A Case of Drug-Induced Proximal Tubular Dysfunction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review of Succimer for Treatment of Lead Poisoning
Review of Succimer for treatment of lead poisoning Glyn N Volans MD, BSc, FRCP. Department of Clinical Pharmacology, School of Medicine at Guy's, King's College & St Thomas' Hospitals, St Thomas' Hospital, London, UK Lakshman Karalliedde MB BS, DA, FRCA Consultant Medical Toxicologist, CHaPD (London), Health Protection Agency UK, Visiting Senior Lecturer, Division of Public Health Sciences, King's College Medical School, King's College , London Senior Research Collaborator, South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, Peradeniya, Sri Lanka. Heather M Wiseman BSc MSc Medical Toxicology Information Services, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 9RT, UK. Contact details: Heather Wiseman Medical Toxicology Information Services Guy’s & St Thomas’ NHS Foundation Trust Mary Sheridan House Guy’s Hospital Great Maze Pond London SE1 9RT Tel 020 7188 7188 extn 51699 or 020 7188 0600 (admin office) Date 10th March 2010 succimer V 29 Nov 10.doc last saved: 29-Nov-10 11:30 Page 1 of 50 CONTENTS 1 Summary 2. Name of the focal point in WHO submitting or supporting the application 3. Name of the organization(s) consulted and/or supporting the application 4. International Nonproprietary Name (INN, generic name) of the medicine 5. Formulation proposed for inclusion 6. International availability 7. Whether listing is requested as an individual medicine or as an example of a therapeutic group 8. Public health relevance 8.1 Epidemiological information on burden of disease due to lead poisoning 8.2 Assessment of current use 8.2.1 Treatment of children with lead poisoning 8.2.2 Other indications 9. -

WO 2014/195872 Al 11 December 2014 (11.12.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/195872 Al 11 December 2014 (11.12.2014) P O P C T (51) International Patent Classification: (74) Agents: CHOTIA, Meenakshi et al; K&S Partners | Intel A 25/12 (2006.01) A61K 8/11 (2006.01) lectual Property Attorneys, 4121/B, 6th Cross, 19A Main, A 25/34 (2006.01) A61K 8/49 (2006.01) HAL II Stage (Extension), Bangalore 560038 (IN). A01N 37/06 (2006.01) A61Q 5/00 (2006.01) (81) Designated States (unless otherwise indicated, for every A O 43/12 (2006.01) A61K 31/44 (2006.01) kind of national protection available): AE, AG, AL, AM, AO 43/40 (2006.01) A61Q 19/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A01N 57/12 (2006.01) A61K 9/00 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, AOm 59/16 (2006.01) A61K 31/496 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, PCT/IB20 14/06 1925 KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (22) International Filing Date: OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, 3 June 2014 (03.06.2014) SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, (25) Filing Language: English TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

Chelating Drug Therapy: an Update
Open Access Austin Journal of Genetics and Genomic Research Review Article Chelating Drug Therapy: An Update Vijay Kumar1, Ashok Kumar2*, Sandeep Kumar Singh1, Manoj Kumar3, Surendra Kumar2, Dinesh Abstract 4 5 Kumar and Ragni Singh Purpose: To study the clinical effects of metal toxicity and current 1Department of Neurology, SGPGIMS, India recommendations for management, including chelation therapy, are reviewed. 2Department of Medical Genetics, SGPGIMS, India 3Department of Microbiology, SGPGIMS, India Summary: Metals are essential to many biological processes, but excess 4Department of Chemistry, Dr. R.M.L. Avadh University, of it becomes hazardous to life. These are necessary for cell growth, electron India transport chain, several enzymatic activities and response of immune systems. 5Bheem Rao Ambedkar Bihar University, India They also serve as a cofactor for several enzymes. Chelation therapy is used for clinical management of the excess of metal. However, each metal requires *Corresponding author: Ashok Kumar, Department a specific chelation agent. A chelate is a compound form between metal and a of Medical Genetics, Sanjay Gandhi Post Graduate compound that contains two or more potential ligands. A promising Fe chelator Institute of Medical Sciences, Lucknow, India is Desferrioxamine (Desferal). Penicillamine and Trientine are uses for copper Received: March 12, 2015; Accepted: April 24, 2015; chelation. Meso-2,3-Dimercaptosuccinic Acid (DMSA) and 2,3-Dimercapto- Published: April 27, 2015 Propanesulphonate (DMPS) can be used as effective chelator of mercury. Dimercaprol, edetate calcium disodium, and succimer are the three agents primarily used for chelation of lead. Conclusion: Metal toxicity remains a significant public health concern. Elimination of elevated metal ions can be achieved by proper chelation agents. -

Changes in Tissue Gadolinium Biodistribution Measured in an Animal Model Exposed to Four Chelating Agents
Japanese Journal of Radiology (2019) 37:458–465 https://doi.org/10.1007/s11604-019-00835-1 ORIGINAL ARTICLE Changes in tissue gadolinium biodistribution measured in an animal model exposed to four chelating agents Türker Acar1,6 · Egemen Kaya2 · Mustafa Deniz Yoruk3 · Neslihan Duzenli4 · Recep Selim Senturk4 · Cenk Can4 · Lokman Ozturk3 · Canberk Tomruk5 · Yigit Uyanikgil5 · Frank J. Rybicki6 Received: 17 December 2018 / Accepted: 22 March 2019 / Published online: 30 March 2019 © Japan Radiological Society 2019 Abstract Purpose This study investigated the potential to reduce gadolinium levels in rodents after repetitive IV Gadodiamide admin- istration using several chelating agents. Materials and methods The following six groups of rats were studied. Group 1: Control; Group 2: Gadodiamide only; Group 3: Meso-2,3-Dimercaptosuccinic acid (DMSA) + Gadodiamide; Group 4: N-Acetyl-L-cysteine (NAC) + Gadodiamide; Group 5: Coriandrum sativum extract + Gadodiamide; and Group 6: Deferoxamine + Gadodiamide. Brain, kidney, and blood samples were evaluated via inductively coupled plasma mass spectrometry. The brain was also evaluated histologically. Results Kidney gadolinium levels in Groups 4 and 5 were approximately double that of Group 2 (p = 0.033 for each). There was almost no calcifcation in rat hippocampus for Group 4 rodents when compared with Groups 2, 3, 5 and 6. Conclusion Our preliminary study shows that excretion to the kidney has a higher propensity in NAC and Coriandrum sati- vum groups. It may be possible to change the distribution of gadolinium by administrating several agents. NAC may lower Gadodiamide-induced mineralization in rat hippocampus. Keywords Gadolinium deposition · Dimercaptosuccinic acid · N-Acetyl-L-cysteine · Coriandrum sativum · Deferoxamine Introduction However, the safety profle of gadolinium-based agents [1] was questioned after the discovery of nephrogenic sys- Gadolinium-based contrast agents (GBCA) have been safely temic fbrosis [2], a scleroderma-like disease characterized used in diagnostic radiology since the 1980s. -

Recommended Chelation Protocol for Children with Blls ≥45 Μg/Dl
The New York City Department of Health and Mental Hygiene Guidelines for Health Care Providers Recommended Chelation Protocol for Children With BLLs ≥45 μg/dL Before Providing Chelation Therapy: • Confirm the blood lead level (BLL) ≥45 μg/dL with a venous specimen processed as an emergency test unless symptoms of encephalopathy are present. • Obtain an abdominal x-ray to look for lead solid ingestion; if radio-opaque particles are found or recent ingestion is witnessed, use a cathartic. • Arrange hospitalization and chelation therapy at a facility with expertise in treating lead-poisoned children. • Provide chelation therapy in, and discharge child to, a lead-safe environment. Do not discharge until the NYC Health Department inspects the home. • Inform the NYC Health Department of the hospital admission by calling 646-632-6002. The Health Department can provide referrals to providers with expertise in treating lead intoxication and referrals to temporary lead-safe housing. Chelation Therapy For Children with Venous BLLs ≥45 μg/dL1 BLL (μg/dL) Agent, Dosage,* and Administration Special Considerations Follow-up <45 Chelation therapy not routinely recommended See Reverse for Recommended Follow-up Blood Lead Test Schedule for Children 45 to <70 • DMSA (succimer, 2,3-meso-dimercaptosuccinic acid) • Monitor for anemia, • Schedule weekly health care visits • 1050 mg DMSA / m2 / 24 hours* ÷ q8 hours PO x neutropenia, and to monitor compliance and signs of toxicity. 5 days; round dose to nearest 100 mg/day, and then hepatic toxicity. • Monitor BLLs weekly until level stabilizes, ÷ 100-mg capsules as evenly as possible for q8-hour then follow Recommended Follow-up dosing schedule. -

Effect of Chromium(VI) on Serum Iron and Removal of Its Toxicity by Combining Deferasirox and Deferiprone Chelators in Rats
American Journal of Pharmacology and Toxicology 8 (4): 164-169, 2013 ISSN: 1557-4962 ©2013 Science Publication doi:10.3844/ajptsp.2013.164.169 Published Online 8 (4) 2013 (http://www.thescipub.com/ajpt.toc) Effect of Chromium(VI) on Serum Iron and Removal of its Toxicity by Combining Deferasirox and Deferiprone Chelators in Rats 1S. Jamil A. Fatemi, 1Marzieh Iranmanesh and 2Faezeh Dahooee Balooch 1Department of Chemistry, Faculty of Sciences, Islamic Azad University, Kerman Branch, Kerman, Iran 2Department of Chemistry, Faculty of Sciences, Shahid Bahonar University of Kerman, Kerman, Iran Received 2013-09-26, Revised 2013-10-21; Accepted 2013-10-30 ABSTRACT The present research is aimed to characterize the potential efficiency of two chelators after chromium(VI) administration for 60 days following two doses of 15 and 30 mg kg −1 chromium(VI) per body weight daily to male rats. However, the hypothesis that the two chelators might be more efficient as combined therapy than as single therapy in removing chromium(VI) from bood serum was considered. In this way, two known chelators deferasirox and deferiprone were chosen and tested in the acute rat model. Two chelators were given orally as a single or combined therapy for a period of one week. Chromium(VI) and iron concentrations in blood were determined by flame atomic absorption spectroscopy method. Chromium is one of the most widely used industrial metals. Several million workers worldwide are estimated to be exposed to chromium compounds in an array of industries. Chromium(VI) is more readily absorbed by both inhalation and oral routes. Ingestion of large amounts of chromium(VI) can lead to severe respiratory, cardiovascular, gastrointestinal, hepatic and renal damage and potentially death. -

Renal Papillary Necrosis in Infancy PETER HUSBAND* and K
Arch Dis Child: first published as 10.1136/adc.48.2.116 on 1 February 1973. Downloaded from Archives of Disease in Childhood, 1973, 48, 116. Renal papillary necrosis in infancy PETER HUSBAND* and K. A. HOWLETT From the Departments of Paediatrics and Radiology, Charing Cross Group of Hospitals, Fulham Hospital, London Husband, P., and Howlett, K. A. (1973). Archives of Disease in Childhood, 48, 116. Renal papillary necrosis in infancy. Two infants developed renal papillary necrosis after acute illnesses associated with dehydration. After a short oliguric phase there was a longer phase characterized by impaired urinary concen- tration, hyponatraemia, metabolic acidosis, and a raised blood urea. Intravenous urograms showed contrast collecting in the papillae, with subsequent sinus formation extending into the medulla. In one case impaired urinary concentration was still present 21 months after the initial illness. Renal papillary necrosis was originally described admitted to hospital 9 days later after he had been by Friedreich (1877) in a man aged 70 years. found in his cot, grey, with respiratory distress and a Since then the majority of further cases reported high temperature. 3 days before he had diarrhoea and have also been in adults. It has been thought to vomiting for 24 hours but subsequently tolerated feeds be uncommon and usually to have a fatal outcome of full cream Cow and Gate milk, 180 ml 5 times a day. He was again extremely ill: temperature 40 3 °C, pale, copyright. in infancy and childhood (Davies, Kennedy, and cyanosed with a rapid respiratory rate, but not dehydra- Roberts, 1969). In the newborn infant renal ted. -

Path Renal Outline
Path Renal Outline Krane’s Categorization of Disease + A lot of Extras Kidney Disease Acute Renal Failure Intrinsic Kidney Disease Pre‐Renal Renal Intrinsic Post‐Renal Sodium Excretion <1% Glomerular Disease Tubulointerstitial Disease Sodium Excretion < 1% Sodium Excretion >2% Labs aren’t that useful BUN/Creatinine > 20 BUN/Creatinine < 10 CHF, Cirrhosis, Edema Urinalysis: Proteinuria + Hematuria Benign Proteinuria Spot Test Ratio >1.5, Spot Test Ratio <1.5, Acute Tubular Acute Interstitial Acute 24 Urine contains > 2.0g/24hrs 24 Urine contains < 1.0g/24hrs Necrosis Nephritis Glomerulonephritis Nephrotic Syndrome Nephritic Syndrome Inability to concentrate Urine RBC Casts Dirty Brown Casts Inability to secrete acid >3.5g protein / 24 hrs (huge proteinuria) Hematuria and Proteinuria (<3.5) Sodium Excretion >2% Edema Hypoalbuminemia RBC Casts Hypercholesterolemia Leukocytes Salt and Water Retention = HTN Focal Tubular Necrosis Edema Reduced GFR Pyelonephritis Minimal change disease Allergic Interstitial Nephritis Acute Proliferative Glomerulonephritis Membranous Glomerulopathy Analgesic Nephropathy Goodpasture’s (a form of RPGN) Focal segmental Glomerulosclerosis Rapidly Progressive Glomerulonephritis Multiple Myeloma Post‐Streptococcal Glomerulonephritis Membranoproliferative Glomerulonephritis IgA nephropathy (MPGN) Type 1 and Type 2 Alport’s Meleg‐Smith’s Hematuria Break Down Hematuria RBCs Only RBC + Crystals RBC + WBC RBC+ Protein Tumor Lithiasis (Stones) Infection Renal Syndrome Imaging Chemical Analysis Culture Renal Biopsy Calcium -

Acute Tubular Necrosıs After Nephrectomy: Case Presentatıon
Case Report JOJ Case Stud Volume 7 Issue 1 - May 2018 Copyright © All rights are reserved by Ebru Canakci DOI: 10.19080/JOJCS.2018.07.555703 Acute Tubular Necrosıs after Nephrectomy: Case Presentatıon Ebru Canakci1*, Ahmet Karatas2, Ahmet Gultekin1, Zubeyir Cebeci1, Ilker Coskun1 and Anıl Kılınc1 1Department of Anaesthesiology and Reanimation, Ordu University, Turkey 2Department of Internal Medicine & Nephrology, Ordu University, Turkey Submission: May 07, 2018; Published: May 18, 2018 *Corresponding author: Ebru Canakci, Faculty of Medicine, Department of Anaesthesiology and Reanimation, Ordu University, Ordu, Turkey, Email: Abstract ATN, contrary to prerenal azotemia, is not immediately cured upon the recovery of renal perfusion. In its severe form, renal hypoperfusion leads Acute renal failure (ARF) has a clinical presentation with declining renal function and glomerular filtration rate within hours-days. Ischemic trauma, severe hypovolemia, sepsis and severe burns. Acute kidney injury (AKI) is one of the frequently encountered causes of morbidity and mortalityto bilateral in renal hospitals. cortical The necrosis aim of this and study irreversible is to present renal the insufficiency. case with ATN Ischemic after major ATN often surgery develops and subsequent as a result permanent of major surgical kidney injuryintervention, in light of the information from the literature. Keywords: Nephrectomy; Acute Tubular Necrosis; Hemodialysis Introductıon and Objectıve to endogenous or exogenous toxins. Toxins cause intrarenal Acute renal failure (ARF) has a clinical presentation with vasoconstriction, direct tubular toxicity and/or intratubular obstruction and thus lead to ARF [4]. Acute kidney injury (AKI) hours-days. Although there are several differences in the declining renal function and glomerular filtration rate within is one of the frequently encountered causes of morbidity and mortality in hospitals. -
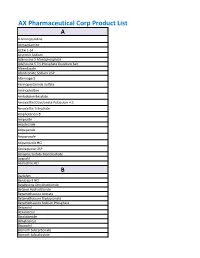
AX Pharmaceutical Corp Product List
AX Pharmaceutical Corp Product List A 4-Aminopyridine Acetazolamine ACTH 1-24 Acyclovir Sodium Adenosine 5 Monophosphate Adenosine 5 Tri-Phosphate Disodium Salt Albendazole Alendronate Sodium USP Alternogest Aminopentamide Sulfate Aminophylline Amlodipine Besylate Amoxicillin/Clavulanate Potassium 4:1 Amoxicillin Trihydrate Amphotericin B Ampicillin Anastrozole Aripepazole Aripiprazole Atipamezole HCl Atovaquone USP Atropine Sulfate Monohydrate Avanafil Azelastine HCl B Baclofen Benazepril HCl Betahistine Dihydrochloride Betaine Hydrochloride Betamethasone Acetate Betamethasone Dipropionate Betamethasone Sodium Phosphate Betaxolol Bexarotene Bicalutamide Bimatoprost Bisacodyl Bismuth Subcarbonate Bismuth Subsalicylate Bleomycin A5 Hydrochloride Bleomycin Sulfate Bretylium Tosylate Brimonidine Brinzolamide Bromhexine Bromocriptine Mesylate Brompheniramine Maleate Budesonide Bumetanide Bupivacaine Base Bupivacaine Hydrochloride Buprenorphine Bupropion HCl Buspirone Hydrochloride Busulfan Butaphosphan Butylated Hydroxyanisole C Cabergoline Calamine Calcium Glycerophosphate Calcium Levulinate Dihydrate Capsaicin Captopril Carbamazepine Carbazochrome Carbenoxolone Carbetocin Acetate Carbidopa Carbocisteine Carboplatin Carmustine Carprofen Carvedilol Cefadroxil Hemihydrate Cefadroxil Monohydrate Cefazolin Cefazolin Sodium Cefdinir Cefotaxime Cefotetan Disodium Cefpodoxime Cefpodoxime Proxetil Ceftazidime Ceftiofur Free Acid Ceftiofur Sodium Ceftriaxone Cefuroxime (Ceftin) Celecoxib Cephalexin Base Cephalexin Monohydrate Cesium Chloride Cetirizine -

Effects of Bodybuilding Supplements on the Kidney
Ali et al. BMC Nephrology (2020) 21:164 https://doi.org/10.1186/s12882-020-01834-5 RESEARCH ARTICLE Open Access Effects of bodybuilding supplements on the kidney: A population-based incidence study of biopsy pathology and clinical characteristics among middle eastern men Alaa Abbas Ali1, Safaa E. Almukhtar2†, Dana A. Sharif3†, Zana Sidiq M. Saleem4†, Dana N. Muhealdeen1 and Michael D. Hughson1* Abstract Background: The incidence of kidney diseases among bodybuilders is unknown. Methods: Between January 2011 and December 2019, the Iraqi Kurdistan 15 to 39 year old male population averaged 1,100,000 with approximately 56,000 total participants and 25,000 regular participants (those training more than 1 year). Annual age specific incidence rates (ASIR) with (95% confidence intervals) per 100,000 bodybuilders were compared with the general age-matched male population. Results: Fifteen male participants had kidney biopsies. Among regular participants, diagnoses were: focal segmental glomerulosclerosis (FSGS), 2; membranous glomerulonephritis (MGN), 2; post-infectious glomeruonephritis (PIGN), 1; tubulointerstitial nephritis (TIN), 1; and nephrocalcinosis, 2. Acute tubular necrosis (ATN) was diagnosed in 5 regular participants and 2 participants training less than 1 year. Among regular participants, anabolic steroid use was self- reported in 26% and veterinary grade vitamin D injections in 2.6%. ASIR for FSGS, MGN, PIGN, and TIN among regular participants was not statistically different than the general population. ASIR of FSGS adjusted for anabolic steroid use was 3.4 (− 1.3 to 8.1), a rate overlapping with FSGS in the general population at 2.0 (1.2 to 2.8). ATN presented as exertional muscle injury with myoglobinuria among new participants. -

Tubular Proteinuria Defined by a Study of Dent's
Kidney International, Vol. 57 (2000), pp. 240±249 Tubular proteinuria de®ned by a study of Dent's (CLCN5 mutation) and other tubular diseases ANTHONY G.W. NORDEN,STEVEN J. SCHEINMAN,MONIQUE M. DESCHODT-LANCKMAN, MARTA LAPSLEY,JOEÈ LLE L. NORTIER,RAJESH V. THAKKER,ROBERT J. UNWIN, and OLIVER WRONG Department of Chemical Pathology, Chase Farm Hospital, Barnet and Chase Farm Hospitals NHS Trust, En®eld, Middlesex, England, United Kingdom; Department of Medicine, State University of New York Health Science Center, Syracuse, New York, USA; Laboratoire de Recherche sur le Metabolisme des Peptides and Nephrology Department, Erasme Hospital, Brussels, Belgium; Nuf®eld Department of Medicine, John Radcliffe Hospital, Headington, Oxford, and Center for Nephrology, Royal Free and University College London Medical School, University College London, London, England, United Kingdom Tubular proteinuria de®ned by a study of Dent's (CLCN5 The term ªtubular proteinuriaº has been applied to mutation) and other tubular diseases. an electrophoretic pattern of urine proteins found in Background. The term ªtubular proteinuriaº is often used patients with chronic proximal renal tubular disease interchangeably with ªlow molecular weight proteinuriaº (LMWP), although the former implies a de®nite etiology. A [1, 2]. This pattern of proteins represents increased excre- speci®c quantitative de®nition of tubular proteinuria is needed, tion of several low molecular weight (LMW) proteins, and we address this by studying ®ve different renal disorders. as well as albumin