Transcript-Full Committee Meeting-June 17, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Army Bases Ready for Ban on Under-21 Tobacco Sales
VIRUS OUTBREAK NFL VIDEO GAMES US unemployment surges Houston to kick 5 great indie titles to 14.7%, a level last seen off season at to play on Nintendo during the Great Depression Kansas City Switch right now Page 7 Page 23 Page 14 Online: Get the latest news on the virus outbreak » stripes.com/coronavirus Volume 79, No. 15A ©SS 2020 CONTINGENCY EDITION SATURDAY, MAY 9, 2020 stripes.com Free to Deployed Areas MICHAEL ABRAMS/Stars and Stripes The Pentagon will raise the age for the sale of tobacco products on military installations from 18 to 21, beginning Aug. 1. Army bases ready for ban on under-21 tobacco sales Stars and Stripes Service members under 21 will not be allowed to buy tobacco products on base beginning in August, when a new Pentagon- wide policy goes into effect. The rule affects the sale of ciga- rettes, smokeless tobacco, hookah tobacco, cigars, pipe tobacco and vaping supplies, such as e-ciga- rettes and e-liquids, the Army said in a statement released this week. It takes effect Aug. 1 at all in- stallations and facilities in the US pulling anti-missile systems U.S., its territories and posses- sions and on Navy ships in U.S. Patriot shuffle from Saudi Arabia amid dispute ports, the statement said. Retail- ers are required to post signs BY LOLITA C. BALDOR Middle East region are also heading home alerting customers to the change Associated Press A U.S. Patriot missile system is seen at to the U.S., in a planned redeployment for by July 1, it stated. -

Can Murphy Break the Curse?
This issue brought to you by New Jersey Governor: Can Murphy Break The Curse? By Jacob Rubashkin FEBRUARY 5, 2021 VOLUME 5, NO. 3 Not long ago, New Jersey Gov. Chris Christie was riding the wave of a re-election win into a top-tier presidential bid. A few years later, politics on the ground have shifted, and Garden State Republicans are grasping 2022 Senate Ratings for power, just hoping to stay competitive in this year’s gubernatorial contest. BATTLEGROUND New Jersey is one of two states (Virginia is the other) that will elect a Democratic-Held (4) Republican-Held (4) governor this year, posing as the appetizer for 2022, when 36 states will Cortez Masto (D-Nev.) NC Open (Burr, R) host a gubernatorial election. Politicos will be looking at both 2021 races Hassan (D-N.H.) PA Open (Toomey, R) for any clues about the national political environment for the midterms, Kelly (D-Ariz.) Johnson (R-Wisc.) including whether the party in power will suffer from the health or Warnock (D-Ga.) Rubio (R-Fl.) economic effects of Covid-19. Solid Democratic (10) Solid Republican (16) Lay of the Land Bennet (D-Colo.) OH Open (Portman, R) New Jersey is a Democratic state. With the exception of 2004, when Blumenthal (D-Conn.) Blunt (R-Mo.) John Kerry won the state by a vanishingly narrow 7 percent, every Duckworth (D-Ill.) Boozman (R-Ark.) Democratic presidential candidate since 2000 has won the state by between Padilla (D-Calif.) Crapo (R-Idaho) 14 points (Hillary Clinton in 2016) and 17 points (President Barack Obama Leahy (D-Vt.) Grassley (R-Iowa) in 2012), regardless of national environment. -

COVID-19 Updates Memo
August 4, 2020 TO: ALL COUNTY COMMISSIONERS, COUNTY EXECUTIVES, COUNTY COUNCIL MEMBERS, COUNTY ADMINISTRATORS AND COUNTY CLERKS FROM: CHERYL SUBLER, EXECUTIVE DIRECTOR RACHEL MASSOUD, POLICY ANALYST ADAM SCHWIEBERT, POLICY ANALYST RE: AUGUST 4, 2020 COVID-19 UPDATES Key Resources 1. CCAO CARES Act Funds Resources Webpage 2. OBM CARES Act Funds Guidance 7.16.2020 3. CCAO Guidance on Using CARES Act Funds 4. Treasury Guidance CARES Act Funds 6.30.2020 5. Treasury CARES Act Funds FAQs 7.8.2020 6. CAB: Employees Returning to Work FAQs 7. CAB: Layoffs and Furloughs Under Civil Service Law 7.15.2020 CCAO COVID-19 Resources Page Gov. DeWine’s Press Conference During today’s press conference, Gov. DeWine announced that the Ohio Department of Health (ODH) will issue a new order requiring that children grades K-12 wear a mask while at school. The administration is working to distribute two million masks to schools and will use regional education service centers to distribute. The order will soon be available here. Lt. Gov. Husted clarified that the administration is still working on its plan for high school contact sports for the fall. An ODH order regarding contact sports from July 4th was extended this week. The administration stated that July 4th order is not the plan for high school contact sports and should not be viewed as such. The administration continues to work with the Ohio High School Athletic Association on this matter. Additionally, Lt. Gov. Husted noted the administration is working with professional sport organizations in Ohio on plans for their seasons. -

The Baldwin Wallace University Ohio Poll in Partnership with Oakland University and Ohio Northern University April 26, 2020
The Baldwin Wallace University Ohio Poll In partnership with Oakland University and Ohio Northern University April 26, 2020 Contents Vote choice in 2020 . .3 Approval: President Trump . 13 Approval: Presidential response to COVID-19 . 15 Approval: Governor DeWine . 17 Economy . 25 Media consumption . 28 Civil liberties and disobedience . 33 COVID-19 personal impact . 37 Just for fun . 48 1 The Baldwin Wallace University Ohio Poll was conducted between 4/20/20 and 4/25/20 in partnership with Oakland University (Michigan) and Ohio Northern University. The survey was conducted online among self-identified registered voters in Ohio (n = 797) using Qualtrics, an online sample aggregator. Sampled individuals were emailed by Qualtrics and responded using a personalized link to the survey. The survey included quotas for age, education, and gender for each state. The quota for age was based on the 2016 Voting and Registration Supplement to the Current Population Survey. The quotas for education and gender were based on data from the 2017 American Community Survey. The survey also included quotas for central metro areas and fringe metro areas at the county level based on data from the U.S. Census, as well as the 2013 National Center for Health Statistics’ (NCHS) Urban-Rural Classification Scheme for Counties. The survey results are weighted by gender, education, race/ethnicity, and annual household income to be representative of each state’s population. In this survey, the design factor was 1.08. The overall margin of error was ±3.7%. The sample size and margin of error are applicable only to overall results, indicated by highlighted columns in the following tables. -

Public Address This Academic Year Marks My 20Th Year at Surged in Ohio
Public Address This academic year marks my 20th year at surged in Ohio. We moved all our events Ohio State. Just prior to the start of my first online, including a fully virtual memorial academic term in 2001, I went on a for Annie Glenn. Students, faculty and University-organized tour of Ohio on staff joined millions of other Americans Tuesday, September 11. The tour was cut in participating in the 2020 election in short by the news of planes crashing into the record numbers. And we all tightened our Twin Towers in New York City and the belts in response to a dramatic decrease in Pentagon in Washington, D.C., killing just our projected revenues for this academic under 3000 Americans. Seven years later, the year. This issue of Public Address crash of the housing market led to the largest features many of the ways we as a contraction of the economy since the Great College have responded to the pandemic. Depression. And then four years ago, less than What’s missing in this issue is the A Letter a month after a tumultuous 2016 presidential degree to which protests around racism from the election, Ohio State campus police shot and and inequity last summer and the killed a Somali refugee who had rammed his storming of the U.S. Capital have Dean vehicle into a crowd of students. Two weeks engulfed the college. Glenn College later Senator John Glenn passed away. faculty, students and staff are passionate Since the first evidence of COVID-19 about issues of fairness and justice and infections in the U.S. -

Pro-Life Hypocrisy on COVID-19 “ ” Summary
Pro-Life Hypocrisy on COVID-19 “ ” Summary Amidst the ongoing COVID-19 pandemic, anti-choice political leaders have made it crystal clear that they don’t value people’s lives. As NARAL has previously documented, self-styled pro-life politicians and pundits have largely ignored the threat of the virus and failed to “ ” work towards solutions that could protect public health – instead, choosing to capitalize on the crisis to attack abortion access. Now, against experts’ recommendations, these so-called pro-life politicians and pundits “ ” have criticized and defied stay-at-home orders in states across the country. Their latest messaging on the COVID-19 crisis falls into six main themes: ● Prioritizing the Economy Over Public Safety ● Promoting/Attending Anti-Quarantine Protests ● Attacking Social Distancing Orders ● Attacking Health Authorities ● Discouraging / Not Wearing PPE ● Dismissing COVID Death Toll If these anti-choice extremists truly valued people’s lives as they claim, they wouldn’t be telling them to put themselves in unsafe situations during a pandemic. There’s nothing pro-life about deliberately putting people’s health and safety at risk. “ ” Contents Prioritizing the Economy Over Public Safety Gov. Greg Abbott (TX) Glenn Beck Former Gov. Chris Christie State Rep. Scott Clem (WY) Sen. Ted Cruz (TX) Gov. Doug Ducey (AZ) Gov. Ron DeSantis (FL) Lyndsey Fifield Rep. Trey Hollingsworth (IN) House Freedom Caucus Sen. Ron Johnson (WI) Gov. Brian Kemp (GA) Sen. John Kennedy (LA) Former Rep. Jason Lewis, Candidate for US Senate Sen. Kelly Loeffler (GA) State Rep. Danny McCormick (LA) House Candidate Tom Norton (MI) Lt. Gov. Dan Patrick (TX) Sen. -

Ailing Malls Face Another Threat with Covid 19
LOOK BACK | THE BLACKOUT FOCUS | LEGAL AFFAIRS: Law schools adapt instruction for the COVID-19 classroom. PAGE 10 NEO had a big role in a dark day for many. PAGE 23 CRAINSCLEVELAND.COM I AUGUST 10, 2020 SMALL BUSINESS RETAIL Flexibility key for employers AILING MALLS and working FACE ANOTHER parents Uncertain school year THREAT WITH presents many hurdles BY RACHEL ABBEY MCCAFFERTY COVID19 In March, everything changed. On the y, employers had to nd ways to accommodate employees who were suddenly balancing child care and work in a new way, as schools went remote and child care centers closed when the COVID-19 pandemic came to Ohio. is fall is sure to hold similar Child care, with conditions: Ohio child care centers can return to pre-pandemic student-teacher ratios, but they must follow a host of safety and hygiene measures. Page 21 challenges. e only di erence? Em- ployers have time to plan ahead for the inevitable. And how they respond SouthPark Mall in Strongsville is seeing a slow return of foot tra c, despite now could have implications for the social distancing requirements. | DAVID KORDALSKI/CRAIN’S CLEVELAND BUSINESS future. In the spring, there was a tangible end in sight for those balancing work Foot tra c, a key indicator of mall health, has fallen 40% from January numbers and their children’s virtual learning. “It felt like there was a term to it,” BY STAN BULLARD Ohio stay-at-home order ended. said John Bernatovicz, founder of Foot tra c at the malls as of July 25 sta ng and consulting rm Willory Northeast Ohio’s already ailing en- is running 40% below what it was in in Bath. -

Key Resources
April 1, 2020 TO: ALL COUNTY COMMISSIONERS, COUNTY EXECUTIVES, COUNTY COUNCIL MEMBERS, COUNTY ADMINISTRATORS AND COUNTY CLERKS FROM: CHERYL SUBLER, EXECUTIVE DIRECTOR RACHEL MASSOUD, POLICY ANALYST ADAM SCHWIEBERT, POLICY ANALYST RE: APRIL 1, 2020 COVID-19 UPDATES Key Resources 1. CAB on Virtual Meetings during COVID-19 2. Emergency Declarations FAQ 3. CAB on COVID-19 Employment Related FAQs 4. Other HR Related CABs 5. County Purchasing Authority during COVID-19 CCAO COVID-19 Resources Page Gov. DeWine’s COVID-19 Press Conference In today’s press conference, Gov. DeWine and Dr. Amy Acton announced that Ohio now has 2,547 confirmed cases. There have been 65 COVID-19 related deaths. Gov. DeWine signed an executive order to help small businesses. The order requests that landlords suspend rent payments for small businesses facing financial hardship due to the COVID-19 pandemic. Landlords are requested to also implement a moratorium of evictions of small business, commercial tenants for no less than 90 days. Lenders to commercial real estate borrowers with a commercial mortgage loan are asked to provide an opportunity for forbearance for at least 90 days. The administration is asking for help from the manufacturing community. They encourage manufacturers to visit https://repurposingproject.com/ to see what the state needs help providing and for more information. If you want to help Ohio’s response to this pandemic, you can contact the state at [email protected]. A video of the governor’s April 1st press conference can be found here. The administration plans to continue daily press briefings at 2 pm. -

NIH FOIA Case No.: 53853; Daily Caller V
DEPARTMENT OF HEALTH&, HUMAN SERVICES Public Health Service National Institutes of Health Freedom of Information Office Building 31, Room 5B-35 31 Center Drive, MSC 2107 Bethesda, Maryland 20892-2107 phone: (301) 496-5633 fax: (301) 402-4541 Via Email: [email protected] November 23, 2020 Chuck Ross The Daily Caller 22110 W. 52nd Street Shawnee, KS 66226 Re: NIH FOIA Case No.: 53853; Daily Caller v. HHS, Case No. 20-cv-1149 (DLF) (D.D.C.) Dear Mr. Ross: This is a partial response to the Freedom of Information Act (FOIA) request that is the subject of the complaint filed in Daily Caller v. HHS, 20-cv-1149, now pending in the U.S. District Court for the District of Columbia. Your FOIA request, dated April 1, 2020, was received by the National Institutes of Allergy and Infectious Diseases (NIAID) on the same day. You requested communications of Dr. Anthony Fauci and Dr. H. Clifford Lane that either 1) include a World Health Organization official and concern the novel coronavirus, or 2) discuss the World Health Organization or certain of its officials, as well as China and the novel coronavirus. You requested these communications from January 1, 2020 to April 1, 2020. In accordance with the Court’s order dated September 22, 2020, we have processed 301 pages of responsive records this month, in addition to 300 pages that were processed last month. We are producing them to you, with certain information withheld pursuant to FOIA Exemptions 4 and 6 of the FOIA, 5 U.S.C. 552(b)(4), 5 U.S.C. -
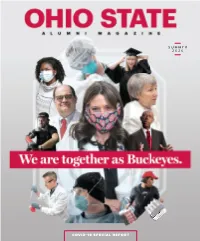
COVID 19 SPECIAL REPORT There Is No Routine Cancer
SUMMER 2020 COVID19 SPECIAL REPORT There is no routine cancer. Just like no two people are exactly the same, neither are their cancers. Each patient’s cancer is fueled by different, unique elements that help cancer cells develop, survive, invade and grow. That’s why researchers and oncologists at The James at Ohio State study the unique genetic makeup of each patient’s cancer. As they discover what drives a patient’s cancer, they develop and deliver the most advanced targeted treatments, leading to better outcomes, faster responses, fewer side effects and more hope. To learn more, visit cancer.osu.edu. James No Routine general_OhioMag_8x10.75.indd 1 5/14/20 2:31 PM How Firm Thy Friendship | SUMMER 2020 Being far from his own home, he can relate to students’ experiences living away from their loved ones, and he puts this knowledge to use every day to support students in our residence halls. In addition to being a staff member, Cornelius is a new alum: He earned his bachelor’s degree in education in May. VOLUME 111, ISSUE 5 Classrooms are on his horizon, but not one to PUBLISHER Molly Ranz Calhoun ’86 teach in — yet. He’ll begin working toward his master’s degree in the fall. If he could gift VICE PRESIDENT FOR MARKETING current and future students anything at all, Adrienne Nazon he says he would choose determination EDITOR and motivation. Mary Alice Casey “Fight for what is important to you,” he ASSOCIATE EDITOR Kristen Schmidt advises. “Never give up.” That is such good guidance for all of us. -

Central OEA/NEA Local Leadership Training Summer Day Trips To
Summer 2021 The American Rescue Plan Act Provides $122 Billion Relief Funding Is Fair School for K-12 Funding Inching Closer Central OEA/NEA Via the Budget? Local Leadership Training Summer Internet Safety and the Day Trips Ohio Educator Code of Conduct to Enjoy Rest if You Must, But Keep Advocating for Change Adrienne M. Bowden (Pickerington EA) Central President and NEA Director This past school year had been a stressful one, to say the After recharging your batteries, we must get right back into least. Some schools started the year teaching remotely, educating and advocate for the students we serve. Issues many others were open from day one for full-time in-person and considerations from the beginning of last school year instruction. As educators and support professionals, we have not gone away. We must work together to dismantle entered the school year in unchartered waters. Many of us unjust racial and social systems and find a way to fully fund went without adequate training in distance learning and CDC public education in our communities. Now is the time to hold protocols, we learned how to master new tools and tech- our elected officials accountable and get the needed nologies, how to keep students engaged in distracting home services and systems in place for the upcoming school year. environments, and what to do about inequities in social and racial justice that have been made worse by the pandemic. A great resource for information on how you can be a part of this effort is NEA’s Advocating for Change website The stakes for this year felt unbearably high. -

Premier Pulse News for Premier Health Physicians VOLUME 7 | ISSUE 5 | JULY 2020
Premier Pulse News for Premier Health Physicians VOLUME 7 | ISSUE 5 | JULY 2020 Future of Health Care in the Era of COVID-19 By Matthew S. Reeves, DO, MBA, chief of integrated care, Premier Health Acknowledging that vast swaths of providers and patients have shortage of severe magnitude, and we are nowhere near engaged in new means of providing health telehealth is a woefully underutilized tool in being out of the thick care that I think they’ll appreciate and want our toolbox. of COVID-19, there to continue. Until this change was forced With great disruption comes the opportunity are some lessons upon them, patients and providers could not for great innovation and leadership. This learned and trends fully understand or accept that change. will be a lesson learned from numerous developing. For example, telehealth, especially in the perspectives – telehealth being just one Over the long-term, outpatient setting, is changed forever. illustration. When we look back on this lower hospital admissions will be the new Patients will demand this ease of access. time, it will be identified as the tipping norm. Hospitals will move toward becoming Providers are going to feel a relief from point transforming our “sick-care” system centers of excellence and/or large intensive running the rat race to keep up by unloading to a “well-care” system. Out of necessity, care units caring for a smaller volume of some of the care to these more efficient new business models will develop that have higher acuity patients. models. Granted, limitations and possible greater vertical integration and collaboration As with any stress/crisis, the best and the abuse of telehealth is a reality.