Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pleural Effusion and Ventilation/Perfusion Scan Interpretation for Acute Pulmonary Embolus
ventricular function by radionuclide angiography during exercise in normal subjects 33. Verani MS. Myocardial perfusion imaging versus two-dimensional echocardiography: and patients with chronic coronary heart disease. J Am Coll Cardiol 1983;1:1518- comparative value in the diagnosis of coronary artery disease. J NucÃCardiol 1529. 1994;1:399-414. 29. Adam WE. Tarkowska A, Bitter F, Stauch M, Geffers H. Equilibrium (gated) 34. Foster T, McNeill AJ, Salustri A, et al. Simultaneous dobutamine stress echocardiog radionuclide ventriculography. Cardiovasc Radial 1979;2:161-173. raphy and technetium-99m SPECT in patients with suspected coronary artery disease. 30. Hurwitz RA, TrêvesS, Kuroc A. Right ventricular and left ventricular ejection fraction J Am Coll Cardiol I993;21:1591-I596. in pediatrie patients with normal hearts: first pass radionuclide angiography. Am 35. Marwick TH, D'Hondt AM, Mairesse GH, Baudhuin T, Wijins W, Detry JM, Meiin Heart J 1984;107:726-732. 31. Freeman ML, Palac R, Mason J, et al. A comparison of dobutamine infusion and JA. Comparative ability of dobutamine and exercise stress in inducing myocardial ischemia in active patients. Br Heart J 1994:72:31-38. supine bicycle exercise for radionuclide cardiac stress testing. Clin NucÃMed 1984:9:251-255. 36. Senior R, Sridhara BS, Anagnostou E, Handler C, Raftery EB, Lahiri A. Synergistic 32. Cohen JL, Greene TO, Ottenweller J, Binebaum SZ, Wilchfort SD, Kim CS. value of simultaneous stress dobutamine sestamibi single-photon-emission computer Dobutamine digital echocardiography for detecting coronary artery disease. Am J ized tomography and echocardiography in the detection of coronary artery disease. -

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Allergic Bronchopulmonary Aspergillosis Revealing Asthma
CASE REPORT published: 22 June 2021 doi: 10.3389/fimmu.2021.695954 Case Report: Allergic Bronchopulmonary Aspergillosis Revealing Asthma Houda Snen 1,2*, Aicha Kallel 2,3*, Hana Blibech 1,2, Sana Jemel 2,3, Nozha Ben Salah 1,2, Sonia Marouen 3, Nadia Mehiri 1,2, Slah Belhaj 3, Bechir Louzir 1,2 and Kalthoum Kallel 2,3 1 Pulmonary Department, Hospital Mongi Slim, La Marsa, Tunisia, 2 Faculty of Medicine, Tunis El Manar University, Tunis, Tunisia, 3 Parasitology and Mycology Department, La Rabta Hospital, Tunis, Tunisia Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disorder caused by hypersensitivity to Aspergillus which colonizes the airways of patients with asthma and cystic fibrosis. Its diagnosis could be difficult in some cases due to atypical Edited by: presentations especially when there is no medical history of asthma. Treatment of ABPA is Brian Stephen Eley, frequently associated to side effects but cumulated drug toxicity due to different molecules University of Cape Town, South Africa is rarely reported. An accurate choice among the different available molecules and Reviewed by: effective on ABPA is crucial. We report a case of ABPA in a woman without a known Shivank Singh, Southern Medical University, China history of asthma. She presented an acute bronchitis with wheezing dyspnea leading to an Richard B. Moss, acute respiratory failure. She was hospitalized in the intensive care unit. The Stanford University, United States bronchoscopy revealed a complete obstruction of the left primary bronchus by a sticky *Correspondence: Houda Snen greenish material. The culture of this material isolated Aspergillus fumigatus and that of [email protected] bronchial aspiration fluid isolated Pseudomonas aeruginosa. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -

Rapid and Precise Diagnosis of Pneumonia Coinfected By
Rapid and precise diagnosis of pneumonia coinfected by Pneumocystis jirovecii and Aspergillus fumigatus assisted by next-generation sequencing in a patient with systemic lupus erythematosus: a case report Yili Chen Sun Yat-Sen University Lu Ai Sun Yat-Sen University Yingqun Zhou First Peoples Hospital of Nanning Yating Zhao Sun Yat-Sen University Jianyu Huang Sun Yat-Sen University Wen Tang Sun Yat-Sen University Yujian Liang ( [email protected] ) Sun Yat-Sen University Case report Keywords: Pneumocystis jirovecii, Aspergillus fumigatus, Next generation sequencing, Case report Posted Date: March 19th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-154016/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/12 Abstract Background: Pneumocystis jirovecii and Aspergillus fumigatus, are opportunistic pathogenic fungus that has a major impact on mortality in patients with systemic lupus erythematosus. With the potential to invade multiple organs, early and accurate diagnosis is essential to the survival of SLE patients, establishing an early diagnosis of the infection, especially coinfection by Pneumocystis jirovecii and Aspergillus fumigatus, still remains a great challenge. Case presentation: In this case, we reported that the application of next -generation sequencing in diagnosing Pneumocystis jirovecii and Aspergillus fumigatus coinfection in a Chinese girl with systemic lupus erythematosus (SLE). Voriconazole was used to treat pulmonary aspergillosis, besides sulfamethoxazole and trimethoprim (SMZ-TMP), and caspofungin acetate to treat Pneumocystis jirovecii infection for 6 days. On Day 10 of admission, her chest radiograph displayed obvious absorption of bilateral lung inammation though the circumstance of repeated fever had not improved. -

Central Nervous System Infections by Members of the Pseudallescheria
Review article Central nervous system infections by members of the Pseudallescheria boydii species complex in healthy and immunocompromised hosts: epidemiology, clinical characteristics and outcome A. Serda Kantarcioglu,1 Josep Guarro2 and G. S. de Hoog3 1Department of Microbiology and Clinical Microbiology, Cerrahpasa Medical Faculty, Istanbul, Turkey, 2Unitat de Microbiologia, Facultat de Medicina i Ciencies de la Salut, Universitat Rovira i Virgili, Reus, Spain and 3Centraalbureau voor Schimmelcultures, Utrecht, and Institute for Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands Summary Infections caused by members of the Pseudallescheria boydii species complex are currently among the most common mould infections. These fungi show a particular tropism for the central nervous system (CNS). We reviewed all the available reports on CNS infections, focusing on the geographical distribution, infection routes, immunity status of infected individuals, type and location of infections, clinical manifestations, treatment and outcome. A total of 99 case reports were identified, with similar percentage of healthy and immunocompromised patients (44% vs. 56%; P = 0.26). Main clinical types were brain abscess (69%), co-infection of brain tissue and ⁄ or spinal cord with meninges (10%) and meningitis (9%). The mortality rate was 74%, regardless of the patientÕs immune status, or the infection type and ⁄ or location. Cerebrospinal fluid culture was revealed as a not very important tool as the percentage of positive samples for P. boydii complex was not different from that of negative ones (67% vs. 33%; P = 0.10). In immunocompetent patients, CNS infection was preceded by near drowning or trauma. In these patients, the infection was characterised by localised involvement and a high fatality rate (76%). -

Spontaneous Pneumothorax in COVID-19 Patients Treated with High-Flow Nasal Cannula Outside the ICU: a Case Series
International Journal of Environmental Research and Public Health Case Report Spontaneous Pneumothorax in COVID-19 Patients Treated with High-Flow Nasal Cannula outside the ICU: A Case Series Magdalena Nalewajska 1, Wiktoria Feret 1 , Łukasz Wojczy ´nski 1, Wojciech Witkiewicz 2 , Magda Wi´sniewska 1 and Katarzyna Kotfis 3,* 1 Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70–111 Szczecin, Poland; [email protected] (M.N.); [email protected] (W.F.); [email protected] (Ł.W.); [email protected] (M.W.) 2 Department of Cardiology, Pomeranian Medical University, 70–111 Szczecin, Poland; [email protected] 3 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70–111 Szczecin, Poland * Correspondence: katarzyna.kotfi[email protected] Abstract: The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a global pandemic and a burden to global health at the turn of 2019 and 2020. No targeted treatment for COVID-19 infection has been identified so far, thus supportive treatment, invasive and non-invasive oxygen support, and corticosteroids remain a common therapy. High-flow nasal cannula (HFNC), a non-invasive oxygen support method, has become a prominent treatment option for respiratory failure during the SARS-CoV-2 pandemic. Citation: Nalewajska, M.; Feret, W.; HFNC reduces the anatomic dead space and increases positive end-expiratory pressure (PEEP), Wojczy´nski,Ł.; Witkiewicz, W.; allowing higher concentrations and higher flow of oxygen. Some studies suggest positive effects of Wi´sniewska,M.; Kotfis, K. HFNC on mortality and avoidance of intubation. -

Rhinitis and Sinusitis
Glendale Animal Hospital 623-934-7243 www.familyvet.com Rhinitis and Sinusitis (Inflammation of the Nose and Sinuses) Basics OVERVIEW Rhinitis—inflammation of the lining of the nose Sinusitis—inflammation of the sinuses The nasal cavity communicates directly with the sinuses; thus inflammation of the nose (rhinitis) and inflammation of the sinuses (sinusitis) often occur together (known as “rhinosinusitis”) “Upper respiratory tract” (also known as the “upper airways”) includes the nose, nasal passages, throat (pharynx), and windpipe (trachea) “Lower respiratory tract” (also known as the “lower airways”) includes the bronchi, bronchioles, and alveoli (the terminal portion of the airways, in which oxygen and carbon dioxide are exchanged) SIGNALMENT/DESCRIPTION OF PET Species Dogs Cats Breed Predilections Short-nosed, flat-faced (known as “brachycephalic”) cats are more prone to long-term (chronic) inflammation of the nose (rhinitis), and possibly fungal rhinitis Dogs with a long head and nose (known as “dolichocephalic dogs,” such as the collie and Afghan hound) are more prone to Aspergillus (a type of fungus) infection and nasal tumors Mean Age and Range Cats—sudden (acute) viral inflammation of the nose and sinuses (rhinosinusitis) and red masses in the nasal cavity and throat (known as “nasopharyngeal polyps”) are more common in young kittens (6–12 weeks of age) Congenital (present at birth) diseases (such as cleft palate) are more common in young pets Tumors/cancer and dental disease—are more common in older pets Foreign -

Allergic Bronchopulmonary Aspergillosis As a Cause of Bronchial Asthma in Children
Egypt J Pediatr Allergy Immunol 2012;10(2):95-100. Original article Allergic bronchopulmonary aspergillosis as a cause of bronchial asthma in children Background: Allergic bronchopulmonary aspergillosis (ABPA) occurs in Dina Shokry, patients with asthma and cystic fibrosis. When aspergillus fumigatus spores Ashgan A. are inhaled they grow in bronchial mucous as hyphae. It occurs in non Alghobashy, immunocompromised patients and belongs to the hypersensitivity disorders Heba H. Gawish*, induced by Aspergillus. Objective: To diagnose cases of allergic bronchopulmonary aspergillosis among asthmatic children and define the Manal M. El-Gerby* association between the clinical and laboratory findings of aspergillus fumigatus (AF) and bronchial asthma. Methods: Eighty asthmatic children were recruited in this study and divided into 50 atopic and 30 non-atopic Departments of children. The following were done: skin prick test for aspergillus fumigatus Pediatrics and and other allergens, measurement of serum total IgE, specific serum Clinical Pathology*, aspergillus fumigatus antibody titer IgG and IgE (AF specific IgG and IgE) Faculty of Medicine, and absolute eosinophilic count. Results: ABPA occurred only in atopic Zagazig University, asthmatics, it was more prevalent with decreased forced expiratory volume Egypt. at the first second (FEV1). Prolonged duration of asthma and steroid dependency were associated with ABPA. AF specific IgE and IgG were higher in the atopic group, they were higher in Aspergillus fumigatus skin Correspondence: prick test positive children than negative ones .Wheal diameter of skin prick Dina Shokry, test had a significant relation to the level of AF IgE titer. Skin prick test Department of positive cases for aspergillus fumigatus was observed in 32% of atopic Pediatrics, Faculty of asthmatic children. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

FINAL RISK ASSESSMENT for Aspergillus Niger (February 1997)
ATTACHMENT I--FINAL RISK ASSESSMENT FOR Aspergillus niger (February 1997) I. INTRODUCTION Aspergillus niger is a member of the genus Aspergillus which includes a set of fungi that are generally considered asexual, although perfect forms (forms that reproduce sexually) have been found. Aspergilli are ubiquitous in nature. They are geographically widely distributed, and have been observed in a broad range of habitats because they can colonize a wide variety of substrates. A. niger is commonly found as a saprophyte growing on dead leaves, stored grain, compost piles, and other decaying vegetation. The spores are widespread, and are often associated with organic materials and soil. History of Commercial Use and Products Subject to TSCA Jurisdiction The primary uses of A. niger are for the production of enzymes and organic acids by fermentation. While the foods, for which some of the enzymes may be used in preparation, are not subject to TSCA, these enzymes may have multiple uses, many of which are not regulated except under TSCA. Fermentations to produce these enzymes may be carried out in vessels as large as 100,000 liters (Finkelstein et al., 1989). A. niger is also used to produce organic acids such as citric acid and gluconic acid. The history of safe use for A. niger comes primarily from its use in the food industry for the production of many enzymes such as a-amylase, amyloglucosidase, cellulases, lactase, invertase, pectinases, and acid proteases (Bennett, 1985a; Ward, 1989). In addition, the annual production of citric acid by fermentation is now approximately 350,000 tons, using either A. -
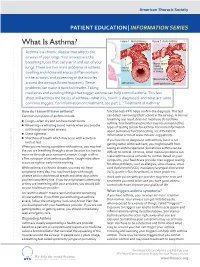
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist.