Post Penicillin Antibiotics: from Acceptance to Resistance?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Derivatives of Clavulanic Acid, Process for Their Preparation And
Europaisches Patentamt © ê European Patent Office © Publication number: 0 003 254 Office européen des brevets Bl © EUROPEAN PATENT SPECIFICATION (45) Date of publication of patent spécification: 28.03.84 © Int. ci.3: C 07 D 498/04, A 61 K 31/42, @ Application number: 78300762.8 A 61 K 31/43, @ Date offiling: 07.12.78 A 61 K 31/545 //(C07D498/04, 263/00, 205/00), (A6 1 K3 1 /43, 3 1/42), (A61K3 1/545, 31/42) (54) Derivatives of clavulanic acid, process for their préparation and compositions containing them. (§) Priority: 26.01 .78 GB 312978 @ Proprietor: BEECHAM GROUP PLC Beecham House Great West Road Brentford Middlesex (GB) (43) Date of publication of application: 08.08.79 Bulletin 79/1 6 @ Inventor: Gasson, Brian Charles 9, Clarence Walk (45) Publication of the grant of the patent: Redhill Surrey (GB) 28.03.84 Bulletin 84/13 © Représentative: Hesketh, Alan, Dr. et al, (84) Designated Contracting States: European Patent Attorney Beecham BE CH DEFRGBITNL Pharmaceuticals Great Burgh Yew Tree Bottom Road Epsom, Surrey, KT18 5XQ (GB) (56) Références cited: BE - A - 847 046 The file contains technical information submitted after the application was filed and not included in this spécification Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. Notice of opposition shall be filed in a written reasoned statement. It shall not be deemed to have been filed until the opposition fee has been paid. -

Reviews ~-Medical Journal Books Received
JUNEJUNE24,L'+,1961 REVIEWS REVIEWS BRITISH 1813 ~-MEDICAL JOURNAL under the Presidency of Sir Charles Dodds. It was the Th2e Medical Register I96I. Parts 1 and 2. (Pp. 3,111 +xxiv.) first joint meeting between the British Society of London: The General Medical Council, 44 Hallam Street, W.i. Enclocrinology and the societies representing the Acta 1961. A Prelude to Medical History. By Felix Marti-lbifiez, Endocrinologica Congresses. M.D. (Pp. 253 +xix. $5.75.) New York: MD Publications, About two-thirds of the papers reported are included Inc. 1961. in four symposia. The first three, on " Neuroendo- The Mantagement ofPediatric Practice. By Hugh C. Thompson, crinology," " Thyroid Gland," and " Parathyroid M.D., and Joseph B. Seagle, M.S., M.D. (Pp. 172+xv; illUs- CGlands," make up Volume 9 (Part I). Volume 10 trated. 60s.) Springfield, Illinois: Charles C. Thomas. Oxford: (Part I1) includes the fourth symposium entitled "Are Blackwell Scientific Publications. 1961. the Endocrine Glands directly related to Cancer ? Par-ents of the Handicapped. Self. Organied Parents' adl Re!atives' Groutps for Treatmenzt of Ill anzd Hanydicappced and the remaining papers grouped under the headings Children. By Alfred H. Katz, D.S.W. (Pp. 155+ix. 48s.) " Steroid Biochemistry " and " Biological Actions and Springfield, Illinois: Charles C. Thomas. Oxford: Blackwell Interrelationships of Steroids and other Hormones." Scientific Publications. 1961. The symposia deal mainly with growing points and Thought Refo.rm and the Psychology, of Totalism. A Study oj give a representative picture of recent European "Brainwashing" in China. By Robert Lifton, M.D. (Pp. 510 achievements in these sectors of endocrinology. -

Haemophilia: Recent History of Clinical Management
HAEMOPHILIA: RECENT HISTORY OF CLINICAL MANAGEMENT The transcript of a Witness Seminar held at the Wellcome Institute for the History of Medicine, London, on 10 February 1998 Edited by D A Christie and E M Tansey HAEMOPHILIA: RECENT HISTORY OF CLINICAL MANAGEMENT Participants Dr Derek Bangham Professor Ilsley Ingram Dr Ethel Bidwell Dr Peter Jones Sir Christopher Booth Professor Christine Lee (Chair) Dr Brian Colvin Dr James Matthews Dr Angela Dike Mrs Riva Miller Mr Ross Dike Dr Charles Rizza Dr Helen Dodsworth Rev Alan Tanner Professor Stuart Douglas* Dr Tilli Tansey Professor Robert Duthie Professor Edward Tuddenham Dr David Evans Dr David Tyrrell Dr Sheila Howarth Mr Clifford Welch Others present at the meeting: Dr Trevor Barrowcliffe, Ms Jacqui Marr, Dr J K Smith, Miss Rosemary Spooner Apologies: Professor Jean-Pierre Allain, Dr Donald Bateman, Dr Rosemary Biggs, Mrs Peggy Britten,** Professor Judith Chessells, Dr Audrey Dawson, Mr Ron Hutton, Professor Ralph Kekwick, Professor Sir David Weatherall *Deceased 15 November 1998 **Deceased 1 March 1999 2 Haemophilia: Recent history Professor Christine Lee:1 I think haemophilia is one of the best areas of clinical medicine where we have seen a very rapid introduction of scientific discovery into clinical practice. All of us who work on haemophilia realize that this has gone on very much with cooperation between the patients and the scientists and the doctors. I first saw haemophilia in 1967 when I was a medical student in Oxford and we were doing our orthopaedics at the Nuffield Orthopaedic Hospital. I have a very clear memory of a ward of little boys with their legs strung up, their arms strung up, and I think there was a schoolroom nearby. -

Clinical Pharmacology in the UK, C. 1950–2000: Industry and Regulation
CLINICAL PHARMACOLOGY IN THE UK, c. 1950–2000: INDUSTRY AND REGULATION The transcript of a Witness Seminar held by the Wellcome Trust Centre for the History of Medicine at UCL, London, on 25 September 2007 Edited by L A Reynolds and E M Tansey Volume 34 2008 ©The Trustee of the Wellcome Trust, London, 2008 First published by the Wellcome Trust Centre for the History of Medicine at UCL, 2008 The Wellcome Trust Centre for the History of Medicine at UCL is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 085484 118 9 All volumes are freely available online at: www.history.qmul.ac.uk/research/modbiomed/wellcome_witnesses/ Please cite as: Reynolds L A, Tansey E M. (eds) (2008) Clinical Pharmacology in the UK c.1950-2000: Industry and regulation. Wellcome Witnesses to Twentieth Century Medicine, vol. 34. London: Wellcome Trust Centre for the History of Medicine at UCL. CONTENTS Illustrations and credits v Abbreviations vii Witness Seminars: Meetings and publications; Acknowledgements E M Tansey and L A Reynolds ix Introduction Professor Parveen Kumar xxiii Transcript Edited by L A Reynolds and E M Tansey 1 References 73 Biographical notes 89 Glossary 103 Index 109 ILLUSTRATIONS AND CREDITS Figure 1 AstraZeneca Clinical Trials Unit, South Manchester. Reproduced by permission of AstraZeneca. 6 Figure 2 A summary of the organization of clinical trials. Adapted from www.clinicaltrials.gov/ct2/info/glossary (visited 1 May 2008). 10 Figure 3 Clinical trial certificates (CTC) and clinical trial exemption (CTX), 1972–1985. Adapted from Speirs (1983) and Speirs (1984). -

Harper, Peter: Transcript of a Video Interview (06-Jun-2015)
History of Modern Biomedicine Research Group School of History, Queen Mary University of London Mile End Road, London E1 4NS website: www.histmodbiomed.org VIDEO INTERVIEW TRANSCRIPT Harper, Peter: transcript of a video interview (06-Jun-2015) Interviewer: Tilli Tansey Transcriber: Debra Gee Editors: Tilli Tansey, Alan Yabsley Date of publication: 20-Mar-2017 Date and place of interview: 06-Jun-2015; Glasgow Publisher: Queen Mary University of London Collection: History of Modern Biomedicine Interviews (Digital Collection) Reference: e2017093 Number of pages: 4 DOI: 10.17636/01021439 Acknowledgments: The project management of Mr Adam Wilkinson is gratefully acknowledged. The History of Modern Biomedicine Research Group is funded by the Wellcome Trust, which is a registered charity (no. 210183). The current interview has been funded by the Wellcome Trust Strategic Award entitled “Makers of modern biomedicine: testimonies and legacy” (2012-2017; awarded to Professor Tilli Tansey). Citation: Tansey E M (intvr); Tansey E M, Yabsley A (eds) (2017) Harper, Peter: transcript of a video interview (06-Jun- 2015). History of Modern Biomedicine Interviews (Digital Collection), item e2017093. London: Queen Mary University of London. Related resources: items 2017094 - 2017099, History of Modern Biomedicine Interviews (Digital Collection) Note: Video interviews are conducted following standard oral history methodology, and have received ethical approval (reference QMREC 0642). Video interview transcripts are edited only for clarity and factual accuracy. Related material has been deposited in the Wellcome Library. © The Trustee of the Wellcome Trust, London, 2017 History of Modern Biomedicine Interviews (Digital Collection) - Harper, P e2017093 | 2 Harper, Peter: transcript of a video interview (06-Jun-2015)* Biography: Professor Peter Harper (b. -
RSC Branding
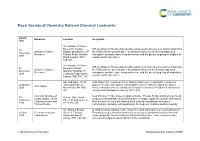
Royal Society of Chemistry National Chemical Landmarks Award Honouree Location Inscription Date The Institute of Cancer Research, Chester ICR scientists on this site and elsewhere pioneered numerous new cancer drugs from 10 Institute of Cancer Beatty Laboratories, 237 the 1950s until the present day – including the discovery of chemotherapy drug December Research Fulham Road, Chelsea carboplatin, prostate cancer drug abiraterone and the genetic targeting of olaparib for 2018 Road, London, SW3 ovarian and breast cancer. 6JB, UK The Institute of Cancer ICR scientists on this site and elsewhere pioneered numerous new cancer drugs from 10 Research, Royal Institute of Cancer the 1950s until the present day – including the discovery of chemotherapy drug December Marsden Hospital, 15 Research carboplatin, prostate cancer drug abiraterone and the genetic targeting of olaparib for 2018 Cotswold Road, Sutton, ovarian and breast cancer. London, SM2 5NG, UK Ape and Apple, 28-30 John Dalton Street was opened in 1846 by Manchester Corporation in honour of 26 October John Dalton Street, famous chemist, John Dalton, who in Manchester in 1803 developed the Atomic John Dalton 2016 Manchester, M2 6HQ, Theory which became the foundation of modern chemistry. President of Manchester UK Literary and Philosophical Society 1816-1844. Chemical structure of Near this site in 1903, James Colquhoun Irvine, Thomas Purdie and their team found 30 College Gate, North simple sugars, James a way to understand the chemical structure of simple sugars like glucose and lactose. September Street, St Andrews, Fife, Colquhoun Irvine and Over the next 18 years this allowed them to lay the foundations of modern 2016 KY16 9AJ, UK Thomas Purdie carbohydrate chemistry, with implications for medicine, nutrition and biochemistry. -

Robert Burns Woodward
The Life and Achievements of Robert Burns Woodward Long Literature Seminar July 13, 2009 Erika A. Crane “The structure known, but not yet accessible by synthesis, is to the chemist what the unclimbed mountain, the uncharted sea, the untilled field, the unreached planet, are to other men. The achievement of the objective in itself cannot but thrill all chemists, who even before they know the details of the journey can apprehend from their own experience the joys and elations, the disappointments and false hopes, the obstacles overcome, the frustrations subdued, which they experienced who traversed a road to the goal. The unique challenge which chemical synthesis provides for the creative imagination and the skilled hand ensures that it will endure as long as men write books, paint pictures, and fashion things which are beautiful, or practical, or both.” “Art and Science in the Synthesis of Organic Compounds: Retrospect and Prospect,” in Pointers and Pathways in Research (Bombay:CIBA of India, 1963). Robert Burns Woodward • Graduated from MIT with his Ph.D. in chemistry at the age of 20 Woodward taught by example and captivated • A tenured professor at Harvard by the age of 29 the young... “Woodward largely taught principles and values. He showed us by • Published 196 papers before his death at age example and precept that if anything is worth 62 doing, it should be done intelligently, intensely • Received 24 honorary degrees and passionately.” • Received 26 medals & awards including the -Daniel Kemp National Medal of Science in 1964, the Nobel Prize in 1965, and he was one of the first recipients of the Arthur C. -

St Catherine's College Oxford
MESSAGES The Year St Catherine’s College . Oxford 2013 ST CATHERINE’S COLLEGE 2013/75 MESSAGES Master and Fellows 2013 MASTER Susan C Cooper, MA (BA Richard M Berry, MA, DPhil Bart B van Es (BA, MPhil, Angela B Brueggemann, Gordon Gancz, BM BCh, MA Collby Maine, PhD California) Tutor in Physics PhD Camb) DPhil (BSc St Olaf, MSc Fellow by Special Election Professor Roger W Professor of Experimental Reader in Condensed Tutor in English Iowa) College Doctor Ainsworth, MA, DPhil, Physics Matter Physics Senior Tutor Fellow by Special Election in FRAeS Biological Sciences Geneviève A D M Peter R Franklin, MA (BA, Ashok I Handa, MA (MB BS Tommaso Pizzari, MA (BSc Wellcome Trust Career Helleringer (Maîtrise FELLOWS DPhil York) Lond), FRCS Aberd, PhD Shef) Development Fellow ESSEC, JD Columbia, Maîtrise Tutor in Music Fellow by Special Election in Tutor in Zoology Sciences Po, Maîtrise, Richard J Parish, MA, DPhil Professor of Music Medicine James E Thomson, MChem, Doctorat Paris-I Panthéon- (BA Newc) Reader in Surgery Byron W Byrne, MA, DPhil DPhil Sorbonne, Maîtrise Paris-II Tutor in French John Charles Smith, MA Tutor for Graduates (BCom, BEng Western Fellow by Special Election in Panthéon-Assas) Philip Spencer Fellow Tutor in French Linguistics Australia) Chemistry Fellow by Special Election Professor of French President of the Senior James L Bennett, MA (BA Tutor in Engineering Science in Law (Leave H14) Common Room Reading) Tutor for Admissions Andrew J Bunker, MA, DPhil Leverhulme Trust Early Fellow by Special Election Tutor in Physics -

Sir John Warcup Cornforth
Sir John Warcup Cornforth The degree of Doctor of Science (honoris causa) was conferred upon Sir John Warcup Cornforth at a ceremony held in the Great Hall on 2 November 1977. Sir John Warcup Cornforth, photo G3_224_1122, University of Sydney Archives. Citation A Nobel Prize-winning chemist who has been totally deaf for the past 40 years will be awarded the honorary degree of Doctor of Science by the University at a cemony in the Great Hall next Wednesday, November 2, 1977. He is Sir John Cornforth, 60, who was awarded the Nobel Prize for Chemistry in 1975 for his work on the stereochemistry of enzyme-catalysed reactions. He is currently the Royal Society Research Professor at the University of Sussex, and during his four-week visit to Australia he will deliver lectures in Sydney, Canberra, Melbourne and Adelaide. Sir John entered this University at the age of 16. The first signs of his deafness (from otosclerosis) had begun when he was 10, and although he had been able to profit from teaching at Sydney Boys' School, he was unable to hear any lecture at the University. He was, however, attracted by laboratory work in organic chemistry (which he had done in an improvised laboratory at home since the age of 14) and by the availability of original chemical literature. In 1937 he graduated with first-class honours and the University medal. After a year of postgraduate research he won a scholarship to work at Oxford. Two such scholarships were awarded each year, and the other was won by Rita Harradence, also of Sydney and also a winner of the University medal. -

Robert Burns Woodward 1917–1979
NATIONAL ACADEMY OF SCIENCES ROBERT BURNS WOODWARD 1917–1979 A Biographical Memoir by ELKAN BLOUT Any opinions expressed in this memoir are those of the author and do not necessarily reflect the views of the National Academy of Sciences. Biographical Memoirs, VOLUME 80 PUBLISHED 2001 BY THE NATIONAL ACADEMY PRESS WASHINGTON, D.C. ROBERT BURNS WOODWARD April 10, 1917–July 8, 1979 BY ELKAN BLOUT OBERT BURNS WOODWARD was the preeminent organic chemist Rof the twentieth century. This opinion is shared by his colleagues, students, and by other distinguished chemists. Bob Woodward was born in Boston, Massachusetts, and was an only child. His father died when Bob was less than two years old, and his mother had to work hard to support her son. His early education was in the Quincy, Massachusetts, public schools. During this period he was allowed to skip three years, thus enabling him to finish grammar and high schools in nine years. In 1933 at the age of 16, Bob Woodward enrolled in the Massachusetts Institute of Technology to study chemistry, although he also had interests at that time in mathematics, literature, and architecture. His unusual talents were soon apparent to the MIT faculty, and his needs for individual study and intensive effort were met and encouraged. Bob did not disappoint his MIT teachers. He received his B.S. degree in 1936 and completed his doctorate in the spring of 1937, at which time he was only 20 years of age. Immediately following his graduation Bob taught summer school at the University of Illinois, but then returned to Harvard’s Department of Chemistry to start a productive period with an assistantship under Professor E. -

Women Physiologists
Women physiologists: Centenary celebrations and beyond physiologists: celebrations Centenary Women Hodgkin Huxley House 30 Farringdon Lane London EC1R 3AW T +44 (0)20 7269 5718 www.physoc.org • journals.physoc.org Women physiologists: Centenary celebrations and beyond Edited by Susan Wray and Tilli Tansey Forewords by Dame Julia Higgins DBE FRS FREng and Baroness Susan Greenfield CBE HonFRCP Published in 2015 by The Physiological Society At Hodgkin Huxley House, 30 Farringdon Lane, London EC1R 3AW Copyright © 2015 The Physiological Society Foreword copyright © 2015 by Dame Julia Higgins Foreword copyright © 2015 by Baroness Susan Greenfield All rights reserved ISBN 978-0-9933410-0-7 Contents Foreword 6 Centenary celebrations Women in physiology: Centenary celebrations and beyond 8 The landscape for women 25 years on 12 "To dine with ladies smelling of dog"? A brief history of women and The Physiological Society 16 Obituaries Alison Brading (1939-2011) 34 Gertrude Falk (1925-2008) 37 Marianne Fillenz (1924-2012) 39 Olga Hudlická (1926-2014) 42 Shelagh Morrissey (1916-1990) 46 Anne Warner (1940–2012) 48 Maureen Young (1915-2013) 51 Women physiologists Frances Mary Ashcroft 56 Heidi de Wet 58 Susan D Brain 60 Aisah A Aubdool 62 Andrea H. Brand 64 Irene Miguel-Aliaga 66 Barbara Casadei 68 Svetlana Reilly 70 Shamshad Cockcroft 72 Kathryn Garner 74 Dame Kay Davies 76 Lisa Heather 78 Annette Dolphin 80 Claudia Bauer 82 Kim Dora 84 Pooneh Bagher 86 Maria Fitzgerald 88 Stephanie Koch 90 Abigail L. Fowden 92 Amanda Sferruzzi-Perri 94 Christine Holt 96 Paloma T. Gonzalez-Bellido 98 Anne King 100 Ilona Obara 102 Bridget Lumb 104 Emma C Hart 106 Margaret (Mandy) R MacLean 108 Kirsty Mair 110 Eleanor A. -

The Antibiotics Composition Comprising Beta-Lactam
(19) & (11) EP 2 062 581 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 153(4) EPC (43) Date of publication: (51) Int Cl.: 27.05.2009 Bulletin 2009/22 A61K 31/545 (2006.01) A61K 31/546 (2006.01) A61K 31/43 (2006.01) A61K 31/431 (2006.01) (2006.01) (2006.01) (21) Application number: 07785338.0 A61K 31/424 A61K 31/7036 A61K 47/18 (2006.01) A61K 47/12 (2006.01) (2006.01) (2006.01) (22) Date of filing: 14.08.2007 A61K 47/02 A61K 47/04 A61K 9/08 (2006.01) A61K 9/19 (2006.01) A61K 9/72 (2006.01) A61P 31/04 (2006.01) A61P 31/00 (2006.01) (86) International application number: PCT/CN2007/002438 (87) International publication number: WO 2008/025226 (06.03.2008 Gazette 2008/10) (84) Designated Contracting States: (71) Applicant: Tianjin Hemey Bio-Tech Co., Ltd. AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Tianjin 300457 (CN) HU IE IS IT LI LT LU LV MC MT NL PL PT RO SE SI SK TR (72) Inventor: ZHANG, Hesheng Designated Extension States: Tianjin 300457 (CN) AL BA HR MK RS (74) Representative: Hryszkiewicz, Danuta et al (30) Priority: 25.08.2006 CN 200610015437 Kancelaria Patentowa ul. Jana z Kolna 38 PL-75-204 Koszalin (PL) (54) THE ANTIBIOTICS COMPOSITION COMPRISING BETA-LACTAM ANTIBIOTICS AND IONIC CHELATING AGENTS (57) The antibiotics composition comprising at least tors and buffers simultaneously. The composition can be one of beta-lactam antibiotics and at least one of ionic formulated with at least one of aminoglycoside antibiotics chelating agents used for inhibiting particulate formation, into solution for controlling microbial infection in a con- further comprising at least one of beta-lactamase inhib- tainer.