Lateral Lengthening and Lateral Release Hailey P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Carpal-Instability-Slide-Summary.Pdf
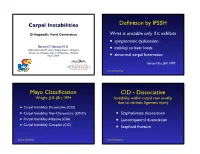
Carpal Instabilities Definition by IFSSH Orthopaedic Hand Conference Wrist is unstable only if it exhibits • symptomatic dysfunction Bernard F. Hearon, M.D. inability to bear loads Clinical Assistant Professor, Department of Surgery • University of Kansas School of Medicine - Wichita May 7, 2019 • abnormal carpal kinematics Garcia-Elias, JHS 1999 Carpal Instability Mayo Classification CID - Dissociative Wright, JHS (Br) 1994 Instability within carpal row usually due to intrinsic ligament injury • Carpal Instability Dissociative (CID) • Carpal Instability Non-Dissociative (CIND) • Scapholunate dissociation • Carpal Instability Adaptive (CIA) • Lunotriquetral dissociation • Carpal Instability Complex (CIC) • Scaphoid fracture Carpal Instability Carpal Instability CIND - Nondissociative Instability between carpal rows due CIA - Adaptive to extrinsic ligament injury Extra-carpal derangement causing carpal malalignment • CIND - Volar Intercalated Segment Instability (VISI) Midcarpal instability caused by malunited • CIND - Dorsal Intercalated fractures of the distal radius Segment Instability (DISI) Taleisnik, JHS 1984 • Combined CIND Carpal Instability Carpal Instability CIC - Complex Instability patterns with qualities of both CID and CIND patterns • Dorsal perilunate dislocations (lesser arc) Perilunate • Dorsal perilunate fracture-dislocations (greater arc injuries) Instability • Volar perilunate dislocations • Axial dislocations, fracture-dislocations Carpal Instability Carpal Instability Perilunate Dislocations Mayfield Classification Progressive -

Disorders of the Knee
DisordersDisorders ofof thethe KneeKnee PainPain Swelling,Swelling, effusioneffusion oror hemarthrosishemarthrosis LimitedLimited jointjoint motionmotion Screw home mechanism – pain, stiffness, fluid, muscular weakness, locking InstabilityInstability – giving way, laxity DeformityDeformity References: 1. Canale ST. Campbell’s operative orthopaedics. 10th edition 2003 Mosby, Inc. 2. Netter FH. The Netter collection of Medical illustrations – musculoskeletal system, Part I & II. 1997 Novartis Pharmaceuticals Corporation. 3. Magee DJ. Orthopedic Physical assessment. 2nd edition 1992 W. B. Saunders Company. 4. Hoppenfeld S. Physical examination of the spine and extremities. 1976 Appleton-century-crofts. AnteriorAnterior CruciateCruciate LigamentLigament Tibial insertion – broad, irregular, diamond-shaped area located directly in front of the intercondylar eminence Femoral attachment Femoral attachment Figure 43-24 In addition to their – semicircular area on the posteromedial synergistic functions, cruciate aspect of the lateral condyle and collateral ligaments exercise 33 mm in length basic antagonistic function 11 mm in diameter during rotation. A, In external Anteromedial bundle — tight in flexion rotation it is collateral ligaments that tighten and inhibit excessive Posterolateral bundle — tight in extension rotation by becoming crossed in 90% type I collagen space. B, In neutral rotation none 10% type III collagen of the four ligaments is under unusual tension. C, In internal Middle geniculate artery rotation collateral ligaments Fat -

Analysis of Rehabilitation Procedure Following Arthroplasty of the Knee with the Use of Complete Endoprosthesis
© Med Sci Monit, 2011; 17(3): CR165-168 WWW.MEDSCIMONIT.COM PMID: 21358604 Clinical Research CR Received: 2010.10.01 Accepted: 2010.12.23 Analysis of rehabilitation procedure following Published: 2011.03.01 arthroplasty of the knee with the use of complete endoprosthesis Authors’ Contribution: Magdalena Wilk-Frańczuk¹,²ACDEF, Wiesław Tomaszewski3ACDEF, Jerzy Zemła²ABDEF, A Study Design Henryk Noga4DEF, Andrzej Czamara3ADEF B Data Collection C Statistical Analysis 1 Andrzej Frycz Modrzewski Cracow University, Cracow, Poland D Data Interpretation 2 Cracow Rehabilitation Centre, Cracow, Poland E Manuscript Preparation 3 College of Physiotherapy, Wroclaw, Poland F Literature Search 4 Endoscopic Surgery Clinic and Sport Clinic Żory, Żory, Poland G Funds Collection Source of support: Departmental sources Summary Background: The use of endoprosthesis in arthroplasty requires adaptation of rehabilitation procedures in or- der to reinstate the correct model of gait, which enables the patient to recover independence and full functionality in everyday life, which in turn results in an improvement in the quality of life. Material/Methods: We studied 33 patients following an initial total arthroplasty of the knee involving endoprosthesis. The patients were divided into two groups according to age. The range of movement within the knee joints was measured for all patients, along with muscle strength and the subjective sensation of pain on a VAS, and the time required to complete the ‘up and go’ test was measured. The gait model and movement ability were evaluated. The testing was conducted at baseline and after com- pletion of the rehabilitation exercise cycle. Results: No significant differences were noted between the groups in the tests of the range of movement in the operated joint or muscle strength acting on the knee joint. -

Knee Pain in Children: Part I: Evaluation
Knee Pain in Children: Part I: Evaluation Michael Wolf, MD* *Pediatrics and Orthopedic Surgery, St Christopher’s Hospital for Children, Philadelphia, PA. Practice Gap Clinicians who evaluate knee pain must understand how the history and physical examination findings direct the diagnostic process and subsequent management. Objectives After reading this article, the reader should be able to: 1. Obtain an appropriate history and perform a thorough physical examination of a patient presenting with knee pain. 2. Employ an algorithm based on history and physical findings to direct further evaluation and management. HISTORY Obtaining a thorough patient history is crucial in identifying the cause of knee pain in a child (Table). For example, a history of significant swelling without trauma suggests bacterial infection, inflammatory conditions, or less likely, intra- articular derangement. A history of swelling after trauma is concerning for potential intra-articular derangement. A report of warmth or erythema merits consideration of bacterial in- fection or inflammatory conditions, and mechanical symptoms (eg, lock- ing, catching, instability) should prompt consideration of intra-articular derangement. Nighttime pain and systemic symptoms (eg, fever, sweats, night sweats, anorexia, malaise, fatigue, weight loss) are associated with bacterial infections, inflammatory conditions, benign and malignant musculoskeletal tumors, and other systemic malignancies. A history of rash or known systemic inflammatory conditions, such as systemic lupus erythematosus or inflammatory bowel disease, should raise suspicion for inflammatory arthritis. Ascertaining the location of the pain also can aid in determining the cause of knee pain. Anterior pain suggests patellofemoral syndrome or instability, quad- riceps or patellar tendinopathy, prepatellar bursitis, or apophysitis (patellar or tibial tubercle). -

Clinical Examination of the Wrist TERRI M
Clinical Examination of the Wrist TERRI M. SKIRVEN, OTR/L, CHT AND A. LEE OSTERMAN, MD HISTORY OF THE INJURY OR ONSET PHYSICAL EXAMINATION INSPECTION OF THE WRIST GENERAL TESTS OBJECTIVE ASSESSMENTS SUMMARY DIAGNOSTIC INJECTION CRITICAL POINTS The wrist is a highly complex joint in a very compact space . Successful clinical evaluation of the wrist requires a 1. Successful clinical examination of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and thorough knowledge of wrist anatomy, biomechanics, pathology. Also required is knowledge of surface anatomy and pathology . and the corresponding underlying structures . The keys to a 2. The wrist examination includes a complete history, successful examination are to link the symptoms with the visual inspection, objective assessments, and a underlying palpable structures and to correlate the mecha- systematic physical examination, including palpation nism of the injury with the physical findings . Some common and provocative testing . conditions may be easily identified on the basis of the clinical 3. The keys to a successful examination are to link the examination, whereas others may require additional diagnos- symptoms with the underlying palpable structures and tic studies, imaging, and repeat evaluations . to correlate the mechanism of the injury with the The components of the wrist examination include a thor- physical findings . ough history, visual inspection, objective assessments, and a 4. Before the wrist is examined, a careful inspection of the systematic physical examination, including palpation and entire upper extremity should be performed to rule out provocative testing to identify tenderness and abnormal other extrinsic and more proximal causes for the wrist motion between bones. -

Spine to Move Mobile Lumbar Spine 7) Cauda Equina Syndrome
13rd EDITION by Anika A Alhambra PERIPHERAL NERVE INJURY SEDDON classification: I. NEUROPRAXIA. − Transient disorder (spontan recovery), several weeks. − EMG of the distal lession usually normal. − Caused by mechanical pressure, exp: − Crutch paralysis − Good prognosis. II. AXONOTMESIS − A discontinuity of the axon, with intact endoneurium. − Wallerian degenration on the distal side. − There is an axon regeneration : 1 – 3 mm/day − Good prognosis III. NEUROTMESIS − Nerve trunk has distrupted, include endoneural tube − Regeneration process Æ neuroma − Prognosis: depend on the surgery technique. SUNDERLAND Classifications: I. Loss of axonal conduction. II. Loss of continuity of the axon, with intact endoneurium. III. Transection of nerve fiber (axon & sheath), with intact perineurium. IV. Loss of perineurium and fascicular continuity. V. Loss of continuity of entire nerve trunk. DEGREE DISCONTINUITY DAMAGE TREATMENT PROGNOSIS 1st None, conduction block Distal nerve fibers Observation Excellent (neuroprxia) remain intact 2nd Axon (axonotmesis) Based on fibrosis Observation Good 3rd Axon & endoneurium Based on fibrosis Lysis Ok 4th Axon, Fibrotic Nerve graft Marginal endoneurium,perineurium connective tissue connects 5th Complete (neurotmesis) Complete Graft/transfer Poor PATOPHYSIOLOGY on the nerve compression injury: 23rd EDITION by Anika A Alhambra 1. Disturb to microcirculation Æ ischemia 2. Disturb to axoplasmic transport Æ neruroaxonal transport Intravascular edema (Increase of vascular permeability) (Degeneration process) Proliferating fibroblast Separation nerve fiber One week (Demyelination) Note: compression 20-30 mmHg Æ pathology on epineurium >80 mmHg Æ completely stop 30 mmHg (8j); 50 mmHg (2j) Æ reverse after 24 hours 400 mmHg (2j) Æ reverse after 1 week ‘Tinnel sign’, is happened on injury and compression, it is sign of regeneration process (continuity sign) Pathological changes on ‘PRIMARY NERVE REPAIR’ 1. -

Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee
To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. S E C T I O N X Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee 31-1 Author: Noyes; Noyes_Section X_main.indd 1 9/23/2015 5:53:34 PM To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. 31 c00031 Knee Articular Cartilage Restoration Procedures Joshua D. Harris, MD, Brian J. Cole, MD, MBA OUTLINE u0010 Indications, 31-2 Preoperative Planning, 31-7 u0045 u0015 Contraindications, 31-4 Intraoperative Evaluation and Operative Technique, 31-8 u0050 u0020 Clinical Biomechanics, 31-4 Clinical Outcomes, 31-9 u0055 u0025 Clinical Evaluation, 31-5 u0030 History, 31-5 u0035 Physical Examination, 31-6 u0040 Diagnostic Tests, 31-7 Once the determination that a defect is symptomatic has p0120 s0010 INDICATIONS been made, conservative treatment options may commence. These Management of symptomatic focal chondral and osteochondral include, but are not limited to, rest, activity modification (typically defects in the knee is complex and multifactorial. -

Knee Injury Medical Treatment Guidelines©
Knee Injury Medical Treatment Guidelines© Proposed by the State of New York Department of Insurance to the Workers’ Compensation Board ©Algorithm 1 and Tables 1 and 2 are taken from the Occupational Medicine Practice Guidelines, 2nd Edition: Knee Complaints published and copyrighted by the American College of Occupational and Environmental Medicine. Copyright 2008, 2007, 2004, 1997 by the American College of Occupational and Environmental Medicine (ACOEM). Commercial reproduction or other use beyond fair use prohibited without explicit ACOEM permission. The American College of Occupational and Environmental Medicine has granted the Workers’ Compensation Board permission to publish Algorithm 1 and Tables 1 and 2 of the Occupational Medicine Practice Guidelines, 2nd Edition: Knee Complaints in connection with the adoption of the New York Knee Injury Medical Treatment Guidelines, including making this guideline available in print and on its website for informational and educational purposes. Use of Algorithm 1 and Tables 1 and 2 of this guideline beyond fair use or for commercial purpose, or both may only occur upon receipt of explicit permission from ACOEM. December 2007 Draft Knee Injury Medical Treatment Guidelines TABLE OF CONTENTS SECTION DESCRIPTION PAGE A. INITIAL DIAGNOSTIC PROCEDURES............................................................ 1. HISTORY-TAKING AND PHYSICIAL EXAMINATION (Hx & PE) .......... a. History of Present Injury ......................................................................... b. Past History ........................................................................................... -

Grafts in Rhinoplasty
Al - Azhar University Center for Virus Studies and Research Grafts in Rhinoplasty Mohamed Rashad Abdel-Hady1, Olfat Abdel-Aziz Sayed2 and Khaled Mohamed Ahmed Abdel-Rahman3 [email protected], [email protected] and [email protected] 1. Prof. of Otolaryngology, Faculty of medicine, Al-Azhar University. 2. Ass.Prof. of Otolaryngology, Faculty of medicine, Al- Azhar University. 3 Specialist of otolaryngology, Helwan University Hospital. Abstract Old rhinoplasty practice has been often relied on resection of the nasal framework in order to achieve aesthetic and/ or functional objectives. Nowadays, careful dissection, conservative resection, planned framework remodeling, & judicious use of properly selected grafts for augmentation comprise the basis for a structural approach to grafting in rhinoplasty. Aim of the work is to present and evaluate outcomes of using grafts in rhinoplasty. Grafts types, techniques were reviewed. Complications, if encountered, were mentioned. Patient satisfaction was evaluated. Methodology is a prospective study utilized the open rhinoplasty technique, upon 35 patients that suffered from various nasal deformities. Their ages ranged between 18 and 45 years. The followed principles consisted of: 1) A precise definition of the type and cause of abnormality. 2) Definition of the goals. 3) Adequate exposure. 4) Preservation or restoration of normal anatomy 5) Incremental and planned correction. 6) Maintenance of nasal airway. Results are 35 patients operated by the open technique, 23 were males while 12 were females. Of them, 32 cases were fully corrected while, 3 cases were partially corrected. Complications were minimal, occurred in 3 cases. The majority of cases (32 cases) were satisfied while 3 cases were unsatisfied. -

Upper Extremity CT CG
AmeriHealth Caritas Louisiana National Imaging Associates, Inc.* Clinical guidelines Original Date: September 1997 UPPER EXTREMITY CT (Hand, Wrist, Elbow, Long bone or Shoulder CT) CPT Codes: 73200, 73201, 73202 Last Revised Date: May 2020 Guideline Number: NIA_CG_057-1 Implementation Date: January 2021TBD GENERAL INFORMATION: It is an expectation that all patients receive care/services from a licensed clinician. All appropriate supporting documentation, including recent pertinent office visit notes, laboratory data, and results of any special testing must be provided. All prior relevant imaging results, and the reason that alternative imaging (gold standard, protocol, contrast, etc.) cannot be performed must be included in the documentation submitted. INDICATIONS FOR UPPER EXTREMITY CT (HAND, WRIST, ARM, ELBOW, OR SHOULDER) (Plain radiographs must precede CT evaluation): Some indications are for MRI, CT, or MR or CT Arthrogram. More than one should not be approved at the same time. If a CT Arthrogram fits approvable criteria below, approve as CT. Joint specific provocative Orthopedic examination , after x-ray completed and MRI is contraindicated or cannot be done (see Table 1) Note: With a positive orthopedic sign, an initial x-ray is always preferred. However, it is not required to approve advanced imaging. Shoulder (Bencardino, 2013; Jain, 2017; Loh, 2016; Somerville, 2017) o Any positive test listed . Neer’s Sign . Hawkins’s sign . Jobe’s test (empty can) . Drop Arm test * National Imaging Associates, Inc. (NIA) is a subsidiary of Magellan Healthcare, Inc. 1— Upper Extremity CT Copyright © 2019-2020 National Imaging Associates, Inc., All Rights Reserved . Full can test . Hornblower’s sign . Anterior Shoulder Apprehension test (Bankart Lesion) . -
Uploads/NCLEX Test.Pdf
73397_FMxx_FINAL.QXD 4/8/10 2:21 PM Page i NCLEX® High-Risk The Disaster Prevention Manual for Nurses Determined to Pass the RN Licensing Examination Marian C. Condon, DEd, RN, CNE Professor Department of Nursing York College of Pennsylvania York, Pennsylvania Karen S. March, PhD, RN, CCRN, ACNS-BC Professor Department of Nursing York College of Pennsylvania York, Pennsylvania 73397_FMxx_FINAL.QXD 4/8/10 2:21 PM Page ii World Headquarters Jones & Bartlett Learning Jones & Bartlett Learning Canada Jones & Bartlett Learning International 40 Tall Pine Drive 6339 Ormindale Way Barb House, Barb Mews Sudbury, MA 01776 Mississauga, Ontario L5V 1J2 London W6 7PA 978-443-5000 Canada United Kingdom [email protected] www.jblearning.com Jones & Bartlett Learning books and products are available through most bookstores and online booksellers. To contact Jones & Bartlett Learning directly, call 800-832-0034, fax 978-443-8000, or visit our website, www.jblearning.com. Substantial discounts on bulk quantities of Jones & Bartlett Learning publications are available to corpora- tions, professional associations, and other qualified organizations. For details and specific discount informa- tion, contact the special sales department at Jones & Bartlett Learning via the above contact information or send an email to [email protected]. Copyright © 2011 by Jones & Bartlett Learning, LLC All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission from the copyright owner. The authors, editor, and publisher have made every effort to provide accurate information. -

204 Komlofske
9/26/2014 Kari M Komlofske, BSN, FNP-C Orthopedics Objectives t w Describe the knee anatomy w Review the various diagnostic tests specific to help diagnose knee disorders w Discuss the differential diagnosis of knee pain Knee Anatomy t w Three bones articulate t Femur, tibia, patella w Fibula is involved with support w Main Ligaments: t Collateral w (lateral and medial) t Patellar t Cruciate w (anterior and posterior) 1 9/26/2014 Knee Anatomy, Continuedt w Meniscus t Medial and lateral w Muscles t Quads, hamstrings, gastrocnemius w Bursa t Anserine (median), prepatellar, semimembranous (popiteal fossa) Examination of the Knee t w Gait and stance t Is there a Varus Deformity (bow legged), or Valgus Deformity (knocked knees) w Pain/Tenderness t Especially important at the joint line (locate it) t Exacerbation, relief t Medications w Range of motion t Full extension is leg flat 0 degrees t Maximum flexion is 150 degrees to your butt (you need about 120 to get up from a chair comfortably) w Visualization t Swelling, ecchymosis, erythema, deformity Examination Continued t w Other history t Buckling or locking symptoms (hx or PE) t Can’t lay on side with legs together in bed: w Anserine bursitis w Associated with OA and varus deformity t Theater sign (hx) – can’t sit through a movie without your knees aching w Patellofemoral syndrome – “J” sign w One side of quad works harder than other w Extend leg and contract quads w Lateral “J” move = weak vastus medialis 2 9/26/2014 PHYSICAL TESTS t w Ballottement w Posterior Drawer Test w McMurray’s Maneuver w Anterior Drawer/Lachman’s w Varus and Valgus Stress w Apley Grind Ballottement t w Knee Effusion t 1.