Critical Medicines List (PDF 745KB)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Idarucizumab Reverses Dabigatran Anticoagulant Activity in Healthy Chinese Volunteers: a Pharmacokinetics, Pharmacodynamics, and Safety Study
Adv Ther (2020) 37:3916–3928 https://doi.org/10.1007/s12325-020-01439-2 ORIGINAL RESEARCH Idarucizumab Reverses Dabigatran Anticoagulant Activity in Healthy Chinese Volunteers: A Pharmacokinetics, Pharmacodynamics, and Safety Study Zining Wang . Xia Zhao . Pengkang He . Shuqing Chen . Jie Jiang . Akiko Harada . Steven Brooks . Yimin Cui Received: May 25, 2020 / Published online: July 20, 2020 Ó The Author(s) 2020 ABSTRACT b.i.d., oral). After a washout period, the 12 subjects again received dabigatran etexilate Introduction: Idarucizumab is a humanized (220 mg b.i.d., oral) and idarucizumab monoclonal antibody fragment that specifically (2.5 ? 2.5 g, intravenous) 2 h after the last binds to dabigatran with high affinity and administration of dabigatran etexilate. reverses its anticoagulant effect. This study Results: The geometric mean (gMean) values of investigated the pharmacokinetics (PK) and area under the plasma concentration–time pharmacodynamics (PD) of idarucizumab in curve (AUC0–?) and maximum concentration healthy Chinese subjects at steady state of (Cmax) were 44,200 nmol h/L and 30,900 nmol/ dabigatran and explored the effect of idaru- L, respectively. An amount of 35.3 lmol of cizumab on PK and PD of dabigatran. idarucizumab, corresponding to 33.8% of the Methods: Twelve subjects received dabigatran total dose, was excreted by urine over 72 h. The etexilate treatment alone (220 mg twice daily, area under the effect (AUECabove,2–12) in the presence and absence of idarucizumab was close to zero for all coagulation parameters, diluted Zining Wang and Xia Zhao contributed equally to this work. thrombin time (dTT), ecarin clotting time (ECT), activated partial thromboplastin time Digital Features To view digital features for this article (aPTT), and thrombin time (TT), which indi- go to https://doi.org/10.6084/m9.figshare.12613334. -

Reversal of Oral Anticoagulation in Patients with Acute Intracerebral Hemorrhage Joji B
Kuramatsu et al. Critical Care (2019) 23:206 https://doi.org/10.1186/s13054-019-2492-8 REVIEW Open Access Reversal of oral anticoagulation in patients with acute intracerebral hemorrhage Joji B. Kuramatsu* , Jochen A. Sembill and Hagen B. Huttner Abstract In light of an aging population with increased cardiovascular comorbidity, the use of oral anticoagulation (OAC) is steadily expanding. A variety of pharmacological alternatives to vitamin K antagonists (VKA) have emerged over recent years (direct oral anticoagulants, DOAC, i.e., dabigatran, rivaroxaban, apixaban, and edoxaban) which show a reduced risk for the occurrence of intracerebral hemorrhage (ICH). Yet, in the event of ICH under OAC (OAC-ICH), hematoma characteristics are similarly severe and clinical outcomes likewise substantially limited in both patients with VKA- and DOAC-ICH, which is why optimal acute hemostatic treatment in all OAC-ICH needs to be guaranteed. Currently, International Guidelines for the hemostatic management of patients with OAC-ICH are updated as several relevant large-sized observational studies and recent trials have established treatment approaches for both VKA- and DOAC-ICH. While the management of VKA-ICH is mainly based on the immediate reversal of elevated levels of international normalized ratio using prothrombin complex concentrates, hemostatic management of DOAC-associated ICH is challenging requiring specific antidotes, notably idarucizumab and andexanet alfa. This review will provide an overview of the latest studies and trials on hemostatic reversal agents and timing and summarizes the effects on hemorrhage progression and clinical outcomes in patients with OAC-ICH. Keywords: Intracerebral hemorrhage, Anticoagulation reversal, Tranexamic acid, Ciraparantag, Desmopressin Introduction importantly have a greater frequency of hematoma ex- Of all stroke sub-types, intracerebral hemorrhage (ICH) pansion (HE), all of which are significant outcome pre- constitutes roughly 15% and is associated with the worst dictors determining an even poorer prognosis [11–13]. -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD August 2016 CONTENTS General Toxicology 6 Metals 30 Management 14 Pesticides 31 Drugs 16 Chemical Warfare 33 Chemical Incidents & 24 Plants 34 Pollution Chemicals 25 Animals 34 CURRENT AWARENESS PAPERS OF THE MONTH Toxicity evaluation of α-pyrrolidinovalerophenone (α-PVP): results from intoxication cases within the STRIDA project Beck O, Franzén L, Bäckberg M, Signell P, Helander A. Clin Toxicol 2016; 54: 568-75. Context An increasing number of new psychoactive substances (NPS) of different chemical classes have become available through marketing and sale over the Internet. This report from the Swedish STRIDA project presents the prevalence, laboratory results, and clinical features in a series of intoxications involving the stimulant NPS -pyrrolidinovalerophenone (-PVP), a potent dopamine re-uptake inhibitor, over a 4-year period. Study design Observational case series of consecutive patients with admitted or suspected intake of NPS presenting to hospitals in Sweden from 2012 to 2015. Patients and methods In the STRIDA project, blood and urine samples are collected from intoxicated patients with admitted or suspected intake of NPS or unknown drugs presenting to hospitals over the country. Analysis of NPS is performed by mass spectrometry multicomponent methods. Clinical data are collected when caregivers consult the Swedish Poisons Information Centre Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England 2 (PIC), and retrieved from medical records. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Review of Succimer for Treatment of Lead Poisoning
Review of Succimer for treatment of lead poisoning Glyn N Volans MD, BSc, FRCP. Department of Clinical Pharmacology, School of Medicine at Guy's, King's College & St Thomas' Hospitals, St Thomas' Hospital, London, UK Lakshman Karalliedde MB BS, DA, FRCA Consultant Medical Toxicologist, CHaPD (London), Health Protection Agency UK, Visiting Senior Lecturer, Division of Public Health Sciences, King's College Medical School, King's College , London Senior Research Collaborator, South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, Peradeniya, Sri Lanka. Heather M Wiseman BSc MSc Medical Toxicology Information Services, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 9RT, UK. Contact details: Heather Wiseman Medical Toxicology Information Services Guy’s & St Thomas’ NHS Foundation Trust Mary Sheridan House Guy’s Hospital Great Maze Pond London SE1 9RT Tel 020 7188 7188 extn 51699 or 020 7188 0600 (admin office) Date 10th March 2010 succimer V 29 Nov 10.doc last saved: 29-Nov-10 11:30 Page 1 of 50 CONTENTS 1 Summary 2. Name of the focal point in WHO submitting or supporting the application 3. Name of the organization(s) consulted and/or supporting the application 4. International Nonproprietary Name (INN, generic name) of the medicine 5. Formulation proposed for inclusion 6. International availability 7. Whether listing is requested as an individual medicine or as an example of a therapeutic group 8. Public health relevance 8.1 Epidemiological information on burden of disease due to lead poisoning 8.2 Assessment of current use 8.2.1 Treatment of children with lead poisoning 8.2.2 Other indications 9. -

Oral Anticoagulants
4/26/2018 Disclosure • Kelsey Gander, PharmD, BCACP Direct Oral Anticoagulants: – Declares no financial relationships pertinent to this session When to Use and How to Choose – Declares off-label use of medication will not be discussed during this presentation. Kelsey Gander, PharmD, BCACP Minnesota Academy of Physician Assistants Conference May 11th, 2018 Abbreviations Objectives • DOAC= direct oral anticoagulant 1) Compare and contrast the efficacy and safety • VTE= venous thromboembolism • DVT= deep vein thrombosis of direct oral anticoagulants (DOACs) to • PE= pulmonary embolism warfarin • A-fib, AF= atrial fibrillation 2) Identify which anticoagulant would be most • ESRD= end stage renal disease appropriate for a given patient • ACC= American College of Cardiology • AHA= American Heart Association 3) Recognize when it would not be appropriate • HRS= Heart Rhythm Society to use a DOAC • BID= twice daily Appropriate Abbreviations Patient Case JJ is a 66 y/o male who was hospitalized for pulmonary • NOAC embolism and initiated on anticoagulant therapy one week – Novel Oral Anticoagulant ago. – Chief complaint: – Non-Vitamin K Oral Anticoagulant • Presents to clinic today for INR check, post-hospital discharge follow- up • TSOAC – Past medical history: • Hypertension, hyperlipidemia, osteoarthritis, erectile dysfunction, – Target Specific Oral Anticoagulant BPH, type 2 diabetes, peripheral artery disease – Home medications • DOAC • Acetaminophen 650mg po every 6 hours PRN – Direct Oral Anticoagulant • Diazepam 5mg po at bedtime PRN anxiety -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -
RCEM NPIS Antidote Guideline Appx 1
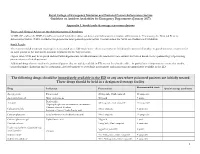
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

WO 2014/195872 Al 11 December 2014 (11.12.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/195872 Al 11 December 2014 (11.12.2014) P O P C T (51) International Patent Classification: (74) Agents: CHOTIA, Meenakshi et al; K&S Partners | Intel A 25/12 (2006.01) A61K 8/11 (2006.01) lectual Property Attorneys, 4121/B, 6th Cross, 19A Main, A 25/34 (2006.01) A61K 8/49 (2006.01) HAL II Stage (Extension), Bangalore 560038 (IN). A01N 37/06 (2006.01) A61Q 5/00 (2006.01) (81) Designated States (unless otherwise indicated, for every A O 43/12 (2006.01) A61K 31/44 (2006.01) kind of national protection available): AE, AG, AL, AM, AO 43/40 (2006.01) A61Q 19/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A01N 57/12 (2006.01) A61K 9/00 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, AOm 59/16 (2006.01) A61K 31/496 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, PCT/IB20 14/06 1925 KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (22) International Filing Date: OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, 3 June 2014 (03.06.2014) SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, (25) Filing Language: English TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

Chelating Drug Therapy: an Update
Open Access Austin Journal of Genetics and Genomic Research Review Article Chelating Drug Therapy: An Update Vijay Kumar1, Ashok Kumar2*, Sandeep Kumar Singh1, Manoj Kumar3, Surendra Kumar2, Dinesh Abstract 4 5 Kumar and Ragni Singh Purpose: To study the clinical effects of metal toxicity and current 1Department of Neurology, SGPGIMS, India recommendations for management, including chelation therapy, are reviewed. 2Department of Medical Genetics, SGPGIMS, India 3Department of Microbiology, SGPGIMS, India Summary: Metals are essential to many biological processes, but excess 4Department of Chemistry, Dr. R.M.L. Avadh University, of it becomes hazardous to life. These are necessary for cell growth, electron India transport chain, several enzymatic activities and response of immune systems. 5Bheem Rao Ambedkar Bihar University, India They also serve as a cofactor for several enzymes. Chelation therapy is used for clinical management of the excess of metal. However, each metal requires *Corresponding author: Ashok Kumar, Department a specific chelation agent. A chelate is a compound form between metal and a of Medical Genetics, Sanjay Gandhi Post Graduate compound that contains two or more potential ligands. A promising Fe chelator Institute of Medical Sciences, Lucknow, India is Desferrioxamine (Desferal). Penicillamine and Trientine are uses for copper Received: March 12, 2015; Accepted: April 24, 2015; chelation. Meso-2,3-Dimercaptosuccinic Acid (DMSA) and 2,3-Dimercapto- Published: April 27, 2015 Propanesulphonate (DMPS) can be used as effective chelator of mercury. Dimercaprol, edetate calcium disodium, and succimer are the three agents primarily used for chelation of lead. Conclusion: Metal toxicity remains a significant public health concern. Elimination of elevated metal ions can be achieved by proper chelation agents. -

Changes in Tissue Gadolinium Biodistribution Measured in an Animal Model Exposed to Four Chelating Agents
Japanese Journal of Radiology (2019) 37:458–465 https://doi.org/10.1007/s11604-019-00835-1 ORIGINAL ARTICLE Changes in tissue gadolinium biodistribution measured in an animal model exposed to four chelating agents Türker Acar1,6 · Egemen Kaya2 · Mustafa Deniz Yoruk3 · Neslihan Duzenli4 · Recep Selim Senturk4 · Cenk Can4 · Lokman Ozturk3 · Canberk Tomruk5 · Yigit Uyanikgil5 · Frank J. Rybicki6 Received: 17 December 2018 / Accepted: 22 March 2019 / Published online: 30 March 2019 © Japan Radiological Society 2019 Abstract Purpose This study investigated the potential to reduce gadolinium levels in rodents after repetitive IV Gadodiamide admin- istration using several chelating agents. Materials and methods The following six groups of rats were studied. Group 1: Control; Group 2: Gadodiamide only; Group 3: Meso-2,3-Dimercaptosuccinic acid (DMSA) + Gadodiamide; Group 4: N-Acetyl-L-cysteine (NAC) + Gadodiamide; Group 5: Coriandrum sativum extract + Gadodiamide; and Group 6: Deferoxamine + Gadodiamide. Brain, kidney, and blood samples were evaluated via inductively coupled plasma mass spectrometry. The brain was also evaluated histologically. Results Kidney gadolinium levels in Groups 4 and 5 were approximately double that of Group 2 (p = 0.033 for each). There was almost no calcifcation in rat hippocampus for Group 4 rodents when compared with Groups 2, 3, 5 and 6. Conclusion Our preliminary study shows that excretion to the kidney has a higher propensity in NAC and Coriandrum sati- vum groups. It may be possible to change the distribution of gadolinium by administrating several agents. NAC may lower Gadodiamide-induced mineralization in rat hippocampus. Keywords Gadolinium deposition · Dimercaptosuccinic acid · N-Acetyl-L-cysteine · Coriandrum sativum · Deferoxamine Introduction However, the safety profle of gadolinium-based agents [1] was questioned after the discovery of nephrogenic sys- Gadolinium-based contrast agents (GBCA) have been safely temic fbrosis [2], a scleroderma-like disease characterized used in diagnostic radiology since the 1980s.