IHF Annual Report 2012.3.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rte Guide Tv Listings Ten
Rte guide tv listings ten Continue For the radio station RTS, watch Radio RTS 1. RTE1 redirects here. For sister service channel, see Irish television station This article needs additional quotes to check. Please help improve this article by adding quotes to reliable sources. Non-sources of materials can be challenged and removed. Найти источники: РТЗ Один - новости газеты книги ученый JSTOR (March 2020) (Learn how and when to remove this template message) RTÉ One / RTÉ a hAonCountryIrelandBroadcast areaIreland & Northern IrelandWorldwide (online)SloganFuel Your Imagination Stay at home (during the Covid 19 pandemic)HeadquartersDonnybrook, DublinProgrammingLanguage(s)EnglishIrishIrish Sign LanguagePicture format1080i 16:9 (HDTV) (2013–) 576i 16:9 (SDTV) (2005–) 576i 4:3 (SDTV) (1961–2005)Timeshift serviceRTÉ One +1OwnershipOwnerRaidió Teilifís ÉireannKey peopleGeorge Dixon(Channel Controller)Sister channelsRTÉ2RTÉ News NowRTÉjrTRTÉHistoryLaunched31 December 1961Former namesTelefís Éireann (1961–1966) RTÉ (1966–1978) RTÉ 1 (1978–1995)LinksWebsitewww.rte.ie/tv/rteone.htmlAvailabilityTerrestrialSaorviewChannel 1 (HD)Channel 11 (+1)Freeview (Northern Ireland only)Channel 52CableVirgin Media IrelandChannel 101Channel 107 (+1)Channel 135 (HD)Virgin Media UK (Northern Ireland only)Channel 875SatelliteSaorsatChannel 1 (HD)Channel 11 (+1)Sky IrelandChannel 101 (SD/HD)Channel 201 (+1)Channel 801 (SD)Sky UK (Northern Ireland only)Channel 161IPTVEir TVChannel 101Channel 107 (+1)Channel 115 (HD)Streaming mediaVirgin TV AnywhereWatch liveAer TVWatch live (Ireland only)RTÉ PlayerWatch live (Ireland Only / Worldwide - depending on rights) RT'One (Irish : RTH hAon) is the main television channel of the Irish state broadcaster, Raidi'teilif's Siranne (RTW), and it is the most popular and most popular television channel in Ireland. It was launched as Telefes Siranne on December 31, 1961, it was renamed RTH in 1966, and it was renamed RTS 1 after the launch of RTW 2 in 1978. -

Goldsmith Festival 2013 Brochure
OBJECTIVES To develop a deeper insight into the writings of Oliver Goldsmith To promote Goldsmith Country thth as a major tourist attraction 2929 AnnualAnnual For further information please contact: GoldsmithGoldsmith www.goldsmithfestival.ie InternationalInternational Goldsmith Literary Tour LiteraryLiterary FestivalFestival Bus Tour featuring readings from selected works of Goldsmith at well known locations including May 31stst - JuneJune 22nd Forgney Church, Lissoy and Kilkenny West 2013 Beginning at 11.00 am and returning to the Goldsmith Monument, Ballymahon Library Admission €10 GOLDSMITH LITERARY FESTIVAL COMMITTEE Theme: Chairman: Seamus McCormack Secretary: Adrian Duncan Treasurer: Niall Nally The Gathering - Committee: Joe Farrell, William Dowler, Cecil English, Are Faraway Hills Greener ? Teddy McGoey, Sean Ryan, Dr. Pat Kelly, Willie Flanagan, Anne Tully “Such is the patriot’s boast, where’er we roam, Produced with Financial Assistance from His first, best country ever is, at home.” The Traveller (1764)- Oliver Goldsmith Longford County Council Designed and printed by Arthur Conlon, Ballymahon - 086 8716763 st Sally Mulready is an elected Labour Party Councillor in the London Borough of Friday May 31 Rustic Inn, Abbeyshrule Adm. €10 Hackney and was appointed to the Irish Council of State in January 2012 by President Michael D. Higgins. She has a solid history of community politics, long 8.00 pm Recital by Innyside Singers term union involvement and championing human rights in Britain and abroad. She is a founder member, and current Chair, of the Irish Women Survivors Network and 8.30 pm Chair: Ciaran Mullooly is the Director of the Irish Elderly Advice Network, a charity supporting older Irish people living in and around London. -

2019 Press Coverage
Media Appearances 2019 Date Staff Member Radio Subject Link RTE Morning Ireland 02 January 2019 Mindy Recycling Shannonside 03 January 2019 Mindy Single Use Plastic (SUP) EastCoast 03 January 2019 Mindy SUP KFM 03 January 2019 Mindy SUP RTE Morning Ireland 09 January 2019 Mindy Incineration Newstalk Between the Lines 19 January 2019 Mindy Recycling Near FM 23 January 2019 Mindy Plastics Tipp Midwest Joe Pryce 29 January 2019 Mindy Deposit Refund Scheme (DRS) CRC Mayo 29 January 2019 Mindy DRS KFM Ciara Noble 31 January 2019 Mindy DRS KFM 05 February 2019 Mindy DRS Eastcoast FM 12 March 2019 Mindy Disposable Cups RTE 12 March 2019 Sorcha Disposable Cups CRC FM 05 April 2019 Mindy Sick of Plastic Shannonside: Joe Finnegan 11 April 2019 Mindy Lidl Recycling Connemara FM 11 April 2019 Mindy Sick of Plastic Newstalk 12 April 2019 Mindy Plastics Newstalk 13 April 2019 Mindy Sick of Plastic Newstalk 19 April 2019 Mindy Litter Newstalk 22 April 2019 Mindy Waste & recycling Today FM Matt Cooper 09 May 2019 Mindy DRS Connemara FM 09 May 2019 Sorcha Conscious Cup Campaign (CCC) Newstalk Morning show 15 May 2019 Mindy DRS Midlands Radio 17 May 2019 Mindy Litter report Newstalk 17 May 2019 Mindy Litter report Eastcoast Radio 17 May 2019 Mindy Litter report Shannonside 17 May 2019 Mindy Litter report Today FM Matt Cooper 17 May 2019 Mindy Litter report KFM 21 May 2019 Mindy Litter report Flirt FM Galway 21 May 2019 Mindy Litter report Newstalk 22 May 2019 Mindy SUP Today FM Matt Cooper 22 May 2019 Mindy SUP Today FM Matt Cooper 15 July 2019 Mindy Newstalk -

A Protestant Paper for a Protestant People: the Irish Times and the Southern Irish Minority
Irish Communication Review Volume 12 Issue 1 Article 5 January 2010 A Protestant Paper for a Protestant People: The Irish Times and the Southern Irish Minority Ian d’Alton Follow this and additional works at: https://arrow.tudublin.ie/icr Part of the Communication Technology and New Media Commons Recommended Citation d’Alton, Ian (2010) "A Protestant Paper for a Protestant People: The Irish Times and the Southern Irish Minority," Irish Communication Review: Vol. 12: Iss. 1, Article 5. doi:10.21427/D7TT5T Available at: https://arrow.tudublin.ie/icr/vol12/iss1/5 This Article is brought to you for free and open access by the Current Publications at ARROW@TU Dublin. It has been accepted for inclusion in Irish Communication Review by an authorized administrator of ARROW@TU Dublin. For more information, please contact [email protected], [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-Share Alike 4.0 License A PROTESTANT PAPER FOR A PROTESTANT PEOPLE: The Irish Times and the southern Irish minority Ian d’Alton WE IRISH PROTESTANTS have always had a reputation for appreciating the minutiae of social distinction. Often invisible to the outsider, this extended to such as our dogs, our yachts and, of course, our newspapers. My paternal grandmother was no exception. Her take on the relative pecking order of the Irish dailies was that one got one’s news and views from the Irish Times, one lit the fire with the Irish Independent, and as for the Irish Press – ah! Delicacy forbids me to go into details, but suffice it to say that it involved cutting it into appropriate squares, and hanging these in the smallest room of the house! In this paper I set the scene, as it were: to examine those who formed the Times’ perceived audience for much of its existence – Irish Protestants, in particular those who were citizens of the Free State and the early Republic. -

The Role of Irish-Language Film in Irish National Cinema Heather
Finding a Voice: The Role of Irish-Language Film in Irish National Cinema Heather Macdougall A Thesis in the PhD Humanities Program Presented in Partial Fulfillment of the Requirements for the degree of Doctor of Philosophy at Concordia University Montreal, Quebec, Canada August 2012 © Heather Macdougall, 2012 ABSTRACT Finding a Voice: The Role of Irish-Language Film in Irish National Cinema Heather Macdougall, Ph.D. Concordia University, 2012 This dissertation investigates the history of film production in the minority language of Irish Gaelic. The objective is to determine what this history reveals about the changing roles of both the national language and national cinema in Ireland. The study of Irish- language film provides an illustrative and significant example of the participation of a minority perspective within a small national cinema. It is also illustrates the potential role of cinema in language maintenance and revitalization. Research is focused on policies and practices of filmmaking, with additional consideration given to film distribution, exhibition, and reception. Furthermore, films are analysed based on the strategies used by filmmakers to integrate the traditional Irish language with the modern medium of film, as well as their motivations for doing so. Research methods included archival work, textual analysis, personal interviews, and review of scholarly, popular, and trade publications. Case studies are offered on three movements in Irish-language film. First, the Irish- language organization Gael Linn produced documentaries in the 1950s and 1960s that promoted a strongly nationalist version of Irish history while also exacerbating the view of Irish as a “private discourse” of nationalism. Second, independent filmmaker Bob Quinn operated in the Irish-speaking area of Connemara in the 1970s; his fiction films from that era situated the regional affiliations of the language within the national context. -

Page 1 of 125 © 2016 Factiva, Inc. All Rights Reserved. Colin's Monster
Colin's monster munch ............................................................................................................................................. 4 What to watch tonight;Television.............................................................................................................................. 5 What to watch tonight;Television.............................................................................................................................. 6 Kerry's wedding tackle.............................................................................................................................................. 7 Happy Birthday......................................................................................................................................................... 8 Joke of the year;Sun says;Leading Article ............................................................................................................... 9 Atomic quittin' ......................................................................................................................................................... 10 Kerry shows how Katty she really is;Dear Sun;Letter ............................................................................................ 11 Host of stars turn down invites to tacky do............................................................................................................. 12 Satellite & digital;TV week;Television.................................................................................................................... -

The Irish Times - Mon, Sep 29, 2008
Adams directs call for truth commission to republicans - The Irish Times - Mon, Sep 29, 2008 US Elections ● Full coverage of the US Presidential undefined 11 °C Dublin » RSS Feeds Site Index election Ireland World CampaignSunsetThe Irishyear on ofTimes trailthe living property 2008 clock cheaply boomSupplements DenisFrankAUDIOHow to Staunton'sMcDonald liveSLIDESHOW: on just andUS a poundelectionKathy The refurbished aSheridan dayblog In Depth followIrish Times the story clock of has a millionaire been unveiled Ferrari- at Other drivingthe newspaper's property developer office at the junction of Today's Paper Tara Street and Townsend Street in Dublin ● Home » ● Ireland » ● In the North » ADVERTISEMENT ● Email to a friend ● Email to Author ● Print ● RSS ● Text Size: Latest » Monday, September 29, 2008 ● 14:23 Adams directs call for truth commission to republicans Zimbabwe unity government close to formation ● 14:19 Injuries Board says insurance hike not justified ● GERRY MORIARTY 14:11 Irish stocks see sharpest fall in more than 20 years SINN FÉIN president Gerry Adams has called for the creation of an independent international truth commission to deal with the legacy of ● 14:10 the Troubles, in a message directed specifically at Sinn Féin and IRA members. Bush says bailout will 'restore strength' ● 14:01 Mr Adams has used the current edition of the republican weekly newspaper, An Phoblacht to back the setting up of a truth commission. Mr Survey finds 40% favour tax hike to pay for services Adams does not specifically state that the IRA must co-operate with such a body, but it appears implicit in one of the nine principles which ● 14:00 'Sacked' employees hold protest in Dublin Sinn Féin proposes should underpin an "effective truth recovery process". -

S.Macw / CV / NCAD
Susan MacWilliam Curriculum Vitae 1 / 8 http://www.susanmacwilliam.com/ Solo Exhibitions 2012 Out of this Worlds, Noxious Sector Projects, Seattle F-L-A-M-M-A-R-I-O-N, Open Space, Victoria, BC 2010 F-L-A-M-M-A-R-I-O-N, aceart inc, Winnipeg Supersense, Higher Bridges Gallery, Enniskillen Susan MacWilliam, Conner Contemporary, Washington DC F-L-A-M-M-A-R-I-O-N, Golden Thread Gallery, Belfast F-L-A-M-M-A-R-I-O-N, NCAD Gallery, Dublin 2009 Remote Viewing, 53rd Venice Biennale 2009, Solo exhibition representing Northern Ireland 13 Roland Gardens, Golden Thread Gallery Project Space, Belfast 2008 Eileen, Gimpel Fils, London Double Vision, Jack the Pelican Presents, New York 13 Roland Gardens, Video Screening, The Parapsychology Foundation Perspectives Lecture Series, Baruch College, City University, New York 2006 Dermo Optics, Likovni Salon, Celje, Slovenia 2006 Susan MacWilliam, Ard Bia Café, Galway 2004 Headbox, Temple Bar Gallery, Dublin 2003 On The Eye, Golden Thread Gallery, Belfast 2002 On The Eye, Butler Gallery, Kilkenny 2001 Susan MacWilliam, Gallery 1, Cornerhouse, Manchester 2000 The Persistence of Vision, Limerick City Gallery of Art, Limerick 1999 Experiment M, Context Gallery, Derry Faint, Old Museum Arts Centre, Belfast 1997 Curtains, Project Arts Centre, Dublin 1995 Liptych II, Crescent Arts Centre, Belfast 1994 Liptych, Harmony Hill Arts Centre, Lisburn List, Street Level Gallery, Irish News Building, Belfast Solo Screenings 2012 Some Ghosts, Dr William G Roll (1926-2012) Memorial, Rhine Research Center, Durham, NC. 2010 F-L-A-M-M-A-R-I-O-N, Sarah Meltzer Gallery, New York. -

Attitudes and Behaviour in the Second Referendum on the Treaty of Lisbon
Attitudes and Behaviour in the Second Referendum on the Treaty of Lisbon Richard Sinnott and Johan A. Elkink Geary Institute and School of Politics and International Relations University College Dublin Report prepared for the Department of Foreign Affairs July 2010 Introduction Twice within the last decade, Irish government proposals to ratify new EU treaties have been defeated by referendum (the referendum on the Treaty of Nice in 2001 and that on the Treaty of Lisbon in 2008). Both outcomes were reversed in follow-on referendums within a year or so of the defeat. Although the net outcome in each case was that Ireland could proceed to ratify the EU treaties in question, the experience was not one that any Irish government would wish to repeat. In this context, our report on attitudes and behaviour in the first Lisbon referendum concluded by noting the “undeniable need” to address the issue of public support for the process of European integration “not just now and not just in the run-up to a referendum but on an on-going and long-term basis”. 1 Our ability to analyse Irish attitudes to European integration and the behaviour consequent on such attitudes has been significantly enhanced by the decision to conduct a post- referendum poll not just after the 2008 referendum NO but also after the 2009 referendum YES. Beginning with a summary of the main trends in voting in Irish EU referendums, this report analyses the sources of the YES and NO votes and of abstention in the 2009 Lisbon referendum. Fieldwork for the poll was conducted by Millward Brown Lansdowne between 20 th and 23 rd November 2009. -
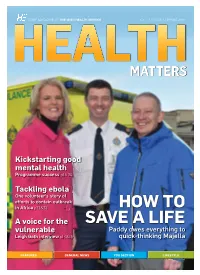
Health Matters Spring 2015
STAFF MAGAZINE OF THE IRISH HEALTH SERVICE VOL. 10 | ISSUE 1 | SPRING 2015 Kickstarting good mental health Programme success p18-20 Tackling ebola One volunteer’s story of efforts to contain outbreak in Africa p22&23 HOW TO A voice for the SAVE A LIFE vulnerable Paddy owes everything to Leigh Gath interview p14&15 quick-thinking Majella FEATURES GENERAL NEWS YOU SECTION LIFESTYLE WELCOME TO THE LATEST EDITION OF HEALTH MATTERS A STAFF magazine would be nothing without the staff itself. These are your stories and we are delighted to be able to shine a light on the many fine initiatives and hard work going on in the HSE around the country. Our cover story of Majella Loftus’s chance encounter with Paddy O’Hara – one that kept him alive until paramedics arrived on the scene to treat his heart attack - should serve as an incentive to any person to acquire the skills that could literally be a life-saver in the future. Congratulations to Debbie O’Reilly, Ireland’s latest boxing titleholder who replaces no less than Olympic gold medal winner Katie Taylor as lightweight champion. Best of luck to her in her future bouts. The HSE can be very proud of the Galway paramedic’s achievements so far. It was also fascinating speaking to Diarmuid O’Donovan and listening to his Lightning Bolts experiences in Africa helping in the battle LimerickLi i k team come thirdhi d ini relayl against the spread of Ebola. And it has certainly been a busy few months within the HSE, with the Little CONTENTS Things, Under the Weather and QUIT campaigns being launched. -

Hearing Women's Voices?
Hearing Women’s Voices? Dr. Kathy Walsh, Exploring women’s underrepresentation Dr. Jane Suiter & in current affairs radio programming at Orla O’Connor peak listening times in Ireland National Womens Council of Ireland Comhairle Náisiúnta Institute for Future na mBan in Éirinn Media & Journalism Published November 2015 by National Women’s Council of Ireland and Dublin City University ISBN 978-0-9926849-4-5 FUNDED BY Hearing Women’s Voices? Exploring women’s underrepresentation in current affairs radio programming at peak listening times in Ireland Dr. Kathy Walsh, Dr. Jane Suiter & Orla O’Connor Acknowledgments National Women’s Council of Ireland and Dublin City University would like to thank the Broadcasting Authority of Ireland for funding this research. We would like to thank Aileen O’Driscoll, Kristy Park and Joe Breen for their work in relation to monitoring the radio programmes. At RTÉ Radio 1 we would like to thank Vincent Murphy and the team at Morning Ireland, Kevin Bakhurst and Tom McGuire for giving their time and for giving us access to the behind the scenes production at Morning Ireland. At Newstalk we would like to thank Garrett Harte, Rebecca Meehan and the team at Newstalk Breakfast for giving us access to the behind the scenes production at Newstalk Breakfast. We would also like to thank Cliona Barnes who put significant work into the establishment and development of this project and Margaret Ward from Clear Ink and founder of Women on Air, for her contribution. Dr Kathy Walsh, Dr Jane Suiter and Orla O’Connor, Director NWCI. Contents 1. -

Heresa Morrow: RTÉ One TV: the Late Late Show: 8Th Jan 2016…………………………….81
Broadcasting Authority of Ireland Broadcasting Complaint Decisions September 2016 Broadcasting Complaint Decisions Contents BAI Complaints Handling Process Page 4 Upheld by the BAI Compliance Committee 26/16 - Mr. Francis Clauson: TV3: ‘The Power to Power Ourselves’ (Advert): 10th Jan 2016………………5 27/16 - Mr. Francis Clauson: RTÉ One TV: ‘The Power to Power Ourselves’ (Advert): 16th Jan 2016….…9 29/16 - Intro Matchmaking: Sunshine 106.8: Two’s Company (Advert):16th Feb 2016…………….………13 Rejected by the BAI Compliance Committee 7/16 - Mr. Brendan Burgess: RTÉ One TV: Ireland’s Great Wealth Divide: 21st Sept 2015……………….16 13/16 - Mr. Martin Hawkes: RTÉ One TV: Prime Time: 3rd Dec 2015……………………………………….23 15/16 - An Taisce: RTÉ One TV: Prime Time: 3rd Dec 2015………………………………………………….28 30/16 - Mr. Pawel Rydzewski: RTÉ One TV: The Late Late Show: 22nd Jan 2016…………………………38 32/16 - Mr Séamus Enright: TV3: TV3 Leaders’ Debate: 11th Feb 2016………………………………….…41 35/16 - Mr. John Flynn: RTÉ One TV: The Late Late Show: 19th Feb 2016…………………………………45 37/16 - Mr. Enda Fanning: RTÉ One TV: The Late Late Show: 19th Feb 2016……………………………48 Rejected by the Executive Complaints Forum 8-10/16 - Mr. Brendan O’ Regan: Newstalk: The Pat Kenny Show: 2nd – 4th Dec 2015……………………52 19/16 - Ms. Patricia Kearney: RTÉ Radio 1: When Dave Met Bob: 29th Dec 2015…………………………58 21/16 – Ms. Mary Jo Gilligan: RTÉ Radio 1: The Ray D’Arcy Show: 14th Nov 2015………………………61 22/16 - Mr. Brendan O’ Regan: Newstalk: Lunchtime: 30th Nov 2015…………………………………….…64 23/16 - Mr. Brendan O’ Regan: Newstalk: The Pat Kenny Show: 1st Dec 2015………………………….…64 25/16 - Mr.