DHSC Integrated Care Vision
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Gd 2020/0058
GD 2020/0058 2020/21 1 Programme for Government October 2020 – July 2021 Introduction The Council of Ministers is pleased to bring its revised Programme for Government to Tynwald. The Programme for Government was agreed in Tynwald in January 2017, stating our strategic objectives for the term of our administration and the outcomes we hoped to achieve through it. As we enter the final year of this parliament, the world finds itself in the grip of the COVID-19 pandemic. This and other external factors, such as the prospect of a trade agreement between the UK and the EU, will undoubtedly continue to influence the work of Government in the coming months and years. What the Isle of Man has achieved over the past six months, in the face of COVID-19, has been truly remarkable, especially when compared to our nearest neighbours. The collective response of the people of our Island speaks volumes of the strength of our community and has served to remind us of the qualities that make our Island so special. At the beginning of the pandemic the Council of Ministers suspended the Programme for Government, and any work within it, to bring to bear the complete resources of the public service in the fight against coronavirus as we worked to keep our island and its people safe. Through the pandemic we have seen behaviour changes in society and in Government, and unprecedented times seem to have brought unprecedented ways of working. It is important for the future that we learn from the experiences of COVID and carry forward the positive elements of both what was achieved, and how Government worked together to achieve it. -

Landlord and Tenant (Private Housing) Bill Committee
H O U S E O F K E Y S O F F I C I A L R E P O R T R E C O R T Y S O I K O I L Y C H I A R E A S F E E D P R O C E E D I N G S D A A L T Y N LANDLORD AND TENANT (PRIVATE HOUSING) BILL COMMITTEE HANSARD Douglas, Monday, 8th September 2014 PP2014/0116 LTPHB, No. 3 All published Official Reports can be found on the Tynwald website www.tynwald.org.im/Official Papers/Hansards/Please select a year: Published by the Office of the Clerk of Tynwald, Legislative Buildings, Finch Road, Douglas, Isle of Man, IM1 3PW. © High Court of Tynwald, 2014 BILL COMMITTEE, MONDAY, 8th SEPTEMBER 2014 Members Present: Chairman: Mr C C Thomas MHK Mr D C Cretney MHK Mr L I Singer MHK Clerk: Mr R I S Phillips Contents Procedural ...................................................................................................................................... 55 EVIDENCE OF Mr D Ashford, Chairman of the Housing and Property Advisory Committee, Ms K Rice, Chief Executive, and Mr I Clague, Borough Engineer and Surveyor, Douglas Borough Council ............................................................................................................... 55 The Court adjourned at 3.15 p.m. and resumed its sitting at 3.26 p.m. when Mr Harmer and Mr Whiteway were called .......................................................................... 68 Procedural ...................................................................................................................................... 68 EVIDENCE OF Mr T Harmer, Commissioner and Mr P Whiteway, Clerk, Ramsey Town Commissioners ....................................................................................................... 69 The Committee adjourned at 4.06 p.m. and resumed its sitting at 4.14 p.m. ............................... 79 Procedural ...................................................................................................................................... 80 The Committee adjourned at 4.15 p.m. -
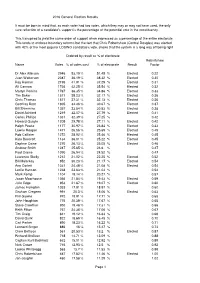
2016 General Election Statistics Summary
2016 General Election Results It must be born in mind that, as each voter had two votes, which they may or may not have used, the only sure reflection of a candidate's support is the percentage of the potential vote in the constituency. This transpired to yield the same order of support when expressed as a percentage of the entire electorate This tends to endorse boundary reforms but the fact that Chris Robertshaw (Central Douglas) was elected with 42% of the most popular LOSING candidate's vote, shows that the system is a long way off being right Ordered by result as % of electorate Robertshaw Name Votes % of votes cast % of electorate Result Factor Dr Alex Allinson 2946 53.19 % 51.45 % Elected 0.22 Juan Watterson 2087 36.19 % 38.32 % Elected 0.30 Ray Harmer 2195 41.91 % 37.29 % Elected 0.31 Alf Cannan 1736 42.25 % 35.54 % Elected 0.32 Martyn Perkins 1767 36.35 % 34.86 % Elected 0.33 Tim Baker 1571 38.23 % 32.17 % Elected 0.36 Chris Thomas 1571 37.31 % 32.13 % Elected 0.36 Geoffrey Boot 1805 34.46 % 30.67 % Elected 0.37 Bill Shimmins 1357 33.54 % 30.53 % Elected 0.38 David Ashford 1219 32.07 % 27.79 % Elected 0.41 Carlos Phillips 1331 32.39 % 27.25 % 0.42 Howard Quayle 1205 29.78 % 27.11 % Elected 0.42 Ralph Peake 1177 30.97 % 26.84 % Elected 0.43 Lawrie Hooper 1471 26.56 % 25.69 % Elected 0.45 Rob Callister 1272 28.92 % 25.46 % Elected 0.45 Kate Beecroft 1134 36.01 % 25.22 % Elected 0.45 Daphne Caine 1270 26.13 % 25.05 % Elected 0.46 Andrew Smith 1247 25.65 % 24.6 % 0.47 Paul Craine 1090 26.94 % 24.52 % 0.47 Laurence Skelly 1212 21.02 -

Invest with Your Head and Your Heart
www.business365iom.co.uk | JULY 2020 ISSUE INVEST WITH YOUR HEAD AND YOUR HEART How RL360 is championing responsible investing For life’s financial journey www.rl360.com RL360 is part of COVID19 CASTLE MONA B365 FEATURE: HOUSEHOLD RESTORATION WELLNESS AT WORK INCOME SURVEY PLANS It’s a topic that many companies have started taking seriously. The reasons aren’t entirely A survey has been launched by Isle of Man Tevir Group has submitted plans for the first altruistic though, because – in purely financial Government Economic Affairs Division, phase of the restoration of the Castle Mona terms – looking after the health and wellbeing to help further understand the impacts of Hotel. The proposed works are detailed within of staff increases efficiency and improves staff the coronavirus (COVID-19) pandemic on three planning applications and three registered retention. people in the Isle of Man. building applications. THE ISLE OF MAN’S ONLY DEDICATED BUSINESS MAGAZINE NEWS | COMMENT | INSIGHT | PEOPLE | MOVEMENTS | FEATURES | TECHNOLOGY | HEALTH ProtectProtect youryour businessbusiness Secure offshore email, archiving & security awareness training services Inside your organisation Educate employees to recognise threats and use best practice security policies with effective online security training programs. At your perimeter Protection from inbound phishing, malware and spam attacks whether in the office, at home or mobile. Contact Us business.sure.com July CORONAVIRUS HOUSEHOLD IMPACT 5 SURVEY LAUNCHED A comprehensive round-up of the latest business news ProtectProtect youryour covering all sectors within the Isle of Man’s diverse and FIRST LOOK AT CASTLE MONA dynamic business environment. 6 RESTORATION PLANS PDMS ENHANCES MARITIME Expert comment from leading figures within the 10 EXPERIENCE businessbusiness business community, on a variety of topical issues across a range of sectors. -

Actions Reporting
PROGRAMME FOR GOVERNMENT Q1 REPORTING 2019/20 DEPARTMENT ACTIONS 1 DEPARTMENT ACTIONS The Programme for Government ‘Our Island - a special place to live and work’ was approved by Tynwald in January 2017 and in April 2017 a performance framework, ‘Delivering a Programme for Government’, was also approved. The ‘Programme for Government 2016-21’ is a strategic plan that outlines measurable goals for Government. The Council of Ministers have committed to providing a public update against the performance framework on a quarterly basis. This report provides an update on performance through monitoring delivery of the actions committed to. The first quarter for 2019/20 ran April, May and June 2019. Information has been provided from across Government Departments, Boards and Offices, and the Cabinet Office have collated these to provide this report. The Programme for Government outlines a number of initial actions that were agreed by the Council of Ministers which will help take Government closer to achieving its overall objectives and outcomes. Departments Boards and Offices have developed action plans to deliver these actions and this report provides an update status report on delivery against these action plans. 2 Q2 Q3 Q4 Q1 Lead Lead Sub Ref Action Comment Political Sponsor End Date 2018/19 2018/19 2018/19 2019/20 Department Committee We have an economy where local entrepreneurship is supported and thriving and more new businesses are choosing to call the Isle of Man home 1.1.01 Promote and drive the Enterprise This action was Department -

Year 4 Amendments
PROGRAMME FOR GOVERNMENT – YEAR 4 Updated 23/09/20 Programme for Government – Year 4 (October 2020 – July 2021) Actions to be removed We have an economy where local entrepreneurship is supported and thriving and more new businesses are choosing to call the Isle of Man home REF ACTION STATUS LEAD DEPARTMENT POLITICAL SPONSOR END DATE Form local development partnerships and produce local Replaced with 1.11 CABO Ray Harmer* Dec 2019 development plans 1.13 Secure a viable proposal for the redevelopment of the Replaced with 1.12 DOI Marlene Maska* April 2021 Summerland Site 1.13 We have a diverse economy where people choose to work and invest We have Island transport that meets our social and economic needs REF ACTION STATUS LEAD DEPARTMENT POLITICAL SPONSOR END DATE We have Island transport that meets our social and economic needs REF ACTION STATUS LEAD DEPARTMENT POLITICAL SPONSOR END DATE *Political Sponsor at the time the action was in progress 2 PROGRAMME FOR GOVERNMENT – YEAR 4 Updated 23/09/20 We have an education system which matches our skills requirements now and in the future REF ACTION STATUS LEAD DEPARTMENT POLITICAL SPONSOR END DATE 4.01 Introduce a regulatory framework for pre-school services Completed DESC Alex Allinson Dec 2021 4.02 Harmonise our further and higher education to ensure we Completed DESC Alex Allinson June 2018 achieve a more effective and value for money service We have an infrastructure which supports social and economic wellbeing REF ACTION STATUS LEAD DEPARTMENT POLITICAL SPONSOR END DATE Develop brownfield -
Legislative Council Elections Bill Was One of Only Two Items to Pass Through Both Branches and Be Promulgated on Tynwald Hill Within the Same Year
Tynwald Annual Report Parliamentary year 2016/2017 We hope you will find this report useful. If you would like to comment on any aspect of it, please contact: The Clerk of Tynwald Office of the Clerk of Tynwald Legislative Buildings Finch Road Douglas Isle of Man IM1 3PW Get in touch Twitter : @tynwaldinfo Telephone: +44 (0)1624 685500 Email: [email protected] An electronic copy of this report can be found at: www.tynwald.org.im © Office of the Clerk of Tynwald Copyright 2017 The text of this document may be reproduced free of charge in any format or medium providing that it is reproduced accurately and not used in a misleading or derogatory context. The material must be acknowledged as copyright of the Office of the Clerk of Tynwald and the title of the document specified. PP 2017/0145 2 Tynwald Annual Report 2016/2017 Contents Foreword by the Presiding Officers 4 1867 Celebrations 6 Changes in Political Membership 8 The Work of the Legislature 10 Tynwald Day 18 Interparliamentary Engagement 26 Education and Outreach 34 The Clerk of Tynwald’s Office 42 Appendix 48 3 PRESIDENT OF TYNWALD The Hon Stephen Charles Rodan BSc (Hons) MRPharmS MLC SPEAKER OF THE HOUSE OF KEYS The Hon Juan Paul Watterson BA FCA CMgr FCMI SHK foreword 4 Tynwald Annual Report 2016/2017 Welcome to the Tynwald Annual Report 2016/7 2016 saw the 150th anniversary of the House of Keys Elections Act 1866. In 2017 we celebrated the 150th anniversary of the first elections which took place under that Act, with polling taking place in the first week of April 1867. -

PROGRAMME for GOVERNMENT Q4 REPORTING Jan - Mar 2019/20 DEPARTMENT ACTIONS
PROGRAMME FOR GOVERNMENT Q4 REPORTING Jan - Mar 2019/20 DEPARTMENT ACTIONS Page 1 of 28 DEPARTMENT ACTIONS The Programme for Government ‘Our Island - a special place to live and work’ was approved by Tynwald in January 2017 and in April 2017 a performance framework, ‘Delivering a Programme for Government’, was also approved. The ‘Programme for Government 2016-21’ is a strategic plan that outlines measurable goals for Government. The Council of Ministers have committed to providing a public update against the performance framework on a quarterly basis. This report provides an update on performance through monitoring delivery of the actions committed to. The fourth and final quarter for 2019/20 ran January, February and March. Information has been provided from across Government Departments, Boards and Offices, and the Cabinet Office have collated these to provide this report on Key Performance Indicators. The Programme for Government outlines a number of initial actions that were agreed by the Council of Ministers which will help take Government closer to achieving its overall objectives and outcomes. Departments Boards and Offices have developed action plans to deliver these actions and this report provides an update status report on delivery against these action plans. Page 2 of 28 Q1 Q2 Q3 Q4 Lead Ref Action Comment Political Sponsor End Date 2019/20 2019/20 2019/20 2019/20 Department We have an economy where local entrepreneurship is supported and thriving and more new businesses are choosing to call the Isle of Man 1.1.02 Partner -
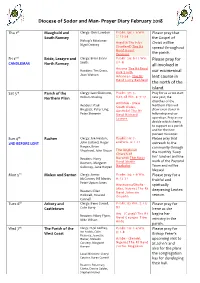
Diocese of Sodor and Man- Prayer Diary February 2018
Diocese of Sodor and Man- Prayer Diary February 2018 Thu 1st Maughold and Clergy: Chris Lowdon Psalm: 50: 1-6 Wis. Please pray that South Ramsey 2: 12-24 the Gospel of Bishop’s Missioner: Argyll & The Isles - Nigel Cretney Christ will be (Scotland) The Rt spread throughout Revd Kevin Pearson the parish. Fri 2nd Bride, Lezayre and Clergy: Brian Evans- Psalm: 29: 8-11 Wis. Please pray for CANDLEMAS North Ramsey Smith 3:1-9 all involved in Arizona The Rt Revd Readers: Tim Grass, Kirk Smith our ecumenical Joan Watson Arkansas- The Rt lent course in Revd Larry Benfield the north of the island. Sat 3rd Parish of the Clergy: Iaen Skidmore, Psalm: 37: 3- Pray for us as we start Northern Plain William Mackay 6,27,28 Wis. 4: 7-17 new year; the churches of the Armidale - (New Readers: Paul South Wales, Northern Plain will Bregazzi, Peter Ling, Australia) The Rt draw even closer in Peter Shimmin Revd Richard fellowship and co- Lewers operation. Pray as we decide which charity to support as a parish and for the new pioneer missioner. Sun 4th Rushen Clergy: Joe Heaton, Psalm: 19: 7- Please pray that 2ND BEFORE LENT John Gulland, Roger end Wis. 6: 1-11 outreach to the Harper, Brian community through Shephard, John Sheen The Anglican Church of the monthly ‘Soup Inn’ lunches and the Readers: Harry Burundi The Most work of the Pastoral Dawson, Margaret Revd Martin Nyaboho Galloway, June Harper Team and will be blessed. Mon 5th Malew and Santon Clergy: James Psalm: 34: 1-6 Wis. -
Annual Report 2015-16 0
Tynwald Annual Report 2015/2016 Get in touch Engage with Tynwald on Twitter @tynwaldinfo Get live updates during Tynwald sittings from @tynwaldlive We hope you will find this report useful. If you would like to comment on any aspect of it, please contact: The Clerk of Tynwald Office of the Clerk of Tynwald Legislative Buildings Finch Road Douglas Isle of Man IM1 3PW Telephone: +44 (0)1624 685500 Email: [email protected] An electronic copy of this report can be found at: www.tynwald.org.im © Office of the Clerk of Tynwald Copyright 2016 The text of this document may be reproduced free of charge in any format or medium providing that it is reproduced accurately and not used in a misleading or derogatory context. The material must be acknowledged as copyright of the Office of the Clerk of Tynwald and the title of the document specified. PP2016/0151 Tynwald Annual Report 2015-2016 CONTENTS FOREWORD BY THE PRESIDING OFFICERS 5 A YEAR OF COMINGS AND GOINGS 13 THE WORK OF THE LEGISLATURE 25 TYNWALD DAY 29 INTERPARLIAMENTARY ENGAGEMENT 37 EDUCATION AND OUTREACH 46 THE CLERK OF TYNWALD’S OFFICE 51 APPENDIX 55 Foreword by the Presiding Officers The Hon Stephen Charles Rodan The Hon Juan Paul Watterson Bsc (Hons) MRPharmS MLC BA FCA CMgr FCMI SHK President of Tynwald Speaker of the House of Keys WELCOME TO THE TYNWALD ANNUAL REPORT FOR 2015/2016 This report covers the last year of the House of Keys which was elected in September 2011 and dissolved in August 2016. In it we pay tribute to former Governor Mr Adam Wood, to the outgoing President, the Hon Clare Christian OBE, and to the 12 MHKs who left the House this year. -

21St February 2020 Mr. Roger Phillips Secretary to the House of Keys The
House of Keys Y Chiare as Feed Legislative Buildings Oikyn Slattyssagh Douglas Doolish Isle of Man Ellan Vannin IM1 3PW IM1 3PW British Isles Ny Ellanyn Goaldagh Tel: 01624651517 Email: [email protected] 21st February 2020 Mr. Roger Phillips Secretary to the House of Keys The Clerk of Tynwald’s Office Legislative Buildings Finch Road Douglas IM1 3PW Dear Mr Phillips, Re: Nomination for the election to Legislative Council to be held on the 12th March 2020. I am writing to propose Mrs Danielle Bell of [Address redacted] for candidature at the forthcoming election to fill four vacant seats of the Legislative Council. Mrs Bell’s nominations will be seconded by Mr David Ashford MHK, with Mr Lawrie Hooper MHK and The Honourable Howard Quayle MHK acting as assenters to the nomination. Mrs Bell’s contact details are as follows: [Contact details redacted] I believe that her background in research and analysis give her the necessary skills to apply critical appraisal and scrutiny key for a potential member of the Legislative Council. She has qualifications in Sport Science and Coaching as well as further training regarding valuing people and diversity, research methods and a wide experience of island life. I believe Mrs Bell would be an asset to the Legislative Council, and to the wider Tynwald Court, and request that she be considered for a vacancy. House of Keys – the elected Branch of Tynwald – the Isle of Man Parliament THE OLDEST CONTINUOUS PARLIAMENT IN THE WORLD Yours sincerely Dr Alex Allinson MHK Member of the House of Keys for Ramsey cc. -

Western News from Your MHKS 2018
Geoffrey Ray Harmer Boot MHK for MHK for Glenfaba & Peel Glenfaba & Peel Minister of Spring/summer 2018 Minister of Environment Food Glenfaba & Peel Infrastructure & Agriculture Welcome to the second of our joint newsletters from the West of (DOI) (DEFA) the Island. We had hoped to produce one every six months but with so much interaction now taking place through social media Tynwald: 01624 685485 Tynwald: 01624 685596 Mobile: 07624 381497 Facebook, Twitter etc. we have decided that an annual overview Mobile: 07624 215577 www.geoffreyboot.org for those of you that don’t have access to social media will www.rayharmer.im [email protected] [email protected] hopefully give you a broad-brush of what’s happened during the year. Programme for Government —one year on Having a Programme for Government has been a great help both for us in Government as well as for Parliament as a whole, providing a road map for the five years of this administraon. We are now some 18 months in and have ust gone through a fairly comprehensive review of where we are in terms of delivery. The programme itself is available on www.gov.im/ media/1354707/programme-for-government-2016-2021.pdf ,ollowing consultaon with all members some amendments are being made for the coming year. This is a-er all a living document. .n terms of what/s being delivered, our individual items will detail what we have done as 0inisters in 12,A and 1O., and it/s fair to say in general terms we are delivering on the commitments our respecve 1epartments have made.