Scholarly Work for Practice Doctorate Nurse Anesthesia Programs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Doctor of Philosophy in Pharmacy
collegE OF PHARmacy Doctor of Philosophy in Pharmacy HEALTH PROFESSIONS DIVISION • ENTERINg Class 20142015 NOVA SOUTHEASTERN UNIVERSITY Nova Southeastern University, synonymous with dynamic innovation and intellectual challenge, is the largest independent not-for-profit university in the Southeast, and with an enrollment of nearly 26,000 students, is the ninth largest in the United States. Situated on a beautiful, 314-acre campus in Fort Lauderdale, Florida, the university is experiencing a sustained period of academic growth, fiscal strength, and commitment to the challenges of the 21st century. In this environment of expansion and stability, the university is capitalizing on its strengths in such areas as academic innovation, comprehensive clinical training, and flexible educational delivery systems. Founded in 1964 as Nova University, the institution merged with Southeastern University of the Health Sciences in 1994, creating Nova Southeastern University. To date, the institution has more than 162,000 alumni. Fully accredited by the Commission on Colleges of the Southern Association of Colleges and Schools, the university awards associate’s, bachelor’s, master’s, educational specialist, and doctoral degrees in a wide range of fields including the health professions, law, business, marine sciences, psychology, social sciences, computer and information sciences, and education. The university’s degree programs are administered through 16 academic centers that offer courses at the main campus and at field-based locations throughout Florida; across the nation; and at selected international sites in Europe, mexico, the Pacific Rim, Central and South America, and the Caribbean. With a budget of more than $220 million per year and an upward trend in enrollment, the university will continue to maintain a solid record of academic and fiscal strength and excellence in teaching and community service, while expanding its mission in research and scholarship. -

DEAC Directory of Institutions
Directory of DEAC-Accredited Institutions Offering Partnership Opportunities March 17, 2020 NOTE: Institutions that provide correspondence courses are marked with an asterisk (*). ABRAHAM LINCOLN UNIVERSITY Physiology, Aromatherapy, Botanical Health care, Business Intelligence, www.alu.edu Safety, Complementary Alternative Computer Science Health Care JESSICA PARK, Vice-President and Medicine, Herbal Medicine, Nutrition, Computing, Geospatial Information Dean, School of Law ([email protected]) and Wellness Coaching. Training in Systems, Health care informatics, complementary modalities and Information Systems Management Associate of Science in Business professional continuing education and Nursing; Bachelor of Science Administration, Bachelor of Science in programs in holistic health also Geographic Information Systems; RN Business Administration, Master of available. to Bachelor of Science, Nursing, RN to Business Administration, Diploma in Master of Science, Nursing, and Criminal Justice, Associate of Science AMERICAN NATIONAL UNIVERSITY Doctor of Nursing Practice Executive in Criminal Justice, Bachelor of Science www.an.edu or Education Leadership. in Criminal Justice, Master of Science DAVID YEAMAN, Executive Director of in Criminal Justice, Associate of Arts in Compliance and Accreditation ANAHEIM UNIVERSITY General Studies, Bachelor of Arts in ([email protected]) www.anaheim.edu General Studies, Diploma in Paralegal KATE STRAUSS, VP Admin Studies, Associate of Science in Associate Degrees of Science Degrees ([email protected]) Paralegal -

CALENDAR 2011 Sydney.Edu.Au/Calendar Calendar 2011 Calendar 2011
CALENDAR 2011 sydney.edu.au/calendar Calendar 2011 Calendar 2011 The Arms of the University Sidere mens eadem mutato Though the constellations change, the mind is universal The Arms Numbering of resolutions The following is an extract from the document granting Arms to the Renumbering of resolutions is for convenience only and does not University, dated May 1857: affect the interpretation of the resolutions, unless the context otherwise requires. Argent on a Cross Azure an open book proper, clasps Gold, between four Stars of eight points Or, on a chief Gules a Lion passant guardant Production also Or, together with this motto "Sidere mens eadem mutato" ... to Web and Print Production, Marketing and Communications be borne and used forever hereafter by the said University of Sydney Website: sydney.edu.au/web_print on their Common Seal, Shields, or otherwise according to the Law of Arms. The University of Sydney NSW 2006 Australia The motto, which was devised by FLS Merewether, Second Vice- Phone: +61 2 9351 2222 Provost of the University, conveys the feeling that in this hemisphere Website: sydney.edu.au all feelings and attitudes to scholarship are the same as those of our CRICOS Provider Code: 00026A predecessors in the northern hemisphere. Disclaimer ISSN: 0313-4466 This publication is copyright and remains the property of the University ISBN: 978-1-74210-173-6 of Sydney. This information is valid at the time of publication and the University reserves the right to alter information contained in the Calendar. Calendar 2010 ii Contents -

Doctorate 1 Doctorate
Doctorate 1 Doctorate A doctorate is an academic degree or professional degree that, in most countries, qualifies the holder to teach at the university level in the specific field of his or her degree, or to work in a specific profession. The research doctorate, or the Doctor of Philosophy (Ph.D.) and its equivalent titles, represents the highest academic qualification. While the structure of U.S. doctoral programs is more formal and complex than in some other systems, the research doctorate is not awarded for the preliminary advanced study that leads to doctoral candidacy, but rather for successfully completing and defending the independent research presented in the form of the doctoral dissertation (thesis). Several first-professional degrees use the term “doctor” in their title, such as the Juris Doctor and the US version of the Doctor of Medicine, but these degrees do not universally contain an independent research component or always require a dissertation (thesis) and should not be confused with PhD degrees or other research doctorates.[1] In fact many universities offer Ph.D followed by a professional doctorate degree or joint Ph.D. with the professional degree (most often Ph.D. work comes sequential to the professional degree): eg. Ph.D. in law after J.D. or equivalent [2][3][4][5] in physical therapy after DPT,[6][7] in pharmacy after DPharm.[8][9] Often such professional degrees are refereed as entry level doctorate program [10][11][12] and Ph.D as postprofessional doctorate. In some countries, the highest degree in a given field is called a terminal degree, although this is by no means universal (the term is not in general use in the UK, for example), practice varies from country to country. -

Huntington University of Health Sciences Self-Paced
School of Nutrition and Integrative Health Sciences Self-Paced Programs Catalog of Courses, Academic Programs & Policies 2020-2021 Accredited Distance Learning • Graduate Degree Programs • Undergraduate Degree Programs • Diploma Programs 118 Legacy View Way • Knoxville, TN 37918 Phone: 865-524-8079 • Fax: 865-524-8339 E-mail: [email protected] Toll Free Phone: 800-290-4226 www.huhs.edu Rev. 1/14/2021 A MESSAGE FROM HUHS’ PROVOST Huntington University of Health Sciences was founded in 1985 as the American Academy of Nutrition, to meet the tremendous demand for an accredited independent study program in nutrition. In 2005 we changed our name to Huntington College of Health Sciences (HCHS) and in 2018 to Huntington University of Health Sciences (HUHS) to reflect our expanded academic offerings. Our students come from all over the world and include nutrition counselors, homemakers, health food store professionals, registered dietitians, chiropractors, registered nurses, dentists, physicians, massage therapists, psychologists, nutritional product marketers, military personnel, business executives, pharmacists and others seeking to enrich their knowledge of nutrition. We are proud of our courses as they reflect the tremendous strides that have recently been made in the field of nutrition education. The knowledge you gain from successful completion of your courses will bring you to a new level of health awareness that, if properly applied, should have a profound and lasting effect on your health as well as those you motivate to a healthier lifestyle. We are also proud of the fact that HUHS is the first nutrition institution to attain accreditation by the Distance Education Accrediting Commission. The Distance Education Accrediting Commission is listed by the U.S. -

The University of Notre Dame Australia Research Guide
The University of Notre Dame Austr alia RESEARCH GUIDE “The underlying capacity is a tangible benefi t, the capacity to help people through community engagement. That is vitally important.” — Fleur McIntyre, Associate Professor, School of Health Sciences APPLY DIRECT NOTREDAME.EDU.AU THE OBJECTS OF THE UNIVERSITY OF NOTRE DAME AUSTRALIA ARE: a) the provision of university education within a context of Catholic faith and values; and b) the provision of an excellent standard of – i) teaching, scholarship and research; ii) training for the professions; and iii) pastoral care for its students. WELCOME TO THE UNIVERSITY OF NOTRE DAME AUSTRALIA’S 2019 POSTGRADUATE RESEARCH GUIDE Within these pages, we hope to give you a snapshot of our very special Australian university – a university which extends from the west coast in the beautiful and historic city of Fremantle, to the north-west town of Broome, and across the continent to our Campus located in the heart of the city of Sydney. Notre Dame is unique for a number of reasons: › As Australia’s fi rst Catholic university, Notre Dame follows the traditions and practices of Catholic higher education which, for centuries in many countries around the world, has offered leadership in university education. › We are committed to a personalised university education, a specifi c focus on pastoral care and support for all our students. › Higher degrees by research are offered at each of our nine academic Schools. Through our three research Institutes, you have the opportunity to work with leading academics on projects and programs that deliver value to people and communities across the country. -
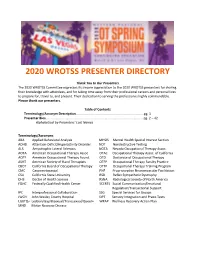
2020 Wrotss Presenter Directory
2020 WROTSS PRESENTER DIRECTORY Thank You to Our Presenters The 2020 WROTSS Committee expresses its sincere appreciation to the 2020 WROTSS presenters for sharing their knowledge with attendees, and for taking time away from their professional careers and personal lives to prepare for, travel to, and present. Their dedication to serving the profession is highly commendable. Please thank our presenters. Table of Contents Terminology/Acronym Description...........................................................................pg. 1 Presenter Bios........................................................................................................... pg. 2 – 42 Alphabetical by Presenters’ Last Names Terminology/Acronyms ABA Applied Behavioral Analysis MHSIS Mental Health Special Interest Section ADHD Attention-Deficit/Hyperactivity Disorder NDT Nondestructive Testing ALS Amyotrophic Lateral Sclerosis NOTA Nevada Occupational Therapy Assoc. AOTA American Occupational Therapy Assoc. OTAC Occupational Therapy Assoc. of California AOTF American Occupational Therapy Found. OTD Doctorate of Occupational Therapy ASHT American Society of Hand Therapists OTFP Occupational Therapy Faculty Practice CBOT California Board of Occupational Therapy OTTP Occupational Therapy Training Program CMC Carpometacarpal PNF Proprioceptive Neuromuscular Facilitation CSU California State University RSD Reflex Sympathetic Dystrophy DHS Doctor of Health Science RSNA Radiological Society of North America FQHC Federally Qualified Health Center SCERTS Social Communication/Emotional -
Doctor of Philosophy (Ph.D.) in Health Science Brochure | College Of
NSU’s Dr. Pallavi Patel College of Health Care Sciences DOCTOR OF PHILOSOPHY (PH.D.) IN HEALTH SCIENCE Online Program Health Professions Division | Students Entering 2020 Now Accepting Applications nova.edu NSU helps students become leaders in the health science field. THE NSU EDGE • low student-to-faculty ratio • advanced patient simulation technology • extensive resources • clinical experience • opportunities to aid urban and rural underserved populations • interprofessional service-learning • faculty and staff members who care about your success • commitment to developing students of academic and clinical distinction • track record for nurturing patient-focused leaders TABLE OF CONTENTS Message from the Dean ���������������������������������������������������� 2 Program Overview �������������������������������������������������������������� 5 Fast Facts ������������������������������������������������������������������������������ 5 Computer Skills and Requirements �������������������������������� 6 Transfer Credits �������������������������������������������������������������������� 7 Course of Study . 8 Admissions Requirements �����������������������������������������������10 Application Procedures . .12 Requirements for Graduation ��������������������������������������������15 Tuition, Fees, and Financial Aid . .15 Message from the HPD Chancellor ���������������������������������16 Health Professions Division Fast Facts �������������������������17 NSU’s HPD Degree Programs ����������������������������������������20 NSU Recognitions -

Nsubachelor of Health Science
Bachelor of NSU Health Science Nova Southeastern University Health Professions Division Entering Class 2016 Online Program NSU MISSION STATEMENT The mission of Nova Southeastern University, a private, not-for-profit institution, is to offer a diverse array of innovative academic programs that complement on-campus educational opportunities and resources with accessible, distance-learning programs to foster academic excellence, intellectual inquiry, leadership, research, and commitment to community through engagement of students and faculty members in a dynamic, lifelong learning environment. NOVA SOUTHEASTERN UNIVERSITY— growth, fiscal strength, and commitment to the synonymous with dynamic innovation and challenges of the 21st century. intellectual challenge—is the second largest, In this environment of expansion and stability, the private, nonprofit university in the Southeast and university is capitalizing on its strengths in such areas 1 of only 37 universities (out of more than 4,000) as academic innovation, comprehensive clinical that have earned designations for both High training, and flexible educational delivery systems. Research Activity and Community Engagement from the Carnegie Foundation for the Advancement Founded in 1964 as Nova University, the institution of Teaching. Situated on a beautiful, 314-acre merged with Southeastern University of the Health campus in Fort Lauderdale, Florida, the university Sciences in 1994, creating Nova Southeastern is experiencing a sustained period of academic University. To date, the institution has more than NSU MAIN CAMPUS 166,000 alumni and current enrollment of more than main campus and at field-based locations throughout 24,000 students. Fully accredited by the Commission Florida; across the nation; and at selected international on Colleges of the Southern Association of Colleges sites in Europe, Mexico, the Pacific Rim, Central and and Schools, the university awards associate’s, South America, and the Caribbean. -

College of Health Care Sciences Audiology Nova Southeastern University
Nova Southeastern University NSUWorks Health Professions Divisions Course Catalogs NSU Course Catalogs and Course Descriptions 2019 College of Health Care Sciences Audiology Nova Southeastern University Follow this and additional works at: https://nsuworks.nova.edu/hpd_coursecatalogs Part of the Medicine and Health Sciences Commons NSUWorks Citation Nova Southeastern University, "College of Health Care Sciences Audiology" (2019). Health Professions Divisions Course Catalogs. 384. https://nsuworks.nova.edu/hpd_coursecatalogs/384 This Program Overview is brought to you for free and open access by the NSU Course Catalogs and Course Descriptions at NSUWorks. It has been accepted for inclusion in Health Professions Divisions Course Catalogs by an authorized administrator of NSUWorks. For more information, please contact [email protected]. Dr. Pallavi Patel College of Health Care Sciences NOVA SOUTHEASTERN UNIVERSITY HEALTH PROFESSIONS DIVISION Audiology ENTERING CLASS 2019 NOVA SOUTHEASTERN UNIVERSITY—synonymous with dynamic innovation and intellectual challenge—is the second largest, private, nonprofit university in the Southeast and 1 out of only 361 colleges and universities nationally selected for the Carnegie Foundation’s Community Engagement Classification. Situated on a beautiful, 314-acre campus in Fort Lauderdale, Florida, the university is experiencing a sustained period of academic growth, fiscal strength, and commitment to the challenges of the 21st century. In this environment of expansion and stability, the university is capitalizing on its strengths in such areas as academic innovation, comprehensive clinical training, and flexible educational delivery systems. Founded in 1964 as Nova University, the institution merged with Southeastern University of the Health Sciences in 1994, creating Nova Southeastern University. To date, the institution has more than 183,000 alumni and current enrollment of nearly 21,000 students. -
B.S. in Nursing Brochure Nova Southeastern University
Nova Southeastern University NSUWorks Health Professions Divisions Course Catalogs NSU Course Catalogs and Course Descriptions 2016 B.S. in Nursing Brochure Nova Southeastern University Follow this and additional works at: http://nsuworks.nova.edu/hpd_coursecatalogs Part of the Nursing Commons NSUWorks Citation Nova Southeastern University, "B.S. in Nursing Brochure" (2016). Health Professions Divisions Course Catalogs. Paper 69. http://nsuworks.nova.edu/hpd_coursecatalogs/69 This Program Overview is brought to you for free and open access by the NSU Course Catalogs and Course Descriptions at NSUWorks. It has been accepted for inclusion in Health Professions Divisions Course Catalogs by an authorized administrator of NSUWorks. For more information, please contact [email protected]. CollegeCollege of of NursingHealth Care Sciences Undergraduate NursingPhysician Assistant • FortEntry BachelorLauderdale of Science in Nursing Program • R.N. to B.S.N. Nova Southeastern University | Health Professions Division | Entering Class 2016 NSU MISSION STATEMENT The mission of Nova Southeastern University, a private, not-for-profit institution, is to offer a diverse array of innovative academic programs that complement on-campus educational opportunities and resources with accessible, distance-learning programs to foster academic excellence, intellectual inquiry, leadership, research, and commitment to community through engagement of students and faculty members in a dynamic, lifelong learning environment. NOVA SOUTHEASTERN UNIVERSITY— growth, fiscal strength, and commitment to the synonymous with dynamic innovation and challenges of the 21st century. intellectual challenge—is the second largest, In this environment of expansion and stability, the private, nonprofit university in the Southeast and university is capitalizing on its strengths in such areas 1 of only 37 universities (out of more than 4,000) as academic innovation, comprehensive clinical that have earned designations for both High training, and flexible educational delivery systems. -

Public Health Education in Montenegro
WP1. ANALYSIS AND ROADMAPING: PUBLIC HEALTH EDUCATION IN MONTENEGRO DELIVERABLE 1.2‘Analysis of EU practice for public healtheducation’ Published on:11/07/2017 Authors: Prof. Dr. John Mantas, Health Info Lab, Dept. Of Public Health, University of Athens, Greece Katia Kolokathi, Health Info Lab,Dept. Of Public Health, University of Athens, Greece Prof. Dr Ramo Sendelj, University of Donja Gorica, Montenegro Prof. Dr Milica Vukotic, University of Donja Gorica,Montenegro Prof. Dr Maja Drakic Grgur, University of Donja Gorica, Montenegro Assist.Prof.Dr Ivana Ognjanovic, University of Donja Gorica, Montenegro Boris Bastijancic,University of Donja Gorica, Montenegro Prof. Dr. Elske Ammenwerth, UMIT, Austria Prof. Dr Róza Ádany, DSc, Faculty of Public Health, University of Debrecen, Hungary Prof. Dr. Orsolya Varga, Faculty of Public Health, University of Debrecen, Hungary Doc. dr Anđela Jakšić Stojanović, Mediterranean University, Montenegro Doc. dr. Danilo Ćupić, Mediterranean University,Montenegro Prof. dr Jelena Žugić,Mediterranean University,Montenegro Doc. dr Dragica Žugić, Mediterranean University, Montenegro Prof. Dr. Petra Knaup, Inst. of Med Biometry and Informatics, University of Heidelberg Max Seitz,Inst. of Med Biometry and Informatics, University of Heidelberg, Germany Prof. dr Goran Nikolic, Faculty of Medicine, University of Montenegro Prof.dr Dragan Đurić, Institute of Modern Technology Montenegro Bojana Tošić, Institute of Modern Technology Montenegro European Commission Erasmus+ Project: | PROJECT COORDINATOR: University of Donja Gorica 573997-EPP-1-2016-1-ME-EPPKA2-CBHE-JP | Donja Gorica, 81 000 Podgorica, Montenegro This project has been funded with support from the European | http://www.udg.edu.me Commission. | [email protected] This publication [communication] reflects the views only of the | Tel:+382(0)20 410 777 author, and the Commission cannot be held responsible for any use | Fax:+382(0)20 410 766 which may be made of the information contained therein.