HIP EXAMINATION Bone School @ Bangalore
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Souvenir Programme, This Information Is Correct
1 SUBSPECIALTY INTEREST GROUP MEETINGS At time of printing this souvenir programme, this information is correct. Should there be any last minute changes, please refer to the signage outside each meeting room or enquire at the secretariat counter. SUBSPECIALTY INTEREST GROUP MEETING DATE TIME MEETINGS ROOM ASEAN OA Education Committee 21st May 2015 0830 - 1700hrs Kelantan Room Meeting Hand Subspecialty Interest Group 22nd May 2015 1030 - 1200hrs Pahang Room Foot & Ankle Subspecialty Interest Negeri Sembilan 22nd May 2015 1030 - 1200hrs Group Room Spine Subspecialty Interest Group 22nd May 2015 1130 - 1200hrs Johore Room Negeri Sembilan Paediatrics Subspecialty Interest Group 22nd May 2015 1400 - 1530hrs Room ASEAN OA Council Meeting 22nd May 2015 1400 - 1730hrs Kelantan Room Arthroplasty Subspecialty Interest 22nd May 2015 1600 - 1730hrs Pahang Room Group Negeri Sembilan Trauma Subspecialty Interest Group 22nd May 2015 1600 - 1730hrs Room Oncology Subspecialty Interest Group 23rd May 2015 1030 - 1200hrs Penang Room Sports Subspecialty Interest Group 23rd May 2015 1400 - 1530hrs Johore Room MOA Annual General Meeting 23rd May 2014 1600 - 1730hrs Johore Room 23rd May 2015 0800 - 1730hrs APOA Council Meeting Kelantan Room 24th May 2015 0800 - 1500hrs 2 INDEX PAGE NO. DESCRIPTION 2 Subspecialty Interest Group Meetings Malaysian Orthopaedic Association Office Bearers 4 45th Malaysian Orthopaedic Association Annual Scientific Meeting 2015 Organising Committee Welcome Message from President of Malaysian Orthopaedic Association and 5 Organising -

Neonatal Orthopaedics
NEONATAL ORTHOPAEDICS NEONATAL ORTHOPAEDICS Second Edition N De Mazumder MBBS MS Ex-Professor and Head Department of Orthopaedics Ramakrishna Mission Seva Pratishthan Vivekananda Institute of Medical Sciences Kolkata, West Bengal, India Visiting Surgeon Department of Orthopaedics Chittaranjan Sishu Sadan Kolkata, West Bengal, India Ex-President West Bengal Orthopaedic Association (A Chapter of Indian Orthopaedic Association) Kolkata, West Bengal, India Consultant Orthopaedic Surgeon Park Children’s Centre Kolkata, West Bengal, India Foreword AK Das ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD. New Delhi • London • Philadelphia • Panama (021)66485438 66485457 www.ketabpezeshki.com ® Jaypee Brothers Medical Publishers (P) Ltd. Headquarters Jaypee Brothers Medical Publishers (P) Ltd. 4838/24, Ansari Road, Daryaganj New Delhi 110 002, India Phone: +91-11-43574357 Fax: +91-11-43574314 Email: [email protected] Overseas Offices J.P. Medical Ltd. Jaypee-Highlights Medical Publishers Inc. Jaypee Brothers Medical Publishers Ltd. 83, Victoria Street, London City of Knowledge, Bld. 237, Clayton The Bourse SW1H 0HW (UK) Panama City, Panama 111, South Independence Mall East Phone: +44-2031708910 Phone: +507-301-0496 Suite 835, Philadelphia, PA 19106, USA Fax: +02-03-0086180 Fax: +507-301-0499 Phone: +267-519-9789 Email: [email protected] Email: [email protected] Email: [email protected] Jaypee Brothers Medical Publishers (P) Ltd. Jaypee Brothers Medical Publishers (P) Ltd. 17/1-B, Babar Road, Block-B, Shaymali Shorakhute, Kathmandu Mohammadpur, Dhaka-1207 Nepal Bangladesh Phone: +00977-9841528578 Mobile: +08801912003485 Email: [email protected] Email: [email protected] Website: www.jaypeebrothers.com Website: www.jaypeedigital.com © 2013, Jaypee Brothers Medical Publishers All rights reserved. No part of this book may be reproduced in any form or by any means without the prior permission of the publisher. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

SIMMONDS TEST: Patient Is Prone Doctor Flexes the Patients Knee to 90 Degrees Doctor Squeezes the Patient’S Calf
Clinical Orthopedic Testing Review SIMMONDS TEST: Patient is prone Doctor flexes the patients knee to 90 degrees Doctor squeezes the patient’s calf. Classical response: Failure of ankle plantarflexion Classical Importance= torn Achilles tendon Test is done bilaterally ACHILLES TAP: Patient is prone Doctor flexes the patient’s knee to 90 degree Doctor dorsiflexes the ankle and then strikes the Achilles tendon with a percussion hammer Classical response: Plantar response Classical Importance= Intact Achilles tendon Test is done bilaterally FOOT DRAWER TEST: Patient is supine with their ankles off the edge of the examination table Doctor grasps the heel of the ankle being tested with one hand and the tibia just above the ankle with the other. Doctor applies and anterior to posterior and then a posterior to anterior sheer force. Classical response: Anterior or posterior translation of the ankle Classical Importance= Anterior talofibular or posterior talofibular ligament laxity. Test is done bilaterally LATERAL STABILITY TEST: Patient is supine Doctor grasps the tibia with one hand and the foot with the other. Doctor rotates the foot into inversion Classical response: Excessive inversion Classical Importance= Anterior talofibular ligament sprain Test is done bilaterally MEDIAL STABILITY TEST: Patient is supine Doctor grasps the tibia with one hand and the foot with the other Doctor rotates the foot into eversion Classical response: Excessive eversion Classical Importance= Deltoid ligament sprain Test is done bilaterally 1 Clinical Orthopedic Testing Review KLEIGER’S TEST: Patient is seated with the legs and feet dangling off the edge of the examination table. Doctor grasps the patient’s foot while stabilizing the tibia with the other hand Doctor pulls the ankle laterally. -

Sacroiliac Joint N Ischium N Ilium N Pubis James R
Pelvic Anatomy Evidence-Based Evaluation & Treatment n Innominates of the Sacroiliac Joint n ischium n ilium n pubis James R. Scifers, DScPT, LAT, ATC Moravian College n Sacrum Athletic Training Program Articulations Biomechanics of the Pelvis n Function of the SI Joint n transmit vertical forces n Sacroiliac Joints n transmit ground n Pubic Symphysis reaction forces n Lumbo-Sacral Joint Sacral Motions Arthrokinematics of the SI Joint n During trunk flexion… n Sacral Base (S1) n Initially, sacral flexion occurs (base of sacrum n Sacral Apex (S5) moves anterior) n Flexion (nutation) n Later, sacral extension occurs with continued trunk flexion (base of sacrum moves posterior) n occurs during exhalation n Extension (counternutation) n occurs during inhalation 1 Dysfunction Classification Ilio-Sacral (IS) Dysfunctions n Sacroiliac Joint (SIJ) n Named for motion at n Any injury to SIJ PSIS n Ilio-Sacral (IS) n anterior rotation n ilium (innominate) n posterior rotation moving on sacrum n up-slip n Sacro-Iliac (SI) n down-slip (rare) n sacrum moving on ilium n in-flare n Pubic Shear n out-flare n Pubic symphysis / Pubic shear lesion Sacro-Iliac (SI) Dysfunctions Pubic Shear Lesions n Sacral Rotations n Named for “direction facing on axis” n Named for any movement at pubic n Forward Rotations symphysis n right on right n Indicates injury to pubic n left on left symphysis n Backward Rotations n right on left n left on right SI Evaluation Evidence-Based Practice (EBP) n Reliability (k) is reproducibility of test results, can be n History* intra-tester (within one clinician) or inter-tester (between n Observation** multiple clinicians) n Palpation** n Sensitivity (sens) is the ability of test to RULE OUT a condition. -

Musculoskeletal Clinical Vignettes a Case Based Text
Leading the world to better health MUSCULOSKELETAL CLINICAL VIGNETTES A CASE BASED TEXT Department of Orthopaedic Surgery, RCSI Department of General Practice, RCSI Department of Rheumatology, Beaumont Hospital O’Byrne J, Downey R, Feeley R, Kelly M, Tiedt L, O’Byrne J, Murphy M, Stuart E, Kearns G. (2019) Musculoskeletal clinical vignettes: a case based text. Dublin, Ireland: RCSI. ISBN: 978-0-9926911-8-9 Image attribution: istock.com/mashuk CC Licence by NC-SA MUSCULOSKELETAL CLINICAL VIGNETTES Incorporating history, examination, investigations and management of commonly presenting musculoskeletal conditions 1131 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey Prof. John O'Byrne Mr. Iain Feeley Dr. Richie Downey Dr. Martin Kelly Mr. Iain Feeley Dr. Lauren Tiedt Dr. Martin Kelly Department of General Practice, RCSI Dr. Lauren Tiedt Dr. Mark Murphy Department of General Practice, RCSI Dr Ellen Stuart Dr. Mark Murphy Department of Rheumatology, Beaumont Hospital Dr Ellen Stuart Dr Grainne Kearns Department of Rheumatology, Beaumont Hospital Dr Grainne Kearns 2 2 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey TABLE OF CONTENTS Prof. John O'Byrne Mr. Iain Feeley Introduction ............................................................. 5 Dr. Richie Downey Dr. Martin Kelly General guidelines for musculoskeletal physical Mr. Iain Feeley examination of all joints .................................................. 6 Dr. Lauren Tiedt Dr. Martin Kelly Upper limb ............................................................. 10 Department of General Practice, RCSI Example of an upper limb joint examination ................. 11 Dr. Lauren Tiedt Shoulder osteoarthritis ................................................. 13 Dr. Mark Murphy Adhesive capsulitis (frozen shoulder) ............................ 16 Department of General Practice, RCSI Dr Ellen Stuart Shoulder rotator cuff pathology ................................... -

Mcmaster Musculoskeletal Clinical Skills Manual 1E
McMaster Musculoskeletal Clinical Skills Manual Authors Samyuktha Adiga Dr. Raj Carmona, MBBS, FRCPC Illustrator Jenna Rebelo Editors Caitlin Lees Dr. Raj Carmona, MBBS, FRCPC In association with the Medical Education Interest Group Narendra Singh and Jacqueline Ho (co-chairs) FOREWORD AND ACKNOWLEDGEMENTS The McMaster Musculoskeletal Clinical Skills Manual was produced by members of the Medical Education Interest Group (co-chairs Jacqueline Ho and Narendra Singh), and Dr. Raj Carmona, Assistant Professor of Medicine at McMaster University. Samyuktha Adiga and Dr. Carmona wrote the manual. Illustrations were done by Jenna Rebelo. Editing was performed by Caitlin Lees and Dr. Carmona. The Manual, completed in August 2012, is a supplement to the McMaster MSK Examination Video Series created by Dr. Carmona, and closely follows the format and content of these videos. The videos are available on Medportal (McMaster students), and also publicly accessible at RheumTutor.com and fhs.mcmaster.ca/medicine/rheumatology. McMaster Musculoskeletal Clinical Skills Manual S. Adiga, J. Rebelo, C. Lees, R. Carmona McMaster Musculoskeletal Clinical Skills Manual TABLE OF CONTENTS General Guide 1 Hip Examination 3 Knee Examination 6 Ankle and Foot Examination 12 Examination of the Back 15 Shoulder Examination 19 Elbow Examination 24 Hand and Wrist Examination 26 Appendix: Neurological Assessment 29 1 GENERAL GUIDE (Please see videos for detailed demonstration of examinations) Always wash your hands and then introduce yourself to the patient. As with any other exam, ensure adequate exposure while respecting patient's modesty. Remember to assess gait whenever doing an examination of the back or any part of the lower limbs. Inspection follows the format: ● S welling ● E rythema ● A trophy ● D eformities ● S cars, skin changes, etc. -

Mcqs and Emqs in Surgery
1 The metabolic response to injury Multiple choice questions ➜ Homeostasis B Every endocrine gland plays an equal 1. Which of the following statements part. about homeostasis are false? C They produce a model of several phases. A It is defined as a stable state of the D The phases occur over several days. normal body. E They help in the process of repair. B The central nervous system, heart, lungs, ➜ kidneys and spleen are the essential The recovery process organs that maintain homeostasis at a 4. With regard to the recovery process, normal level. identify the statements that are true. C Elective surgery should cause little A All tissues are catabolic, resulting in repair disturbance to homeostasis. at an equal pace. D Emergency surgery should cause little B Catabolism results in muscle wasting. disturbance to homeostasis. C There is alteration in muscle protein E Return to normal homeostasis after breakdown. an operation would depend upon the D Hyperalimentation helps in recovery. presence of co-morbid conditions. E There is insulin resistance. ➜ Stress response ➜ Optimal perioperative care 2. In stress response, which of the 5. Which of the following statements are following statements are false? true for optimal perioperative care? A It is graded. A Volume loss should be promptly treated B Metabolism and nitrogen excretion are by large intravenous (IV) infusions of related to the degree of stress. fluid. C In such a situation there are B Hypothermia and pain are to be avoided. physiological, metabolic and C Starvation needs to be combated. immunological changes. D Avoid immobility. D The changes cannot be modified. -

Common Causes of Hip Pain
Common Causes of Hip Pain • Osteoarthritis • Osteonecrosis Physical Examination of the Hip • Sciatica • Stress Fracture • Infection • Impingement / labral tear • Trochanteric Bursitis • IT Band Pathology Physical Exam 1. Gait analysis 2. Examination Standing • Hip / spinal alignment • Crouch may be hip contracture Gait Analysis 3. Examination Supine • Palpation • Range-of-motion • Strength testing • Distal pulses 4. Provocative maneuvers Pathologic Gait Antalgic: Shortened stance on painful side Steppage: Leg lifts higher to clear ground Waddling: Broad-based, pelvis drops towards raised leg during swing . proximal myopathy Trandelenburg: Trunk towards weak side during stance . abductor weakness Look at posture…leaning forward might be spine Steppage gait . Antalgic gait . - Compensatory for foot drop - “Limping” - Exaggerated hip flexion - Shortened stance allows foot on weak side to clear ground phase on painful / - Tibialis anterior weakness affected limb -RX: • AFO brace, • Refer, especially if acute Trandelenburg gait . - Weak abductors - Superior gluteal nerve - Prior hip surgery Exam Standing . - Walk around the patient - Overall posture - Pelvic tilt Exam Standing • Scoliosis • Leg length discrepancy - Crouch • Hip contracture • Spinal hyperlordosis - Adductor contracture Exam Supine . - Palpation… • know your anatomy / landmarks - Range of motion . Exam Supine • Flexion: 110 - 120° • Extension: 10 - 15° • IR/ER: 30 - 40° / 40 – 60° - Strength and sensation testing - Don’t forget distal pulses Exam Supine . Exam Supine . - Inspection -

Spine to Move Mobile Lumbar Spine 7) Cauda Equina Syndrome
13rd EDITION by Anika A Alhambra PERIPHERAL NERVE INJURY SEDDON classification: I. NEUROPRAXIA. − Transient disorder (spontan recovery), several weeks. − EMG of the distal lession usually normal. − Caused by mechanical pressure, exp: − Crutch paralysis − Good prognosis. II. AXONOTMESIS − A discontinuity of the axon, with intact endoneurium. − Wallerian degenration on the distal side. − There is an axon regeneration : 1 – 3 mm/day − Good prognosis III. NEUROTMESIS − Nerve trunk has distrupted, include endoneural tube − Regeneration process Æ neuroma − Prognosis: depend on the surgery technique. SUNDERLAND Classifications: I. Loss of axonal conduction. II. Loss of continuity of the axon, with intact endoneurium. III. Transection of nerve fiber (axon & sheath), with intact perineurium. IV. Loss of perineurium and fascicular continuity. V. Loss of continuity of entire nerve trunk. DEGREE DISCONTINUITY DAMAGE TREATMENT PROGNOSIS 1st None, conduction block Distal nerve fibers Observation Excellent (neuroprxia) remain intact 2nd Axon (axonotmesis) Based on fibrosis Observation Good 3rd Axon & endoneurium Based on fibrosis Lysis Ok 4th Axon, Fibrotic Nerve graft Marginal endoneurium,perineurium connective tissue connects 5th Complete (neurotmesis) Complete Graft/transfer Poor PATOPHYSIOLOGY on the nerve compression injury: 23rd EDITION by Anika A Alhambra 1. Disturb to microcirculation Æ ischemia 2. Disturb to axoplasmic transport Æ neruroaxonal transport Intravascular edema (Increase of vascular permeability) (Degeneration process) Proliferating fibroblast Separation nerve fiber One week (Demyelination) Note: compression 20-30 mmHg Æ pathology on epineurium >80 mmHg Æ completely stop 30 mmHg (8j); 50 mmHg (2j) Æ reverse after 24 hours 400 mmHg (2j) Æ reverse after 1 week ‘Tinnel sign’, is happened on injury and compression, it is sign of regeneration process (continuity sign) Pathological changes on ‘PRIMARY NERVE REPAIR’ 1. -

Leg Length Discrepancy
Gait and Posture 15 (2002) 195–206 www.elsevier.com/locate/gaitpost Review Leg length discrepancy Burke Gurney * Di6ision of Physical Therapy, School of Medicine, Uni6ersity of New Mexico, Health Sciences and Ser6ices, Boule6ard 204, Albuquerque, NM 87131-5661, USA Received 22 August 2000; received in revised form 1 February 2001; accepted 16 April 2001 Abstract The role of leg length discrepancy (LLD) both as a biomechanical impediment and a predisposing factor for associated musculoskeletal disorders has been a source of controversy for some time. LLD has been implicated in affecting gait and running mechanics and economy, standing posture, postural sway, as well as increased incidence of scoliosis, low back pain, osteoarthritis of the hip and spine, aseptic loosening of hip prosthesis, and lower extremity stress fractures. Authors disagree on the extent (if any) to which LLD causes these problems, and what magnitude of LLD is necessary to generate these problems. This paper represents an overview of the classification and etiology of LLD, the controversy of several measurement and treatment protocols, and a consolidation of research addressing the role of LLD on standing posture, standing balance, gait, running, and various pathological conditions. Finally, this paper will attempt to generalize findings regarding indications of treatment for specific populations. © 2002 Elsevier Science B.V. All rights reserved. Keywords: Leg length discrepancy; Low back pain; Osteoarthritis 1. Introduction LLD (FLLD) defined as those that are a result of altered mechanics of the lower extremities [12]. In addi- Limb length discrepancy, or anisomelia, is defined as tion, persons with LLD can be classified into two a condition in which paired limbs are noticeably un- categories, those who have had LLD since childhood, equal. -
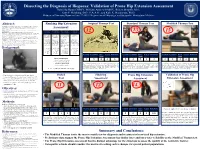
Prone Hip Extension Assessment Gabriella Baran OMSIV, William Andrew OMSIV, Robert Murphy, M.S., Kurt P
Dissecting the Diagnosis of Iliopsoas: Validation of Prone Hip Extension Assessment Gabriella Baran OMSIV, William Andrew OMSIV, Robert Murphy, M.S., Kurt P. Heinking, D.O., F.A.A.O., and Kyle K. Henderson, Ph.D. Midwestern University, Downers Grove, IL60515; Departments of Physiology, and Osteopathic Manipulative Medicine Abstract: Ranking Hip Extension Original Thomas Test Standard Thomas Test Modified Thomas Test Introduction: The father of British Orthopaedic surgery, Hugh Owen Thomas, is recognized for his method to assess hip flexion contracture in patients with Potts disease. The “Thomas Test” was modified to assess the iliopsoas muscle in healthy patients. In Osteopathic medical schools, prone hip extension is also used to Assessment: appreciate a palpable barrier. Objective: Provide historical context for hip extension assessment for medical education and validate prone hip extension assessment. 13 Versatility Specialization Muscle Groups Accuracy Methods: IRB approval was obtained (MWU#2852) and subjects assessed with the Modified- 12 15 Thomas Test (MTT), prone hip extension, and other structural examinations: pelvic side shift, leg length, lumbar curve, seated and standing flexion tests. A digital goniometer and force plate transducer were used to assess Applicability to Applicability to a # of muscle groups Diagnosis prone hip range of motion (ROM) and physician applied force. Results: The MTT, utilizing gravity as the force for hip extension, had high intra-rater reliability (0.969). different patient specific patient assessed and/or ability consistency: Preliminary data for prone hip extension assessment had high intra-rater reliability for ROM (0.973) and the populations: population: to treat: force required to reach the perceived restrictive barrier (0.928).