulmonary aspergillosis, besides sulfamethoxazole and trimethoprim (SMZ-TMP), and caspofungin acetate to treat Pneumocystis jirovecii infection for 6 days. On Day 10 of admission, her chest radiograph displayed obvious absorption of bilateral lung inammation though the circumstance of repeated fever had not improved. -

Central Nervous System Infections by Members of the Pseudallescheria
Review article Central nervous system infections by members of the Pseudallescheria boydii species complex in healthy and immunocompromised hosts: epidemiology, clinical characteristics and outcome A. Serda Kantarcioglu,1 Josep Guarro2 and G. S. de Hoog3 1Department of Microbiology and Clinical Microbiology, Cerrahpasa Medical Faculty, Istanbul, Turkey, 2Unitat de Microbiologia, Facultat de Medicina i Ciencies de la Salut, Universitat Rovira i Virgili, Reus, Spain and 3Centraalbureau voor Schimmelcultures, Utrecht, and Institute for Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands Summary Infections caused by members of the Pseudallescheria boydii species complex are currently among the most common mould infections. These fungi show a particular tropism for the central nervous system (CNS). We reviewed all the available reports on CNS infections, focusing on the geographical distribution, infection routes, immunity status of infected individuals, type and location of infections, clinical manifestations, treatment and outcome. A total of 99 case reports were identified, with similar percentage of healthy and immunocompromised patients (44% vs. 56%; P = 0.26). Main clinical types were brain abscess (69%), co-infection of brain tissue and ⁄ or spinal cord with meninges (10%) and meningitis (9%). The mortality rate was 74%, regardless of the patientÕs immune status, or the infection type and ⁄ or location. Cerebrospinal fluid culture was revealed as a not very important tool as the percentage of positive samples for P. boydii complex was not different from that of negative ones (67% vs. 33%; P = 0.10). In immunocompetent patients, CNS infection was preceded by near drowning or trauma. In these patients, the infection was characterised by localised involvement and a high fatality rate (76%). -

Redalyc.Morphological Varieties of Trichophyton Rubrum Clinical Isolates
Revista Mexicana de Micología ISSN: 0187-3180 [email protected] Sociedad Mexicana de Micología México Hernández-Hernández, Francisca; Manzano-Gayosso, Patricia; Córdova-Martínez, Erika; Méndez- Tovar, Luis Javier; López-Martínez, Rubén; García de Acevedo, Beatriz; Orozco-Topete, Rocío; Cerbón, Marco Antonio Morphological varieties of Trichophyton rubrum clinical isolates Revista Mexicana de Micología, núm. 25, diciembre, 2007, pp. 9-14 Sociedad Mexicana de Micología Xalapa, México Available in: http://www.redalyc.org/articulo.oa?id=88302504 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Morphological varieties of Trichophyton rubrum clinical isolates Francisca Hernández-Hernández 1, Patricia Manzano-Gayosso1, Erika Córdova-Martínez1, Luis Javier Méndez-Tovar2, Rubén López-Martínez1, Beatriz García de Acevedo3, Rocío Orozco-Topete3, Marco Antonio Cerbón4 1 Departamento de Microbiología y Parasitología, Facultad de Medicina, Universidad Nacional Autónoma de México. 2Servicio de Dermatología y Micología, Centro Médico Nacional (CMN) Siglo XXI, IMSS. 3Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”. 4Departamento de Biología, Facultad de Química, Universidad Nacional Autónoma de México. México, D. F., México 7 0 Variedades morfológicas de aislamientos clínicos de Trichophyton rubrum 0 2 , 4 1 Resumen. Trichophyton rubrum es el dermatofito antropofílico causante de micosis - 9 superficiales aislado con mayor frecuencia en todo el mundo. Diversas variedades : 5 2 morfológicas de este dermatofito han sido reportadas, lo cual en algunas ocasiones hace A Í difícil su identificación. Nuestro objetivo fue identificar y determinar la frecuencia de G O variedades morfológicas entre los aislados de T. -

Immunopathology of Aspergillus Infections in Children with Chronic Granulomatous Disease and Cystic Fibrosis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Aberdeen University Research Archive Immunopathology of Aspergillus Infections in Children with Chronic Granulomatous Disease and Cystic Fibrosis. Adilia Warris, MD PhD MRC Centre for Medical Mycology, Aberdeen Fungal Group, Institute of Medical Sciences, University of Aberdeen, UK. Corresponding address: Medical Research Council Centre for Medical Mycology at the University of Aberdeen, Aberdeen Fungal Group, Institute of Medical Sciences, Foresterhill, AB25 2ZD, Aberdeen, UK. Phone: +44 (0)1224437596. Fax: +44 (0)1224437506. E-mail: [email protected] Acknowledgements AW is supported by the Wellcome Trust Strategic Award (grant 097377) and the MRC Centre for Medical Mycology (grant MR/N006364/1) at the University of Aberdeen. Key Words: chronic granulomatous disease, cystic fibrosis, Aspergillus, aspergillosis, inflammation Abbreviated title: Aspergillus infections in CGD and CF Running head title: Aspergillus infections in CGD and CF Introduction Children with chronic granulomatous disease (CGD) and cystic fibrosis (CF) share some important clinical characteristics which are the consequence of their intrinsic susceptibility to recurrent and opportunistic infections and exaggerated inflammation. Although the clinical phenotypes of Aspergillus disease differ substantially between those two non-neutropenic patient groups, the underlying pathophysiology show remarkable commonalities with excessive inflammation being a hallmark of Aspergillus disease. The occurrence of Aspergillus infections in these two patient populations is associated with decreased quality of life and premature death. Our knowledge of the pathophysiology of Aspergillus infections is mainly derived from infections caused by a single species - Aspergillus fumigatus - in the neutropenic host. The insights obtained in this setting do not translate well to the non-neutropenic host. -

FINAL RISK ASSESSMENT for Aspergillus Niger (February 1997)
ATTACHMENT I--FINAL RISK ASSESSMENT FOR Aspergillus niger (February 1997) I. INTRODUCTION Aspergillus niger is a member of the genus Aspergillus which includes a set of fungi that are generally considered asexual, although perfect forms (forms that reproduce sexually) have been found. Aspergilli are ubiquitous in nature. They are geographically widely distributed, and have been observed in a broad range of habitats because they can colonize a wide variety of substrates. A. niger is commonly found as a saprophyte growing on dead leaves, stored grain, compost piles, and other decaying vegetation. The spores are widespread, and are often associated with organic materials and soil. History of Commercial Use and Products Subject to TSCA Jurisdiction The primary uses of A. niger are for the production of enzymes and organic acids by fermentation. While the foods, for which some of the enzymes may be used in preparation, are not subject to TSCA, these enzymes may have multiple uses, many of which are not regulated except under TSCA. Fermentations to produce these enzymes may be carried out in vessels as large as 100,000 liters (Finkelstein et al., 1989). A. niger is also used to produce organic acids such as citric acid and gluconic acid. The history of safe use for A. niger comes primarily from its use in the food industry for the production of many enzymes such as a-amylase, amyloglucosidase, cellulases, lactase, invertase, pectinases, and acid proteases (Bennett, 1985a; Ward, 1989). In addition, the annual production of citric acid by fermentation is now approximately 350,000 tons, using either A. -
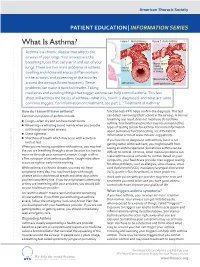
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Acute (Serious) Bronchitis
Acute (serious) Bronchitis This is an infection of the air tubes that go down to your lungs. It often follows a cold or the flu. Most people do not need treatment for this. The infection normally goes away in 7-10 days. We make every effort to make sure the information is correct (right). However, we cannot be responsible for any actions as a result of using this information. Getting Acute Bronchitis How the lungs work Your lungs are like two large sponges filled with tubes. As you breathe in, you suck oxygen through your nose and mouth into a tube in your neck. Bacteria and viruses in the air can travel into your lungs. Normally, this does not cause a problem as your body kills the bacteria, or viruses. However, sometimes infection can get through. If you smoke or if you have had another illness, infections are more likely to get through. Acute Bronchitis Acute bronchitis is when the large airways (breathing tubes) to the lungs get inflamed (swollen and sore). The infection makes the airways swell and you get a build up of phlegm (thick mucus). Coughing is a way of getting the phlegm out of your airways. The cough can sometimes last for up to 3 weeks. Acute Bronchitis usually goes away on its own and does not need treatment. We make every effort to make sure the information is correct (right). However, we cannot be responsible for any actions as a result of using this information. Symptoms (feelings that show you may have the illness) Symptoms of Acute Bronchitis include: • A chesty cough • Coughing up mucus, which is usually yellow, or green • Breathlessness when doing more energetic activities • Wheeziness • Dry mouth • High temperature • Headache • Loss of appetite The cough usually lasts between 7-10 days. -

To Honeycombing in Idiopathic Pulmonary Fibrosis
Piciucchi et al. BMC Pulmonary Medicine (2016) 16:87 DOI 10.1186/s12890-016-0245-x CORRESPONDENCE Open Access From “traction bronchiectasis” to honeycombing in idiopathic pulmonary fibrosis: A spectrum of bronchiolar remodeling also in radiology? Sara Piciucchi1*, Sara Tomassetti2, Claudia Ravaglia2, Christian Gurioli2, Carlo Gurioli2, Alessandra Dubini3, Angelo Carloni4, Marco Chilosi5, Thomas V Colby6 and Venerino Poletti2,7 Abstract Background: The diagnostic and prognostic impact of traction bronchiectasis on high resolution CT scan (HRCT) in patients suspected to have idiopathic pulmonary fibrosis (IPF) is increasing significantly. Main body: Recent data demonstrated that cysts in honeycombing areas are covered by epithelium expressing bronchiolar markers. In IPF bronchiolization is the final consequence of a variety of pathogenic events starting from alveolar stem cell exhaustion, and ending in a abnormal/dysplastic proliferation of bronchiolar epithelium. CT scan features of traction bronchiectasis and honeycombing should be interpreted under the light of these new pathogenetic and morphologic considerations. Short conclusion: We suggest that in IPF subjects traction bronchiectasis and honeycombing -now defined as distinct entities on HRCT scan- are actually diverse aspects of a continuous spectrum of lung remodeling. Keywords: Traction bronchiectasis, Honeycombing, Fibroblastic Foci, Bronchiolar dysplastic proliferation Background Mechanical stress may contribute to the subpleural Histologically, Usual Interstitial Pneumonia (UIP) is and usually basilar localization of UIP changes [10, 11]. characterized by a combination of “patchy fibrosis” and The final stage of this “bronchiolization” process cor- fibroblastic foci displaying a “patchwork pattern”. Disease responds radiologically to honeycombing, typically seen progression is characterized by the appearance of air- first in the subpleural regions of the lower lobes [2, 3]. -

Ergot Alkaloid Biosynthesis in Aspergillus Fumigatus : Association with Sporulation and Clustered Genes Common Among Ergot Fungi
Graduate Theses, Dissertations, and Problem Reports 2009 Ergot alkaloid biosynthesis in Aspergillus fumigatus : Association with sporulation and clustered genes common among ergot fungi Christine M. Coyle West Virginia University Follow this and additional works at: https://researchrepository.wvu.edu/etd Recommended Citation Coyle, Christine M., "Ergot alkaloid biosynthesis in Aspergillus fumigatus : Association with sporulation and clustered genes common among ergot fungi" (2009). Graduate Theses, Dissertations, and Problem Reports. 4453. https://researchrepository.wvu.edu/etd/4453 This Dissertation is protected by copyright and/or related rights. It has been brought to you by the The Research Repository @ WVU with permission from the rights-holder(s). You are free to use this Dissertation in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you must obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/ or on the work itself. This Dissertation has been accepted for inclusion in WVU Graduate Theses, Dissertations, and Problem Reports collection by an authorized administrator of The Research Repository @ WVU. For more information, please contact [email protected]. Ergot alkaloid biosynthesis in Aspergillus fumigatus: Association with sporulation and clustered genes common among ergot fungi Christine M. Coyle Dissertation submitted to the Davis College of Agriculture, Forestry, and Consumer Sciences at West Virginia University in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Genetics and Developmental Biology Daniel G. Panaccione, Ph.D., Chair Kenneth P. Blemings, Ph.D. Joseph B.