Casei Reports
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ionization Energies of Benzodiazepines Salvatore Millefiori, Andrea Alparone
Electronic properties of neuroleptics: ionization energies of benzodiazepines Salvatore Millefiori, Andrea Alparone To cite this version: Salvatore Millefiori, Andrea Alparone. Electronic properties of neuroleptics: ionization energies of benzodiazepines. Journal of Molecular Modeling, Springer Verlag (Germany), 2010, 17 (2), pp.281- 287. 10.1007/s00894-010-0723-7. hal-00590996 HAL Id: hal-00590996 https://hal.archives-ouvertes.fr/hal-00590996 Submitted on 6 May 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Editorial Manager(tm) for Journal of Molecular Modeling Manuscript Draft Manuscript Number: JMMO1191R1 Title: Electronic properties of neuroleptics: ionization energies of benzodiazepines Article Type: Original paper Keywords: Benzodiazepines; vertical ionization energies; vertical electron affinities; DFT calculations; electron propagator theory calculations. Corresponding Author: Prof. Salvatore Millefiori, Corresponding Author's Institution: First Author: Salvatore Millefiori Order of Authors: Salvatore Millefiori; Andrea Alparone Abstract: Abstract. Vertical ionization energies (VIEs) of medazepam and nordazepam and of their molecular subunits have been calculated with the electron propagator method in the P3/CEP-31G* approximation. Vertical electron affinities (VEAs) have been obtained with a ΔSCF procedure at the DFT-B3LYP/6-31+G* level of theory. Excellent correlations have been achieved between IEcalc and IEexp allowing reliable assignment of the ionization processes. -

Understanding Benzodiazephine Use, Abuse, and Detection
Siemens Healthcare Diagnostics, the leading clinical diagnostics company, is committed to providing clinicians with the vital information they need for the accurate diagnosis, treatment and monitoring of patients. Our comprehensive portfolio of performance-driven systems, unmatched menu offering and IT solutions, in conjunction with highly responsive service, is designed to streamline workflow, enhance operational efficiency and support improved patient care. Syva, EMIT, EMIT II, EMIT d.a.u., and all associated marks are trademarks of General Siemens Healthcare Diagnostics Inc. All Drugs other trademarks and brands are the Global Division property of their respective owners. of Abuse Siemens Healthcare Product availability may vary from Diagnostics Inc. country to country and is subject 1717 Deerfield Road to varying regulatory requirements. Deerfield, IL 60015-0778 Please contact your local USA representative for availability. www.siemens.com/diagnostics Siemens Global Headquarters Global Siemens Healthcare Headquarters Siemens AG Understanding Wittelsbacherplatz 2 Siemens AG 80333 Muenchen Healthcare Sector Germany Henkestrasse 127 Benzodiazephine Use, 91052 Erlangen Germany Abuse, and Detection Telephone: +49 9131 84 - 0 www.siemens.com/healthcare www.usa.siemens.com/diagnostics Answers for life. Order No. A91DX-0701526-UC1-4A00 | Printed in USA | © 2009 Siemens Healthcare Diagnostics Inc. Syva has been R1 R2 a leading developer N and manufacturer of AB R3 X N drugs-of-abuse tests R4 for more than 30 years. R2 C Now part of Siemens Healthcare ® Diagnostics, Syva boasts a long and Benzodiazepines have as their basic chemical structure successful track record in drugs-of-abuse a benzene ring fused to a seven-membered diazepine ring. testing, and leads the industry in the All important benzodiazepines contain a 5-aryl substituent ring (ring C) and a 1,4–diazepine ring. -

Retention Behaviour of Some Benzodiazepines in Solid-Phase Extraction Using Modified Silica Adsorbents Having Various Hydrophobicities
ACADEMIA ROMÂNĂ Rev. Roum. Chim., Revue Roumaine de Chimie 2015, 60(9), 891-898 http://web.icf.ro/rrch/ RETENTION BEHAVIOUR OF SOME BENZODIAZEPINES IN SOLID-PHASE EXTRACTION USING MODIFIED SILICA ADSORBENTS HAVING VARIOUS HYDROPHOBICITIES Elena BACALUM,a Mihaela CHEREGIb,* and Victor DAVIDb,* a Research Institute from University of Bucharest – ICUB, 36-46 M. Kogalniceanu Blvd., Bucharest, 050107, Roumania b University of Bucharest, Faculty of Chemistry, Department of Analytical Chemistry, 90 Panduri Ave, Bucharest – 050663, Roumania Received April 6, 2015 The retention properties of six benzodiazepines (alprazolam, bromazepam, diazepam, flunitrazepam, medazepam, and nitrazepam) on four different solid phase extraction silica 1.0 adsorbents with various hydrophobicities (octadecylsilica, octylsilica, phenylsilica, and cyanopropylsilica) were 0.8 H O investigated. The breakthrough curves showed a significant N retention of these compounds on octadecylsilica, octylsilica, 0.6 Br N phenylsilica, excepting alprazolam that has a poor retention on 0 C/C N octadecylsilica. These results can be explained by the 0.4 PHENYL CN hydrophobic character of studied benzodiazepines (octanol- C18 0.2 C8 Bromazepam water partition constant, log Kow, being situated within the interval 1.90-4.45). A poor retention on cyanopropylsilica was 0.0 observed for all studied compounds indicating that π-π and 0 102030405060708090100 Volume (mL) polar intermolecular interactions have a less significant role in their retention on this adsorbent. Generally, the breakthrough -

Benzodiazepines in Chronic Pain Why the Interest?
Why the Interest? • 33 years in chronic pain rehabilitation Benzodiazepines • Many patients are dysfunctional, depressed, in Chronic Pain regressed, and cognitively impaired while taking opioids plus benzodiazepines. • Engendered a negative attitude Edward Covington, MD • Stimulated curiosity about what we Cleveland Clinic Foundation do and do not know about these drugs in pain patients, especially in combination with opioids Disclaimer History Much of the data that I could find is quite old • For centuries, humans have sought anxiolysis, euphoria • Alcohol was followed by sedatives and anxiolytics • 19th century – Bromides (“take a powder”), choral hydrate (Mickey Finn), paraldehyde • Barbiturates synthesized in 1903 • Meprobamate in 1950 Benzodiazepine Introduction Benzodiazepine Use in America • Chlordiazepoxide introduced in 1960 • BZs are the most prescribed CNS depressants • Addictiveness and lethality of barbiturates (and similar drugs) led to their replacement by BZs • Estimated past year prevalence of BZ use in • Use of BZs increased dramatically the USA = 12.9% – US sales peaked in 1975 – Anxiolytics / hypnotics accounted for 10% of all • 14.2% of these have taken the drug ≥ 12 mo prescriptions Barker MJ et al. Arch Clin Neuropsychology 2004;19:437-454 • WHO recommended scheduling BZs in the early • About 100 million prescriptions in 1999 1980s DEA Lader, M: J Subs Abuse Treatment 1991;8:53-59 1 Mechanism of Tranquilization How Reinforcing are BZs? - • GABA binding permits Cl influx Humans • Hyperpolarizes cell, •Normal (light -

Analytical Methods for Determination of Benzodiazepines. a Short Review
Cent. Eur. J. Chem. • 12(10) • 2014 • 994-1007 DOI: 10.2478/s11532-014-0551-1 Central European Journal of Chemistry Analytical methods for determination of benzodiazepines. A short review Review Article Paulina Szatkowska1, Marcin Koba1*, Piotr Kośliński1, Jacek Wandas1, Tomasz Bączek2,3 1Department of Toxicology, Faculty of Pharmacy, Collegium Medicum of Nicolaus Copernicus University, 85-089 Bydgoszcz, Poland 2Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Medical University of Gdańsk, 80-416 Gdańsk, Poland 3Institute of Health Sciences, Division of Human Anatomy and Physiology, Pomeranian University of Słupsk, 76-200 Słupsk, Poland Received 16 July 2013; Accepted 6 February 2014 Abstract: Benzodiazepines (BDZs) are generally commonly used as anxiolytic and/or hypnotic drugs as a ligand of the GABAA-benzodiazepine receptor. Moreover, some of benzodiazepines are widely used as an anti-depressive and sedative drugs, and also as anti-epileptic drugs and in some cases can be useful as an adjunct treatment in refractory epilepsies or anti-alcoholic therapy. High-performance liquid chromatography (HPLC) methods, thin-layer chromatography (TLC) methods, gas chromatography (GC) methods, capillary electrophoresis (CE) methods and some of spectrophotometric and spectrofluorometric methods were developed and have been extensively applied to the analysis of number of benzodiazepine derivative drugs (BDZs) providing reliable and accurate results. The available chemical methods for the determination of BDZs in biological materials and pharmaceutical formulations are reviewed in this work. Keywords: Analytical methods • Benzodiazepines • Drugs analysis • Pharmaceutical formulations © Versita Sp. z o.o. 1. Introduction and long). For this reason, an application of these drugs became broader allowing their utility to a larger extent, Benzodiazepines have been first introduced into medical and at the same time, problems related to drug abuse practice in the 60s of the last century. -

A Review of the Evidence of Use and Harms of Novel Benzodiazepines
ACMD Advisory Council on the Misuse of Drugs Novel Benzodiazepines A review of the evidence of use and harms of Novel Benzodiazepines April 2020 1 Contents 1. Introduction ................................................................................................................................. 4 2. Legal control of benzodiazepines .......................................................................................... 4 3. Benzodiazepine chemistry and pharmacology .................................................................. 6 4. Benzodiazepine misuse............................................................................................................ 7 Benzodiazepine use with opioids ................................................................................................... 9 Social harms of benzodiazepine use .......................................................................................... 10 Suicide ............................................................................................................................................. 11 5. Prevalence and harm summaries of Novel Benzodiazepines ...................................... 11 1. Flualprazolam ......................................................................................................................... 11 2. Norfludiazepam ....................................................................................................................... 13 3. Flunitrazolam .......................................................................................................................... -

An Inventory of Literature on the Relation Between Drug Use, Impaired Driving and Traffic Accidents
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by National Documentation Centre on Drug Use E.M.C.D.D.A. DRUGS MISUSE RESEARCH DIVISION HEALTH RESEARCH BOARD An Inventory of Literature on the Relation between Drug Use, Impaired Driving and Traffic Accidents CT.97.EP.14 Research Team: Colin Gemmell Trinity College, Dublin Rosalyn Moran Drugs Misuse Research Division, Health Research Board James Crowley Professor, Transport Policy Research Institute, University College Dublin Richeal Courtney Medical Expert, for the Health Research Board EMCDDA: Lucas Wiessing February 1999 Please use the following citation: European Monitoring Centre for Drugs and Drug Addiction. An Inventory of Literature on the Relation betweenDrug Use, Impaired Driving and Traffic Accidents. (CT.97.EP.14) Lisbon: EMCDDA, February 1999. Contact Details Drugs Misuse Research Division Health Research Board 73 Lower Baggot Street Dublin 2 Ireland European Monitoring Centre for Drugs and Drug Addiction Rua Cruz de Santa Apolónia 23/25 1100, Lisboa Portugal. Further copies of this bibliography can be obtained from the EMCDDA at the above address. CREDITS Principal Researchers Ms Rosalyn Moran, Project Leader, Health Research Board Professor James Crowley, Professor, Transport Policy Research Institute, UCD Dr Richeal Courtney, Medical Expert, on behalf of the Health Research Board Research Assistants Colin Gemmell (Synthesis and Final Reports) Sarah Heywood (Literature Search and Collaborative Network) For the EMCDDA Lucas Wiessing -

Apo-Bromazepam
PRODUCT MONOGRAPH APO-BROMAZEPAM bromazepam 1.5 mg, 3 mg and 6 mg Tablets Anxiolytic - Sedative APOTEX INC. Date of Revision: 150 Signet Drive March 10, 2016 Toronto, Ontario M9L 1T9 Control No.: 192477 1 Table of Contents PART I: HEALTH PROFFESSIONAL INFORMATION .................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................. 3 INDICATIONS AND CLINICAL USE ................................................................................... 3 CONTRAINDICATIONS ........................................................................................................ 4 WARNINGS AND PRECAUTIONS ....................................................................................... 4 ADVERSE REACTIONS ......................................................................................................... 9 DRUG INTERACTIONS ....................................................................................................... 11 DOSAGE AND ADMINISTRATION ................................................................................... 12 OVERDOSAGE ...................................................................................................................... 14 ACTION AND CLINICAL PHARMACOLOGY ................................................................. 15 STORAGE AND STABILITY ............................................................................................... 16 DOSAGE FORMS, COMPOSITION AND PACKAGING ................................................. -

Mental Disorders and Illicit Drug Use Expert Group
Global Burden of Disease Mental Disorders and Illicit Drug Use Expert Group Fiona Charlson, Louisa Degenhardt, Jennifer McLaren, Wayne Hall and Michael Lynskey Benzodiazepine-related mortality Illicit Drugs Discussion Paper No. 1 GBD2005 Mental Disorders and Illicit Drug Use Expert Group www.gbd.unsw.edu.au BENZODIAZEPINE-RELATED MORTALITY Fiona Charlson, Louisa Degenhardt, Jennifer McLaren, Wayne Hall and Michael Lynskey Illicit Drugs Discussion Paper No. 1 Recommended citation: Charlson, F., Degenhardt, L., McLaren, J., Hall, W., & Lynskey, M. (2008). Benzodiazepine- related mortality. Global Burden of Disease Mental Disorders and Illicit Drug Use Expert group, Illicit drugs discussion paper No. 1. National Drug and Alcohol Research Centre, University of NSW: Sydney. ISBN: 978 0 7334 2688 9 ©NATIONAL DRUG AND ALCOHOL RESEARCH CENTRE, UNIVERSITY OF NEW SOUTH WALES, SYDNEY, 2008 This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use or use within your organisation. All other rights are reserved. Requests and enquiries concerning reproduction and rights should be addressed to the information manager, National Drug and Alcohol Research Centre, University of New South Wales, Sydney,NSW 2052, Australia. GBD2005 Mental Disorders and Illicit Drug Use Expert Group www.gbd.unsw.edu.au Table of contents Summary and recommendations .............................................................................................. 1 1. Introduction -
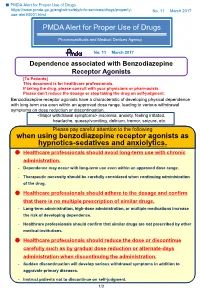
PMDA Alert for Proper Use of Drugs When Using Benzodiazepine
■ PMDA Alert for Proper Use of Drugs https://www.pmda.go.jp/english/safety/info-services/drugs/properly- No. 11 March 2017 use-alert/0001.html PMDA Alert for Proper Use of Drugs Pharmaceuticals and Medical Devices Agency No. 11 March 2017 Dependence associated with Benzodiazepine Receptor Agonists [To Patients] This document is for healthcare professionals. If taking the drug, please consult with your physicians or pharmacists. Please don’t reduce the dosage or stop taking the drug on self-judgment. Benzodiazepine receptor agonists have a characteristic of developing physical dependence with long-term use even within an approved dose range, leading to various withdrawal symptoms on dose reduction or discontinuation. <Major withdrawal symptoms> insomnia, anxiety, feeling irritated, headache, queasy/vomiting, delirium, tremor, seizure, etc. Please pay careful attention to the following when using benzodiazepine receptor agonists as hypnotics-sedatives and anxiolytics. Healthcare professionals should avoid long-term use with chronic administration. - Dependence may occur with long-term use even within an approved dose range. - Therapeutic necessity should be carefully considered when continuing administration of the drug. Healthcare professionals should adhere to the dosage and confirm that there is no multiple prescription of similar drugs. - Long-term administration, high-dose administration, or multiple medications increase the risk of developing dependence. - Healthcare professionals should confirm that similar drugs are not prescribed by other medical institutions. Healthcare professionals should reduce the dose or discontinue carefully such as by gradual dose reduction or alternate-days administration when discontinuing the administration. - Sudden discontinuation will develop serious withdrawal symptoms in addition to aggravate primary diseases. -
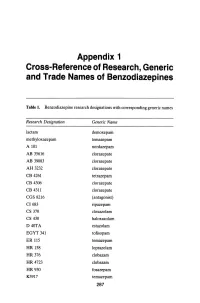
Appendix 1 Cross-Reference of Research, Generic and Trade Names of Benzodiazepines
Appendix 1 Cross-Reference of Research, Generic and Trade Names of Benzodiazepines Table 1. Benzodiazepine research designations with corresponding generic names Research Designation Generic Name lactam demoxepam methyloxazepam temazepam A 101 nordazepam AB 35616 clorazepate AB 39083 clorazepate AH 3232 clorazepate CB 4261 tetrazepam CB 4306 clorazepate CB 4311 clorazepate CGS 8216 (antagonist) CI683 ripazepam CS 370 cloxazolam CS 430 haloxazolam D40TA estazolam EGYT 341 tofisopam ER 115 temazepam HR 158 loprazolam HR376 clobazam HR 4723 clobazam HR930 fosazepam K3917 temazepam 287 THE BENZODIAZEPINES Research Designation Generic Name LA 111 diazepam LM 2717 clobazam ORF 8063 triflubazam Ro 4-5360 nitrazepam Ro 5-0690 chlordiazepoxide Ro 5-0883 desmethy1chlordiazepoxide Ro 5-2092 demoxepam Ro 5-2180 desmethyldiazepam Ro 5-2807 diazepam Ro 5-2925 desmethylmedazepam Ro 5-3059 nitrazepam Ro 5-3350 bromazepam Ro 5-3438 fludiazepam Ro 5-4023 clonazepam Ro 5-4200 flunitrazepam Ro 5-4556 medazepam Ro 5-5345 temazepam Ro 5-6789 oxazepam Ro 5-6901 flurazepam Ro 15-1788 (antagonist) Ro 21-3981 midazolam RU 31158 loprazolam S 1530 nimetazepam SAH 1123 isoquinazepam SAH 47603 temazepam SB 5833 camazepam SCH 12041 halazepam SCH 16134 quazepam U 28774 ketazolam U 31889 alprazolam U 33030 triazolam W4020 prazepam We 352 triflubazam 288 RESEARCH, GENERIC AND TRADE NAMES Research Designation Generic Name We 941 brotizolam Wy 2917 temazepam Wy 3467 diazepam Wy 3498 oxazepam Wy 3917 temazepam Wy 4036 lorazepam Wy 4082 lormetazepam Wy 4426 oxazepam Y 6047 -

Benzodiazepine Assay
2 SUmmARy Benzodiazepines are sedative-hypnotic drugs that are structurally similar and include widely used drugs such as chlordiazepoxide, diazepam, and oxazepam. The different benzodiazepines are absorbed at different rates, and the timing of their psychoactive effects varies with the absorption rate. Benzodiazepines are usually taken orally and are metabolized in the liver. Some benzodiazepine metabolites are pharmacologically active.2 Benzodiazepines potentiate the effect Benzodiazepine Assay of other central nervous system depressants, such as ethyl alcohol.3 The Emit® II Plus Benzodiazepine Assay, an enzyme immunoassay technique, tests for benzodiazepines and their metabolites in human urine. Positive results for specimens containing September 2010 9F052.4D_E other compounds structurally unrelated to benzodiazepines have not been observed. The cutoff levels for distinguishing positive from negative specimens are 200 ng/mL and 300 ng/mL. Methods historically used for detecting benzodiazepines in biological fluids include gas chromatography with electron-capture4 or flame-ionization detection,5 high-performance liquid chromatography,6 thin-layer chromatography,7 fluorescence-TLC densitometry,8 enzyme immunoassay,9 and radioimmunoassay.10 While confirmation techniques other than GC/MS may be adequate for some drugs of abuse, GC/MS is generally accepted as a vigorous confirmation technique for all drugs, since it provides the best level of confidence in the result.1 Catalog Quantity/ 3 mEThODOLOgy Number Product Description Volume OSR9F229 Emit® II Plus Benzodiazepine Assay The Emit® II Plus Benzodiazepine Assay is a homogeneous enzyme immunoassay technique used for the analysis of specific compounds in human urine.11 The assay is based on competition OSR9F618 R1 (Antibody/Substrate Reagent 1) 2 x 31 mL between drug in the specimen and drug labeled with the enzyme glucose-6-phosphate dehydrogenase (G6PDH) for antibody binding sites.