Foot Axes and Angles
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skeletal Foot Structure
Foot Skeletal Structure The disarticulated bones of the left foot, from above (The talus and calcaneus remain articulated) 1 Calcaneus 2 Talus 3 Navicular 4 Medial cuneiform 5 Intermediate cuneiform 6 Lateral cuneiform 7 Cuboid 8 First metatarsal 9 Second metatarsal 10 Third metatarsal 11 Fourth metatarsal 12 Fifth metatarsal 13 Proximal phalanx of great toe 14 Distal phalanx of great toe 15 Proximal phalanx of second toe 16 Middle phalanx of second toe 17 Distal phalanx of second toe Bones of the tarsus, the back part of the foot Talus Calcaneus Navicular bone Cuboid bone Medial, intermediate and lateral cuneiform bones Bones of the metatarsus, the forepart of the foot First to fifth metatarsal bones (numbered from the medial side) Bones of the toes or digits Phalanges -- a proximal and a distal phalanx for the great toe; proximal, middle and distal phalanges for the second to fifth toes Sesamoid bones Two always present in the tendons of flexor hallucis brevis Origin and meaning of some terms associated with the foot Tibia: Latin for a flute or pipe; the shin bone has a fanciful resemblance to this wind instrument. Fibula: Latin for a pin or skewer; the long thin bone of the leg. Adjective fibular or peroneal, which is from the Greek for pin. Tarsus: Greek for a wicker frame; the basic framework for the back of the foot. Metatarsus: Greek for beyond the tarsus; the forepart of the foot. Talus (astragalus): Latin (Greek) for one of a set of dice; viewed from above the main part of the talus has a rather square appearance. -

Rethinking the Evolution of the Human Foot: Insights from Experimental Research Nicholas B
© 2018. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2018) 221, jeb174425. doi:10.1242/jeb.174425 REVIEW Rethinking the evolution of the human foot: insights from experimental research Nicholas B. Holowka* and Daniel E. Lieberman* ABSTRACT presumably owing to their lack of arches and mobile midfoot joints Adaptive explanations for modern human foot anatomy have long for enhanced prehensility in arboreal locomotion (see Glossary; fascinated evolutionary biologists because of the dramatic differences Fig. 1B) (DeSilva, 2010; Elftman and Manter, 1935a). Other studies between our feet and those of our closest living relatives, the great have documented how great apes use their long toes, opposable apes. Morphological features, including hallucal opposability, toe halluces and mobile ankles for grasping arboreal supports (DeSilva, length and the longitudinal arch, have traditionally been used to 2009; Holowka et al., 2017a; Morton, 1924). These observations dichotomize human and great ape feet as being adapted for bipedal underlie what has become a consensus model of human foot walking and arboreal locomotion, respectively. However, recent evolution: that selection for bipedal walking came at the expense of biomechanical models of human foot function and experimental arboreal locomotor capabilities, resulting in a dichotomy between investigations of great ape locomotion have undermined this simple human and great ape foot anatomy and function. According to this dichotomy. Here, we review this research, focusing on the way of thinking, anatomical features of the foot characteristic of biomechanics of foot strike, push-off and elastic energy storage in great apes are assumed to represent adaptations for arboreal the foot, and show that humans and great apes share some behavior, and those unique to humans are assumed to be related underappreciated, surprising similarities in foot function, such as to bipedal walking. -

5Th Metatarsal Fracture
FIFTH METATARSAL FRACTURES Todd Gothelf MD (USA), FRACS, FAAOS, Dip. ABOS Foot, Ankle, Shoulder Surgeon Orthopaedic You have been diagnosed with a fracture of the fifth metatarsal bone. Surgeons This tyPe of fracture usually occurs when the ankle suddenly rolls inward. When the ankle rolls, a tendon that is attached to the fifth metatarsal bone is J. Goldberg stretched. Because the bone is weaker than the tendon, the bone cracks first. A. Turnbull R. Pattinson A. Loefler All bones heal in a different way when they break. This is esPecially true J. Negrine of the fifth metatarsal bone. In addition, the blood suPPly varies to different I. PoPoff areas, making it a lot harder for some fractures to heal without helP. Below are D. Sher descriPtions of the main Patterns of fractures of the fifth metatarsal fractures T. Gothelf and treatments for each. Sports Physicians FIFTH METATARSAL AVULSION FRACTURE J. Best This fracture Pattern occurs at the tiP of the bone (figure 1). These M. Cusi fractures have a very high rate of healing and require little Protection. Weight P. Annett on the foot is allowed as soon as the Patient is comfortable. While crutches may helP initially, walking without them is allowed. I Prefer to Place Patients in a walking boot, as it allows for more comfortable walking and Protects the foot from further injury. RICE treatment is initiated. Pain should be exPected to diminish over the first four weeks, but may not comPletely go away for several months. Follow-uP radiographs are not necessary if the Pain resolves as exPected. -

Canine Tarsus Stabilization Surgical Technique 1 2
Canine Tarsus Stabilization Surgical Technique 1 2 Place the patient in a dorsal recumbent position and Make a medial incision beginning just proximal to the administer general anesthesia. Perform a hanging limb medial malleolus extending distally to the level of the technique with aseptic preparation and appropriate proximal intertarsal joint. Inspect the medial structures limb draping. of the tarsal joint. Identify the origin of the long part of the medial collateral ligament (MCL) on the medial malleolus of the tibia. 3 4 Using the aiming guide, place the 0.049 inch (1.2 mm) Use the 2.0 mm cannulated drill over the guidewire to guidewire from the origin of the long part of the MCL create the tibial bone tunnel for suture passage. in a proximal and slight cranial direction such that the it emerges on the lateral tibia just cranial to the fibula. Make a small incision on the lateral side where the guidewire tents the skin. 5 As a surgical landmark, identify the talocentral tarsal joint on the medial side by either a palpation or by inserting a small needle into the joint space. Using the aiming guide, place a 0.049 inch (1.2 mm) guidewire starting at the medial aspect of the talar head oriented parallel to the talocentral tarsal joint in a slightly plantar direction to capture the calcaneus. The guidewire should emerge just plantar to the boney tubercle of the lateral portion of the distal calcaneus. Make a small incision where the guidewire tents the skin. 6 7 Use the 2.0 mm cannulated drill over the guidewire to Identify the insertion of the short part of the MCL on the create the distal talus bone tunnel for suture passage. -

Equine MRI, Edited by Rachel C
Chapter 17 The p roximal t arsal r egion Rachel Murray , Natasha Werpy , Fabrice Audigi é , Jean - Marie Denoix , Matthew Brokken and Thorben Schulze INTRODUCTION Imaging of the proximal tarsus can be achieved in both standing and anaes- thetized horses. The height of the horse and the amount of hind end mus- culature determines which magnet confi guration will produce the best images of this region. A horse with short limbs and wide, well - muscled quarters may be more diffi cult to fi t into the long, narrow bore of some high - fi eld magnets under general anaesthesia. In the same way, the side of the lateral recumbency should be considered because it is generally easier to bring the proximal tarsus of the lower hind limb closer to the isocentre of the magnet compared with the upper one. Well developed hind limb musculature can prevent the limb from being placed far enough into the bore to allow the tarsus to be positioned at the isocentre of the magnet. The tarsus of a horse with this body type (or stature) is more easily positioned in a standing system. In contrast, for a narrow horse with long limbs, the height of the tarsus and width between the limbs may make it more diffi cult to image this region within a standing system. The degree of sway in the proximal aspect of the limbs in a standing, sedated horse is often substan- tially greater than in the distal aspect of the limbs. This degree of sway can produce signifi cant motion artefact and can make it frustrating to acquire images of the proximal tarsus. -
Analysis of the Talus and Calcaneus Bones from the Poole-Rose Ossuary
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 2005 Analysis of the talus and calcaneus bones from the Poole-Rose Ossuary: a Late Woodland burial site in Ontario, Canada Adrienne Elizabeth Penney Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Penney, Adrienne Elizabeth, "Analysis of the talus and calcaneus bones from the Poole-Rose Ossuary: a Late Woodland burial site in Ontario, Canada" (2005). LSU Master's Theses. 3114. https://digitalcommons.lsu.edu/gradschool_theses/3114 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. ANALYSIS OF THE TALUS AND CALCANEUS BONES FROM THE POOLE-ROSE OSSUARY: A LATE WOODLAND BURIAL SITE IN ONTARIO, CANADA A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Master of Arts in The Department of Geography and Anthropology by Adrienne Elizabeth Penney B.A. University of Evansville, 2003 August 2005 ACKNOWLEDGEMENTS I appreciate the cooperation of the Alderville First Nation, and especially Nora Bothwell, for allowing the study of the valuable Poole-Rose collection. I would like to thank Ms. Mary H. Manhein, my advisor, for all of her time, encouragement, and assistance. -

Management of Intra-Articular Fractures of the Calcaneus: Introducing a New Locking Plate
Shafa Ortho J. 2018 November; 5(4):e7991. doi: 10.5812/soj.7991. Published online 2018 October 9. Letter Management of Intra-Articular Fractures of the Calcaneus: Introducing a New Locking Plate Bijan Valiollahi 1, * and Mostafa Salariyeh 1 1Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran *Corresponding author: Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran. Email: [email protected] Received 2016 October 31; Revised 2018 September 22; Accepted 2018 September 27. Keywords: Calcaneus Fracture, New Plate, Sinus Tarsal Approach Dear Editor, displaced intra-articular fractures involving the posterior Fracture of the calcaneus is usually a challenging prob- facet and is ideally performed within three weeks of in- lem for orthopedic surgeons and patients. Calcaneal frac- jury. Beyond this time, separation of the fragments be- tures are the most common of tarsal bone fractures, and comes more challenging. To achieve an adequate reduc- most of them are displaced intra-articular (nearly 75%) frac- tion, surgery must be performed after soft tissue swelling tures, usually resulting from falling or motor vehicle acci- diminishes (2). dents (1). Full diminishing of soft tissue edema is demonstrated Most patients with calcaneal fractures are usually by a positive wrinkle test, indicating that surgical interven- young men in their prime working years, which results in tion may be performed safely. For the extensile lateral ap- a significant loss of economic productivity. Although sur- proach, a good skin with positive wrinkle test is needed. gical techniques and fixation implants have generally im- Concerns about high wound complication rates in the ex- proved functional outcomes, there is vast controversy as to tensile lateral approach have prompted some to improve the management of these highly complex injuries. -
The Occurrence of Tarsal Injuries in Male Mice of C57BL/6N Substrains in Multiple
bioRxiv preprint doi: https://doi.org/10.1101/2020.02.25.964254; this version posted February 25, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Long title: The occurrence of tarsal injuries in male mice of C57BL/6N substrains in multiple 2 international mouse facilities 3 4 Short title: Tarsal injury in C57BL/6N male mice 5 6 Eleanor Herbert2, Michelle Stewart1, Marie Hutchison1, Ann M. Flenniken4,5, Dawei Qu4,5, 7 Lauryl M. J. Nutter4,6, Colin McKerlie4,6, Liane Hobson1, Brenda Kick3, Bonnie Lyons3, Jean- 8 Paul Wiegand3, Rosalinda Doty3, Juan Antonio Aguilar-Pimentel7, Martin Hrabe de Angelis7,8,9, 9 Mary Dickinson10, John Seavitt10, Jacqueline K. White3, Cheryl L Scudamore1, Sara Wells1* 10 11 12 13 Affiliations 14 1 Mary Lyon Centre, MRC Harwell Institute, Harwell Campus, Oxfordshire, OX11 0RD, UK 15 2 Department of Pathobiology and Population Sciences, Royal Veterinary College, Hertfordshire, 16 UK AL9 7TA, UK 17 3 The Jackson Laboratory, 600 Main Street, Bar Harbor, Maine 04609, USA 18 4 The Centre for Phenogenomics, Toronto, ON, Canada, M5T 3H7 19 5 Lunenfeld-Tanenbaum Research Institute, Sinai Health, 600 University Avenue, Toronto, 20 ON, Canada, M5G 1X5 21 6 The Hospital for Sick Children, 555 University Avenue, Toronto, ON, Canada, M5G 1X8 22 7German Mouse Clinic, Institute of Experimental Genetics, Helmholtz Zentrum München, 23 Ingolstädter Landstraße 1, 85764 Neuherberg, Germany 24 8School of Life Science Weihenstephan, Technische Universität München, Alte Akademie 8, 25 85354 Freising, Germany 26 9German Center for Diabetes Research (DZD), Ingolstädter Landstr. -
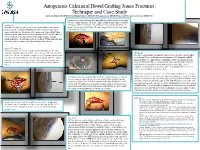
Autogenous Calcaneal Dowel Grafting Jones Fractures: Technique and Case Study Edward G
Autogenous Calcaneal Dowel Grafting Jones Fractures: Technique and Case Study Edward G. Blahous JR, DPM, FACFAS, Richard T. Bouché, DPM, FACFAS, Amol Saxena, DPM, FACFAS, FAAPSM, Chad Seidenstricker, DPM, PGY-3 A trephine is now used to obtain a bone graft plug, which will be used as an inlay graft to be placed into reamed hole. To assure a tight custom fit trephine diameter should be Introduction 1 mm greater than the reamer size. The authors’ prefer use of bone graft procured Many foot and ankle surgeons elect to treat the proximal fifth metatarsal base from the lateral calcaneal wall (Fig 6). The bone plug graft is then gently aligned and fractures near the metaphyseal-diaphyseal junction by surgical repair due to tamped into place (Fig 8). unpredictable outcomes with nonoperative management. Intramedullary fixation (IM) is the current “gold standard” and has high union rate [1]. However, there are several reports of complications with the IM technique. Notably, refracture, prominent hardware, and slow time to fracture healing [2-5]. This publication aims to describe a novel technique to treat the problematic Jones fracture. Figure 10. Intraoperative anteroposterior fluoroscopic Figure 11. Intraoperative lateral fluoroscopic view Figure 6. Incision placement with trephine in Figure 5. Visualization of recipient hole view of fracture site with graft and fixation in place. of fracture site with graft and fixation in place. Surgical Technique [6] place for safe exposure of lateral calcaneal through fracture site. The patient is placed in a lateral decubitus position with ipsilateral side facing wall. superiorly. A dorsolateral incision is made centered over the fifth metatarsal base Discussion fracture site. -

Understanding the First
CME / ORTHOTICS & BIOMECHANICS Goals and Objectives After reading this CME the practitioner will be able to: 1) Understand normal and abnormal function of the first ray with special emphasis on its integral role in medial longitudinal arch function and hypermobility. Understanding 2) Acquire knowledge of the various etiologic factors that result in first ray hypermobility. the First Ray 109 3) Appreciate its normal and abnormal motion along Here’s a review of its normal with its attendant bio and and abnormal function, identification, pathomechanics. and clinical significance. 4) Become familiar with vari- ous methods to subjectively and BY JOSEPH C D’AMICO, DPM objectively identify its presence. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Con- tinuing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $26.00 per topic) or 2) per year, for the special rate of $210 (you save $50). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. You can also take this and other exams on the Internet at www.podiatrym.com/cme. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. 144. Other than those entities currently accepting CPME-approved credit, Podiatry Management cannot guarantee that these CME credits will be acceptable by any state licensing agency, hospital, managed care organization or other entity. -

Radiography and Radiographic Interpretation of the Tarsus (VET-473) Western Veterinary Conference 2004 Timothy R
Radiography and Radiographic Interpretation of the Tarsus (VET-473) Western Veterinary Conference 2004 Timothy R. O'Brien, DVM, PhD, DACVR University of California, Davis Davis, CA, USA 18276161 I. Introduction Tarsal diseases are a common cause of hind limb lameness in the horse. The clinical signs of tarsal disease often resemble those of stifle disease particularly the response to flexion tests. As a result both the stifle and tarsus are commonly radiographed to identify pathologic change in the horse with a hind limb lameness and during purchase evaluations. It seems prudent for purchase evaluations to radiograph these anatomical areas in both limbs. Radiographic interpretation of the tarsus is considered difficult by most equine practitioners. There seems to be three major causes of this difficulty. These causes relate to the numerous bones comprising the tarsus, variety of shapes of the tarsal bones, and veterinarians tend to be less familiar with the radiographic anatomy and pathology of the tarsus than most other anatomical regions, particularly regions of the forelimb. I am going to make some general statements in an attempt to simplify the radiographic interpretation of the tarsus. These general statements are: Most radiographic findings are located at the dorsum of the tarsus. Pathologic abnormalities of the tarsus tend to be in specific anatomical areas. Soft tissue swelling (STS) is a key for assisting to localize the abnormality. There are only a few radiographic diagnoses for the tarsus. The diagnoses of abnormalities of the tarsus identified with radiology can be classified in the following way: 1. Soft tissue swelling without bony change 2. -

Foot and Ankle Injuries
Foot and Ankle Injuries Today’s lecture can be viewed at Learning in Athletics the following URL address: We most likely will not get “All of life should be a through all these slides today, learning experience, not Thomas W. Kaminski, PhD, ATC, http://sites.udel.edu/chshowever the presentation- atep/lectures/is just for the trivial FNATA, FACSM, RFSA thorough and complete and will reasons but because by Professor make for an excellent study continuing the learning Director of Athletic Training Education guide for the BOC process, we are challenging our brain University of Delaware examination! Good Luck! and therefore building brain circuitry” Arnold Scheibel Athletic Training & Sports Laboratory Manual UD is located here! A First State to accompany Fact! Health Care: The Journal for the Rehabilitation Techniques in Sports Medicine Delaware is 96 miles Practicing Clinician and Athletic Training long and varies from th 9 to 35 miles in 6 Edition width. http://www.healio.com /journals/atshc https://www.healio.com/books/athletic- training/%7b927168ac-1da2-422c-b98e- ae9013d4e15b%7d/rehabilitation-techniques-for- sports-medicine-and-athletic-training-sixth-edition Perhaps ATC’s Need to Incorporate Lower Extremity ~ Foot this Into Their Assessment Scheme? Anatomical Review Cyriax- “Diagnosis is only a matter of applying one’s anatomy” 1 Clinical PEARL: Lower Extremity ~ Foot Navicular Palpation Lower Extremity ~ Foot • Palpated 2-3 cm anteroinferior to the medial malleolus • More prominent with foot adducted Radiographically Viewed The Ankle Mortise Articulations Ankle Joint (Medial View) 1. Fibula 2. Tibia 3. Ankle jointChallenge 4. Promontoryyourself of tibia to 5. Trochlear surface of talus 6.