2016 AHA IT Survey
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Update from the CEO by Charles Jaffe, MD, Phd, HL7 CEO HL7’S 22Nd Annual Plenary Meeting
AUGUST 2008 In This Issue... Update from the CEO By Charles Jaffe, MD, PhD, HL7 CEO HL7’s 22nd Annual Plenary Meeting..... 2 Work Group Co-Chair Elections: As the languid days of August almost impercep- Development Organizations What to Expect in Vancouver................ 3 tibly transform into the cool autumn nights of (SDOs). Most importantly, September, some significant milestones emerged Update from Headquarters.............. 4-5 it is a living document. The from the HL7 landscape. Roadmap development team ExL Pharma’s 4th Annual EHR and will continue to be com- Charles Jaffe, MD, PhD eClinical Technologies Conference....... 6 The membership of HL7 has its very first posed of a broad constitu- News from the PMO.............................. 6 Roadmap. A strategic plan for technical and busi- ency with distinct requirements, and with plans to ness development is embodied in this document. It publish Roadmap updates annually. Version 3 Normative Edition 2008 Now Available...................................... 7 is more than just a promise to our stakeholders; the Roadmap provides the end-user community, gov- As the Roadmap matures, it will reflect the changing Multiple Modes of Delivering ernment agencies, software developers and other Education............................................. 8 business needs of our organization. More opportuni- standards development organizations clear guide- ties require more creative resource development and Advisory Council News....................... 9 lines for our products and services. In addition, the new means of expanding our funding model. Co-Chair Election Results.................... 9 Roadmap offers something beyond a commitment to develop a new standard or a new release of a Part of our new funding model emerged with the HL7 Certification Exam balloted one. -
HL7 Mobile Health Work Group
SEPTEMBER 2013 HL7 Mobile Health Work Group 101 By Gora Datta, Co-Chair, HL7 Mobile Health Work Group; Co-Lead, HL7 In- teroperability EHR Work Group; HL7 Ambassador; Group Chairman & CEO, CAL2CAL Corporation The HL7 Mobile Health (MH) Work Group is now • Identify and one year old! Over the past year, the work group promote mobile (WG) has rapidly matured from loosely held health concepts interested individuals to a cohesive group of ex- for interoper- perts that meets regularly. We welcome one and ability as Gora Datta all to join our Mobile Friday weekly calls every adopted and Friday at 11am ET. adapted for use in the mobile environment. • Coordinate and cooperate with other The group’s mission “The HL7 Mobile Health groups interested in using mobile health to Work Group creates and promotes health infor- promote health, wellness, public health, mation technology standards and frameworks for clinical, social media, and other settings. mobile health” captures the essence of its charter, • Provide a forum where HL7 members and as outlined: stakeholders collaborate in standardizing • Identify (and develop, as applicable) data to enable the secure exchange, storage, standards and functional requirements that analysis, and transmission of data and are specific to the mobile health environment. information for mobile applications and/ or mobile devices. One of the challenges the group has is that it is one of the few HL7 groups (like the EHR WG) that is not domain specific; and is more horizontal in nature. Therefore, its charter cuts across other vertical/domain oriented (work) groups. Given the tremendous interest and participation not only in the US but also globally, the HL7 Mobile Health WG is rapidly stepping up to identify and fill the gaps in the mobile health standards space. -

Seven Members Honored HL7 Honored Seven Members with the 14Th Annual W
JANUARY 2011 Upcoming WORKING GROUP MEETINGS 2010 Ed Hammond Volunteer of the Year Awards Seven members honored HL7 honored seven members with the 14th annual W. Edward Hammond, PhD Volunteer of the Year Award. Established in 1997, the award is named after Dr. Ed Hammond, one of HL7’s most active volunteers, founding member and past Board chair. The award recognizes individuals who January 9 – 14, 2011 May 15 – 20, 2011 have made significant contributions to HL7’s success. The 2010 recipients include: • Hugh Glover and Julie James, HL7 UK January Working Group • Stan Huff, MD, chief medical informatics officer, Intermountain Healthcare Working Group Meeting • Charlie Mead, MD, MSc, CTO, 3rd Millennium, Inc. Meeting • Mark Shafarman, principal, Shafarman Consulting Hilton in the Walt Disney World Resort • D. Mead Walker, Health Data and Interoperability, Inc. Cliftons Meeting and Training Center Lake Buena Vista, FL • Pat Van Dyke, director of information, security, privacy and EDI representing Delta Dental and the Amora Hotel Plans Association Sydney, Australia About the Volunteers: Hugh Glover and Julie James have been involved with HL7 since 2001. They received the award jointly as they are partners both personally and profession- ally. They have both actively contributed to HL7 for many years and have held leadership positions in the Pharmacy Work Group such as a co-chair or facili- tator. Their backgrounds—James as a pharmacist and Glover’s expertise in data modeling—complement each other and have brought valuable insight to HL7. Both have been involved with Version 3 development since its inception. James September 11 – 16, 2011 January 15 – 20, 2012 is also active in the Patient Safety Work Group. -

Open Platform Architecture Based Upon SMART Apps Platform and the HL7 FHIR® (DSTU) Demonstrated at HIMSS14
MAY 2014 Open Platform Architecture Based Upon SMART Apps Platform and the HL7 FHIR® (DSTU) Demonstrated at HIMSS14 By David Kreda, Translation Advisor, and Joshua Mandel MD, Lead Architect, SMART Platforms Project Harvard Medical School/Children’s Hospital Boston www.smartplatforms.org During the HIMSS14 Annual Conference (Feb- ferent internal architectures ruary 23-27, 2014 in Orlando, Florida), several and technologies, they healthcare IT exhibitors presented an eye-open- were nonetheless able to ing example of the potential of HL7’s newest supply the data via FHIR standard, FHIR® (Fast Healthcare Interoperabil- API calls made by the suite David Kreda ity Resources). The list of exhibitors included of SMART Apps that were Cerner, Intermountain Healthcare, Hewlett Pack- installed on their systems. ard, and Harris Corporation. They presented the Harris Corporation then SMART on FHIR Open Platform Architecture, demonstrated its services which combines FHIR and the open source, web- oriented architecture (SOA) standards based technology stack created by the service, which accepted SMART Platforms Project, a research effort based same FHIR API queries at Harvard Medical School and Children’s Hos- from the SMART apps, fed- pital Boston that enables real-time integration of erated queries to the same substitutable medical apps, or SMART apps, on EHR systems holding the EHR systems. patient data, and synthe- Josh Mandel, MD sized a cross system, longi- Three sophisticated EHR systems, including tudinal patient record, which was returned to the Cerner Millennium, HELP2 from Intermountain requesting SMART app. Healthcare, and VistA from the Veterans Health Administration, were each independently FHIR- Hewlett Packard, which engineered the SMART enabled in less than six weeks. -

A Survey of U.S. Healthcare IT Industry Landscape
July 28, 2016 Industry Research Department, Mizuho Bank Mizuho Industry Focus Vol. 183 A Survey of U.S. Healthcare IT Industry Landscape Global Corporate Advisory Americas Tim Wang, CFA, 2016 [email protected] 〈Summary〉 ○ U.S. Healthcare IT industry is booming. Over the recent years, many companies have had robust growth and the sector has attracted huge inflow of private and public investments. There are many types of HCIT companies, operating with different business models and participating in various segments of HCIT. In this report, we try to first identify the drivers behind HCIT growth and then delineate the dynamics in each HCIT segment. ○ Key drivers of HCIT are also the underlying drivers of the U.S. healthcare system, namely Obamacare, the transition to value-based reimbursement model, rising consumerism, industry consolidation, etc. Within HCIT, major drivers include the HITECH Act, advancement of technology, and the convergence of healthcare, IT, and consumer industries. ○ The booming HCIT market is in transition. Incentives for EHR created by the HITECH Act have largely run their course. In the future, the marketplace will be driven less by government subsidies and more by private spending. To earn revenues from private payers, HCIT companies increasingly need to demonstrate the clinical and financial value of their offerings. To achieve this, HCIT companies need to collaborate closely with their customers. ○ For the various HCIT segments, we see three especially promising areas – integration of remote patient monitoring either through wearables or other devices with data analytics and intervention capabilities; big data analytics by Artificial Intelligence; and telemedicine. We expect stable growth for RCM, PM, payer solution segments. -

Healthcare Services: Healthcare IT Services Insights
January 2013 Healthcare Services: Healthcare IT Services Insights 2013 Outlook — Focus on Data Analytics Background too soon for the US healthcare system. pressure on federal and state budgets, In 2009 healthcare providers began to make Healthcare is a data-intensive endeavor and employers’ income statements and household their first healthcare IT investments in the wise application of technology to analyze income making the cost trend unsupportable; anticipation of receiving the incentives and data is among the best tools available to and iii) with the enactment of the Affordable avoiding the penalties for achieving improve efficiencies and manage risk in Care Act (the “ACA”), 20 million people Meaningful Use as prescribed by the order to ensure delivery of quality care to an poised to enter the market with coverage at American Recovery and Reinvestment Act of increased population of insured in the face the lowest level of reimbursement. A 2009 (“ARRA”). According to the CMS, as of budget constraints and payment reforms. revolution is underway in which payers of November 2012, about $9.3 billion in — governments, employers and consumers While the macro factors driving trends in the electronic health record (EHR) incentive — are overthrowing the old regime of sector are well known, they are so profound payments had been made to 173,168 fee-for-service and forcing risk-bearing that they bear repeating: i) a multi-decade professionals and 3,393 hospitals. The reimbursement models such as bundled trend of healthcare expenditures rising faster ARRA may or may not have spurred payments, value based purchasing, than GDP, as a result of an aging population recovery, but it certainly stimulated accountable care and readmission penalties and increases in cost of care; ii) extreme reinvestment in healthcare IT, perhaps none onto providers. -
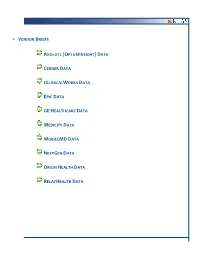
Vendor Briefs Axolotl (Optuminsight) Data Cerner Data Eclinicalworks Data Epic Data Gehealthcare Data Medicity Data Mobilemd
. VENDOR BRIEFS AXOLOTL (OPTUMINSIGHT) DATA CERNER DATA ECLINICALWORKS DATA EPIC DATA GE HEALTHCARE DATA MEDICITY DATA MOBILEMD DATA NEXTGEN DATA ORION HEALTH DATA RELAYHEALTH DATA Vendor Briefs 22 I HIE Study 2011 This material is copyrighted. Any organization gaining unauthorized access to this report will be liable to compensate KLAS for the retail price. Vendor Briefs . AXOLOTL (OPTUMINSIGHT) ELYSIUM EXCHANGE Number of With 14 live public HIEs (more than any other vendor) and 8 live private HIEs validated, Live HIEs Axolotl is one of the few vendors that can boast substantial penetration in both the Claimed by public and private markets. They have been working in the HIE market since 1995, and Vendor when it comes to mindshare in the current HIE market, Axolotl is on the short list of vendors that providers consistently mention. In addition, Axolotl is one of the few HIE vendors actively pursuing opportunities in the public HIE market. NA Axolotl customers at public HIEs tend to be more satisfied than customers at private Number of HIEs, as evidenced by the disparity in KLAS performance scores between the two Live Public groups—public HIEs give Axolotl an average score of 83.8, while private HIEs give them HIEs Validated an average score of 76.4. Providers at public HIEs generally feel like they get what they expect from Axolotl and 14 appreciate how engaged they are as a vendor. One CIO at a public HIE commented, “I worked with Axolotl to get everything up and running. I worked with their sales manager. He spent a lot of time going over what they could and, more importantly, what they Public HIEs couldn’t do by way of an HIE. -

Healthcare & Life Sciences Update
Healthcare & Life Sciences Industry Update December 2012 Member FINRA/SIPC www.harriswilliams.com What We’ve Been Reading December 2012 • An article in the New York Times by Robert Pear gives some very useful information around the tax increases that will be taking effect in January as part of the ACA. With the general media mostly focused on the fiscal cliff and the impending rises in capital gains and dividend taxes, many affluent Americans have overlooked the additional taxes they will be hit with in order to fund health reform. The article goes into some detail on the payroll, investment and income taxes that are expected to generate more than $300 billion in tax revenues over the next 10 years with 85% coming from the top 1% of taxpayers. • In order to save costs, California is currently experimenting with a program by which a large group of disabled Medicaid enrollees have been moved out of traditional fee-for- service coverage into managed care plans outsourced to commercial insurers. According to an article by Mary Carey and Sarah Varney at Medcity News, this program is being closely watched by both industry and the federal government ahead of the shift of 2 million Medicare/Medcaid dual eligibles into managed care as required by the ACA. California is expecting to save $663 million as part of the program but there is significant concern that the standard of care for these patients will suffer. • The Supreme Court is set to consider the legality of settlements between branded and generic pharmaceutical companies sometimes called “Pay for Delay” settlements, according to an article in the Wall Street Journal. -
HL7 Pilot Program Provides Key Intellectual Property Free of Charge
MAY 2012 HL7 Pilot Program Provides Key Intellectual Property Free of Charge HL7 recently announced a pilot program to provide some of its key intellectual property free of charge. “HL7 is keeping its promise to lower the barriers to adoption of electronic health records by making portions of our valuable intellectual property freely available to our stakeholders,” said Charles Jaffe, MD, PhD, CEO of HL7. “We believe that care givers, academic centers and vendors will greatly benefit from this significant enhancement for access to valuable HL7 material.” In the pilot project, HL7 will enable no-cost licensing of its domain analysis models (DAMs) and functional profiles. This offer, a first for HL7, was announced at the 2012 HIMSS Annual Conference and Exhibition, one of the largest health information technology conferences in the United States. The DAM is a set of requirements that explore and analyze the business of a particular clinical “domain.” Domain analysis is the first step in creating HL7 standards for a specific care or research environment. The domain analysis process produces documentation describing the stakeholders, activities, interactions, and information for a particular domain and serves as the source of require- ments used in the design of HL7 standards. Stand-alone DAMs will be made available at no cost during the one-year pilot, including: • HL7 Version 3 DAM: Cardiology; Acute Coronary Syndrome • HL7 Version 3 DAM: Clinical Trials Registration and Results • HL7 Version 3 DAM: Analysis Model: Vital Records Functional profiles for the HL7 Electronic Health Record System Functional Model (EHR-S FM) will also be available as part of the pilot program. -
HL7 International Is Coming to Canada in 2012 (Again!) Michael Van Campen
SEPTEMBER 2011 HL7 International is Coming to Canada in 2012 (Again!) Michael Van Campen By Michael van Campen, Chair, HL7 Canada; Affiliate Director, HL7 International Board of Directors In keeping with the tradition of hosting annual, non-US working group meetings (WGMs), HL7 Canada and HL7 International will be hosting the May 2012 Working Group Meeting in Vancouver, BC, May 13-18. This follows on the successful meeting in Vancouver in Sep- tember 2008 where over 500 attendees participated in the working group meetings. The May 2012 WGM will be an excellent opportunity to understand and share Canadian HL7 experiences with the HL7 international community, specifically around HL7 Version 3 and the Clinical Document Architecture (CDA®) in provincial and national implementations — the EHR is active and growing in Canada! Vancouver is a popular destination, with many international and domestic flights from Asia, Europe and the Americas. For those who attended in 2008, Vancouver has now installed a light rail connection from the Vancouver airport to downtown Vancouver. Also, there are many remnants of the 2010 Winter Olympics for those interested in the facilities. Lastly, May is spring time in Vancouver, with several outdoor activities for those interested in getting close to nature. continued on next page . ® Health Level Seven and HL7 are registered trademarks of Health Level Seven International, registered in the US Trademark Office In This Issue... HL7 Is Coming To Canada, continued HL7 Coming to Canada, Again!............ 1-2 HL7 and IHTSDO Expand Collaborative Efforts................................ 3 Please mark your calendars for this important 25th Annual Plenary Meeting Agenda... -

April 2009 Newsletter
APRIL 2009 Health Level Seven Hosts Pioneering Cross-Continent Dialogue on Standards and Interoperability in Africa In This Issue... at January Working Group Meeting HL7 Hosts Dialogue on Standards and Interoperability in Africa.......... 1, 3 HL7 hosted a high- Update from the CEO........................... 2 level delegation of five Ugandan information Letter from the Chair........................... 3 and communications Update From Headquarters............... 4-6 technology experts (ICT) at its 2009 kick- Quality Reporting Work Demo’d at NHIN Forum..................................... 7 off Working Group Meeting in Orlando, News from the PMO............................. 7 Florida, January 11-16, Why HL7 Creates Draft Standards........ 8 2009. This effort is a critical first step to Modeling CDA with Standards-Based Tools......................... 9 increased interoperabil- ity information-sharing Breakthrough in Family Health efforts between HL7 History Information Exchange...... 10-11 and ICT reform drivers Co-Chair Election Results................... 11 in both Africa and Asia. The Ugandan contin- HL7 Chair Ed Hammond, PhD, Eddie Mukooyo, MD, and HL7 CEO What the OMG Relationship Means gent is led by Eddie to HL7 Members................................ 12 Charles Jaffe, MD, PhD Mukooyo, MD, head of HL7 Benefactors................................. 12 the country’s Ministry SOA Conference In Healthcare............ 13 of Health. Uganda has served as an ICT leader active participants at the standards development since the 2003 enactment of the ICT4D National table and have our voice be heard.” HL7 Certification Exam Policy which pledges the government’s support Congratulations.................................. 14 for development of sustainable ICT initiatives The shortage of educational resources and lack Upcoming Working Group that provide quantifiable results for the benefit of of direct involvement in healthcare standards Meetings............................................ -

Nebraska Operational Ehealth Plan
Nebraska Operational eHealth Plan May 2012 Version 6 Nebraska Operational eHealth Plan 1 July 2012 This edition of Nebraska’s Strategic eHealth Plan lays out the state’s vision, goals, and objectives, and strategies for implementing statewide health information exchange and supporting the meaningful use of health information technology. The plan focuses on the domains of adoption, governance, finance, technical infrastructure, business and technical operations. Key considerations and recommendations are also included. As the eHealth Council continues to address the development of health information exchange and the adoption of health IT, the plan will be updated. Frequent revisions are anticipated due the quickly changing health IT environment. Please check the Nebraska Information Technology Commission’s website (www.nitc.nebraska.gov) for the most recent edition. May 2012 State of Nebraska Nebraska Information Technology Commission 501 S. 14th Street P.O. Box 95045 Lincoln, NE 68509-5045 (402) 471-3560 www.nitc.nebraska.gov Nebraska Operational eHealth Plan 2 July 2012 Table of Contents Privacy and Security Framework 5 • NeHII 5 • eBHIN 12 Sustainability Plan 17 • Conditions for Sustainability of Health Information Exchange 17 • Sustainability of Services Offered 19 o NeHII 19 o eBHIN 29 Project Management Plan 36 • Issues and Risks 36 • Staffing Plans 43 o State of Nebraska 43 o NeHII 45 o eBHIN 47 • Timelines and Milestones 49 o NeHII 49 o eBHIN 59 Evaluation Plan 62 • Aim 62 • Key Evaluation Questions 62 • Evaluation Framework 63