Guidance on Contingency Planning for People Who Use Drugs and COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
UCD Commuting Guide
University College Dublin An Coláiste Ollscoile, Baile Átha Cliath CAMPUS COMMUTING GUIDE Belfield 2015/16 Commuting Check your by Bus (see overleaf for Belfield bus map) UCD Real Time Passenger Information Displays Route to ArrivED • N11 bus stop • Internal campus bus stops • Outside UCD James Joyce Library Campus • In UCD O’Brien Centre for Science Arriving autumn ‘15 using • Outside UCD Student Centre Increased UCD Services Public ArrivED • UCD now designated a terminus for x route buses (direct buses at peak times) • Increased services on 17, 142 and 145 routes serving the campus Transport • UCD-DART shuttle bus to Sydney Parade during term time Arriving autumn ‘15 • UCD-LUAS shuttle bus to Windy Arbour on the LUAS Green Line during Transport for Ireland term time Transport for Ireland (www.transportforireland.ie) Dublin Bus Commuter App helps you plan journeys, door-to-door, anywhere in ArrivED Ireland, using public transport and/or walking. • Download Dublin Bus Live app for updates on arriving buses Hit the Road Don’t forget UCD operates a Taxsaver Travel Pass Scheme for staff commuting by Bus, Dart, LUAS and Rail. Hit the Road (www.hittheroad.ie) shows you how to get between any two points in Dublin City, using a smart Visit www.ucd.ie/hr for details. combination of Dublin Bus, LUAS and DART routes. Commuting Commuting by Bike/on Foot by Car Improvements to UCD Cycling & Walking Facilities Parking is limited on campus and available on a first come first served basis exclusively for persons with business in UCD. Arrived All car parks are designated either permit parking or hourly paid. -

Liberating Learning. a Study of Daytime Education Groups in Ireland. INSTITUTION AONTAS, Dublin (Ireland).;University Coll., Dublin (Ireland)
DOCUMENT RESUME ED 374 220 CE 067 110 AUTHOR Inglis, Tom; And Others TITLE Liberating Learning. A Study of Daytime Education Groups in Ireland. INSTITUTION AONTAS, Dublin (Ireland).;University Coll., Dublin (Ireland). REPORT NO ISBN-0-906826-03-9 PUB DATE 93 NOTE 105p. AVAILABLE FROMAONTAS, 22 Earlsfort Terrace, Dublin 2, Ireland (5.99 Irish pounds). PUB TYPE Reports Research/Technical (143) Tests /Evaluation Instruments (160) EDRS PRICE MF01/PC05 Plus Postage. DESCRIPTORS Access to Education; *Adult Education; *Day Programs; Educational Research; Foreign Countries; Lifelong Learning; Noncredit Courses; *Nonformal Education; *Womens Education IDENTIFIERS *Ireland ABSTRACT A study examined daytime education groups, a major phenomenon in Irish adult education. Results showed that 96 groups were operating, mostly in suburban areas, particularly Dublin. These groups had 8,723 adults participating in their courses and programs. What made them unique was their voluntary, locally based nature. The groups received little or no recognition, encouragement, or support from the Department of Education. They were generally dependent on local level support. More than half operated from private homes. Two-thirds rented premises. One in three did not have any insurance coverage for their activities. Two-thirds provided child care, which approximately one-fifth of the participants used. The groups provided a large number and wide range of educational courses and programs. In contrast to statutory providers, the groups had greater control over the whole process. Although crafts and skill-based learning were still emphasized. the main type of learning was oriented toward social and personal understanding. Most courses were run on a strict self-financing basis. -

Some Useful Contact Numbers Teeth and a Healthy Smile Health Centres with Dental Clinics
Helpful tips for healthy Some useful contact numbers teeth and a healthy smile Health Centres with Dental Clinics • To keep teeth healthy, cut down on how Dublin North West often you take sugary drinks and foods, • Roselawn Rd., Blanchardstown 01-646 4550 especially between meals. • Quarry Rd., Cabra 01-868 0762 • Brush your teeth and gums with a pea size • Wellmount Park, Finglas 01-856 7700 amount of fluoride toothpaste twice a day. • Ballygall Rd., Finglas 01-884 5000 • Children under 2 years should not use • Cherryfield Lawn, Hartstown 01-866 2831 fluoride toothpaste when toothbrushing. Dublin North • Supervise toothbrushing in children under 7 • Cromcastle Rd., Coolock 01-816 4232 years to help them clean their teeth properly. • Bridge St., Swords 01-840 4633 • Do not miss your • New St., Malahide 01-845 0256 dental appointments. They are offered at important stages • Willie Nolan Rd., Baldoyle 01-839 2331 of development of your child’s mouth. • Thomas Hand St., Skerries 01-849 4916 • Please bring your childs PPS number • Hampton St., Balbriggan 01-841 3543 when using the dental services. • Lusk, Co. Dublin 01-870 9018 • Oldtown 01-807 8828 • Darndale Health Centre 01-877 1561 • Foxfield Cresent, Kilbarrack 01-839 1221 Dublin North Central • North Strand Rd., North Strand 01-855 6466 • Griffith Ave., Marino 01-833 3421 • Main Street, Ballymun 01-846 7160 • Larkhill 01-837 3796 How does the service work? Prevention orientated service The dental team is made up of Dental hygienists are specially trained • the dentist • the dental hygienist members of the dental team. They play an • the oral health promoter • the dental nurse important role in the dental health of your They work together to provide a quality child. -
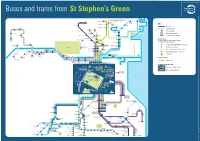
Buses and Trams from St Stephen's Green
142 Buses and trams from St Stephen’s Green 142 continues to Waterside, Seabury, Malahide, 32x continues to 41x Broomfield, Hazelbrook, Sainthelens and 15 Portmarnock, Swords Manor Portmarnock Sand’s Hotel Baldoyle Malahide and 142 Poppintree 140 Clongriffin Seabury Barrysparks Finglas IKEA KEY Charlestown SWORDS Main Street Ellenfield Park Darndale Beaumont Bus route Fosterstown (Boroimhe) Collinstown 14 Coolock North Blakestown (Intel) 11 44 Whitehall Bull Tram (Luas) line Wadelai Park Larkhill Island Finglas Road Collins Avenue Principal stop Donnycarney St Anne’s Park 7b Bus route terminus Maynooth Ballymun and Gardens (DCU) Easton Glasnevin Cemetery Whitehall Marino Tram (Luas) line terminus Glasnevin Dublin (Mobhi) Harbour Maynooth St Patrick’s Fairview Transfer Points (Kingsbury) Prussia Street 66x Phibsboro Locations where it is possible to change Drumcondra North Strand to a different form of transport Leixlip Mountjoy Square Rail (DART, COMMUTER or Intercity) Salesian College 7b 7d 46e Mater Connolly/ 67x Phoenix Park Busáras (Infirmary Road Tram (Luas Red line) Phoenix Park and Zoo) 46a Parnell Square 116 Lucan Road Gardiner Bus coach (regional or intercity) (Liffey Valley) Palmerstown Street Backweston O’Connell Street Lucan Village Esker Hill Abbey Street Park & Ride (larger car parks) Lower Ballyoulster North Wall/Beckett Bridge Ferry Port Lucan Chapelizod (142 Outbound stop only) Dodsboro Bypass Dublin Port Aghards 25x Islandbridge Heuston Celbridge Points of Interest Grand Canal Dock 15a 15b 145 Public Park Heuston Arran/Usher’s -

Constituency of Dublin Central
Dublin Central Constituency of Dublin Central 2019/20 Polling Place Polling Polling District PD Voters Voters Table Polling Station Code From To Totals District Totals Old School House 229 Arran Quay A WA 1 909 909 909 30 Phibsboro Road Dublin 7 Stanhope St. N.S. Hall, 230 Arran Quay B WB 1 591 591 1903 Manor Street, 231 592 1228 637 Dublin, 7 232 1229 1903 675 St. Paul`s CBS 233 Arran Quay C WD 1 624 624 1709 Brunswick St. North 234 625 1251 627 Dublin 7 235 1252 1709 743 ( Inns Quay C WP 1 285 1400 236 Inns Quay C WP 286 1003 718 237 1004 1400 693 ( North City 1 WS 1 296 1072 238 North City 1 WS 297 1072 776 239 Rotunda B WY 1 770 770 770 St Gabriels N.S. 240 Arran Quay D WE 1 534 534 1847 Cowper Street 241 535 1198 664 Dublin 7 242 1199 1847 649 243 Arran Quay E WF 1 694 694 2189 244 695 1444 750 245 1445 2189 745 North Strand Church Parish Hall 246 Ballybough A WG 1 498 498 2237 (formerly St Columbas) 247 499 1107 609 North Strand 248 1108 1793 686 Dublin 3 249 1794 2237 696 ( North Dock A WU 1 252 996 250 North Dock A WU 253 996 744 O'Connell`s Secondary School 251 Ballybough B WJ 1 552 552 1661 North Richmond Street 252 553 1241 689 off North Circular Road 253 1242 1661 725 Dublin 1 ( Drumcondra South B WL 1 305 1038 254 Drumcondra South B WL 306 1038 733 St.Brigid's Nursery 255 Mountjoy B WR 1 536 536 1147 Mountjoy Square Park North 256 537 1147 611 Dublin 1 St. -

Eastp Int Business Park Dublin’S Premier Business Park
To Let by Way of Sublease or Assignment Pinnacle 2 (Block 9) EASTP INT BUSINESS PARK DUBLIN’S PREMIER BUSINESS PARK Overview • Fully fitted offices • Mix of open plan and cellular accommodation • Secure bicycle and car spaces • Available immediately • Excellent transport links • Established business park location block g DART Lines Clontarf Clontarf LUAS Lines a Station location Road Cafes & Russell Street Services Restaurants Dublin Port Tunnel Eastpoint Business Park is Irelands most Ballybough East Wall Road prestigious and successful business North Strand Road Links Childcare Creche Insomnia campus. The park is strategically located Dorset Street Lower a short distance from the city centre and Our Pharmacy Blockburger Summerhill ParadeConnolly Docklands Station IFSC. The park also benefits from ease Bleeper Bike Emer’s Kitchen O’Connell Street Docklands of access to the Dublin port tunnel and Payzone Eastpoint Market every Rail Station IFSC Docklands M50. Eastpoint Business Park provides Wednesday SPOORSE Dry Cleaning City Centre occupants with a different setting to that Custom House Quay The PointVillage of the city centre with it’s landscaped North Wall Quay gardens and waterfront walks whilst still Tara St Station being situated next to Dublin’s Central Leisure Hotels Business District. Pearse St Pearse Station Street It comes with no surprise that some Clontarf GAA Clontarf Castle Mount Street Lower DART Depotof the world’s largest companies such City Motocross5 a-side football pitch The Gibson Hotel Grand Canal Street Dublin Club as Google, Oracle, Datalex and British Odeon Cinema Point The Marker d P village Airwaysoa have chosen Eastpoint Business ort Tu R Hilton Garden Inn e Ballsbridge Up Line n yr Park as their Irish hub. -

Obituaries, Death Notices, Etc. - G
Obituaries, death notices, etc. - G Surname Forename Date of Newspaper Address Notes Gabbet John 11/04/1815 Clare St. Gabbet Joseph jun., Rev. 07/08/1858 London Gabbet Mary 22/10/1823 Glenwood Gabbet William 28/12/1861 Strand House aged 65, burried at Cahernarry Gabbett Alicia 09/10/1833 Tontine Buildings Gabbett Alicia 23/03/1839 Strand House wife of Daniel Gabbett, buried at Cahirconlish Gabbett Angel Catherine 01/04/1890 Surrey death notice, widow of Mathew Richard Gabbett of Ballybrood, Co. Limerick Gabbett Anne 05/09/1817 Thomas Street Gabbett Augusta 15/02/1896 5 Orsett Terrace, Hyde Park, London dau of Butler Thornton of Skerton, Lancashire, wife of Daniel Fitzgerald Gabbett of Cahirconlish Gabbett Charlotte Maria 27/01/1874 Eden Terrace wife of Poole Gabbett; death notice Gabbett Daniel 15/01/1848 Strand House solicitor, int. at Caherconlish; (death report 15/01/1848) Gabbett Daniel 21/10/1857 Bellfield, North Strand Gabbett Daniel Fitzgerald 21/07/1852 aged 23, late 12th Lancers; removal from res of his uncle, Rev. Joseph Gabbett, Ardvallen, Kilmallock; int at Cahirconlish; (funeral report 21/07/1852) Gabbett Daniel Fitzgerald 06/08/1898 Caherconlish House aged 56, former M.P. for Limerick, d. in London (further report 09/08/1898) Gabbett Deborah 17/09/1870 1 Tontine Buildings widow of late Richard Gabbett Gabbett Deborah Alicia 04/12/1850 Thornville, nr Limerick City dau of Daniel Gabbett Surname Forename Date of Newspaper Address Notes Gabbett Diana 05/02/1851 Corbally House, Limerick wife of Thomas Gabbett, dau of Major Creagh of Carrigerry, co. -

Cycle Network Plan Draft Greater Dublin Area Cycle Network Plan
Draft Greater Dublin Area Cycle Network Plan Draft Greater Dublin Area Cycle Network Plan TABLE OF CONTENTS PART 1: WRITTEN STATEMENT 3.8. Dublin South East Sector ................................................................................................ 44 INTRODUCTION 3.8.1 Dublin South East - Proposed Cycle Route Network........................................................... 44 CHAPTER 1 EXISTING CYCLE ROUTE NETWORK ....................................................... 1 3.8.2 Dublin South East - Proposals for Cycle Route Network Additions and Improvements...... 44 3.8.3 Dublin South East - Existing Quality of Service ................................................................... 45 1.1. Quality of Service Assessments ........................................................................................1 CHAPTER 4 GDA HINTERLAND CYCLE NETWORK ................................................... 46 1.2. Existing Cycling Facilities in the Dublin City Council Area..................................................1 4.1 Fingal County Cycle Route Network................................................................................ 46 1.3. Existing Cycling Facilities in South Dublin County Area.....................................................3 4.1.1 South Fingal Sector.............................................................................................................. 46 1.4. Existing Cycling Facilities in Dun Laoghaire-Rathdown Area .............................................5 4.1.2 Central Fingal Sector -

An Exploration of the Life of Percy Ludgate
© Brian Coghlan 2019 An exploration of the life of Percy Ludgate Presented to the West Cork History Festival 10-Aug-2019 Dr.Brian Coghlan School of Computer Science and Statistics Trinity College Dublin © Brian Coghlan 2019 Why is he important ? © Brian Coghlan 2019 Percy Ludgate: why is he important ? • 2nd person in history to design general-purpose computer General-purpose computer == analytical machine & vice-versa In theory can solve any solvable problem • Two mechanical designs before the electronic computer era: 1843: Charles Babbage’s analytical engine 1909: Percy Ludgate’s analytical machine – very different • Subsequently: c.1914: Electromechanical designs begun c.1937: Electronic designs begun © Brian Coghlan 2019 Percy Ludgate: why is he important ? • He was Irish 1883-1922: born, lived, died in Ireland • Worked in Dublin, published in Scientific Proc. Royal Dublin Society 1991: Ludgate Prize Computer Science at Trinity College Dublin • He was born in Skibbereen 2016: Ludgate Hub opened in Skibbereen © Brian Coghlan 2019 Mysteries © Brian Coghlan 2019 Percy Ludgate: mysteries • Percy Ludgate died young and single in 1922 aged 39 By 1987 there were no other descendants of his parents So records are scant. Randell said: “an archivist stated that by all normal criteria, it was clear that he had never existed” • Yet he did exist, with large number of relatives and acquaintances First objective == related documents, photos, memories Do they still exist ? If so, where ? © Brian Coghlan 2019 Percy Ludgate: mysteries • His 1909 paper -

The Irish Volunteers in North Co. Dublin, 1913-17
Title The Irish Volunteers in north Co. Dublin, 1913-17 By Peter Francis Whearity SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MA IN LOCAL HISTORY DEPARTMENT OF HISTORY NATIONAL UNIVERSITY OF IRELAND MAYNOOTH Supervisor of research: Dr Terence A. Dooley December 2011 Contents Page Illustrations iii Abbreviations iv Acknowledgment v Map 1 specifically made for this study vi Map 2 Ordnance Survey of Ireland, Townland Index, for County Dublin vii Introduction 1 Chapter 1 The formation of the Irish Volunteer movement 10 Chapter 2 The National Volunteer movement 28 Chapter 3 The Redmondite-split and its aftermath 47 Chapter 4 The 1916 Rising in north County Dublin 68 Chapter 5 The aftermath of the Rising 88 Conclusion 111 Appendix 121 Bibliography 134 List of Tables Table 1 Irish Volunteer companies formed in north County Dublin up to 11 June 1914 27 Table 2 Irish national Volunteer companies formed after 11 June 1914 45 Table 3 National Volunteer companies at the time of the Redmondite-split 58 Table 4 County Dublin Volunteer membership figures for the period beginning July 1914, until Apr. 1916 67 Table 5 Places in north County Dublin from where arrested men came from after the Rising 90 i Table 6 Age profiles of north County Dublin men arrested after the Rising 92 Table 7 Marital status of north County Dublin men arrested after the 1916 Rising 93 Table 8 Occupational profiles of north County Dublin men arrested after the Rising 94 Table 9 Category A prisoners from north County Dublin after the Rising 96 Table 10 Category B prisoners from north County Dublin after the Rising 97 Table 11 Category C prisoners from north County Dublin after the Rising 98 Table 12 Classification of arrested north County Dublin men on R.I.C. -

Greening Strategy DRAFT 2018
Greening Strategy DRAFT 2018 All plans shown in this document are preliminary and for the purposes of discussion only and are not fixed, all plans will be subject to further consultation Contents Introduction Page 1 3.6 Tree Planting Strategy 3.7 Future Tree Planting Projects 3.8 Micro-Projects 1.0 The Greening Strategy Study Area Page 2 3.9 Project Phasing 1.1 The North East Inner City - Local Context 1.2 History and Heritage 1.3 The Dublin Docklands, Canals and Railways 1.4 Cultural Heritage 1.5 2018: Current context of the North East Inner City 1.6 Demographics 1.7 Planning Context 2.0 The ‘Green Infrastructure’ Audit Page 6 2.1 The Study Area 2.2 The Audit : Methodology and Site Appraisal 2.3 Urban Form 2.4 Landscape Quality 2.5 Deficit of quality ‘Green Infrastructure’ 2.6 Existing Green Space Audit 2.7 Public Consultation 3.0 The ‘Green Infrastructure’ Vision & Strategy Page 15 3.1 The ‘Green Infrastructure’ Vision 3.2 The Health Benefits of ‘Green Infrastructure’ and ‘Open Space’ (International Best Practice) 3.3 The Strategic Objectives and Benefits of the ‘Green Infrastructure’ Strategy 3.4 The ‘Green Infrastructure’ Strategy 3.5 Open Space Projects 2 Introduction The North East Inner City Greening Strategy was initiated by Dublin City Council, based on the recommendations of The parks, landscape development and future management within Dublin City. The North East Inner City Greening Strategy Mulvey Report. The report entitled ‘Dublin North East Inner City: Creating A Brighter Future: The Social And Economic can be viewed in the context of the wider vision, and utilises the success of the Liberties Greening Strategy (2015) as Regeneration Of Dublin’s North East Inner City’ was brought about as a response to the gangland murders in the North an example to follow. -

Community and Social Infrastructure Audit for Lands at Holy Cross College, Clonliffe Road, Dublin 3 and Drumcondra Road Lower, Drumcondra, Dublin 9
HOLY CROSS COLLEGE SHD Community and Social Infrastructure Statement STRATEGIC HOUSING DEVELOPMENT PLANNING APPLICATION COMMUNITY AND SOCIAL INFRASTRUCTURE AUDIT FOR LANDS AT HOLY CROSS COLLEGE, CLONLIFFE ROAD, DUBLIN 3 AND DRUMCONDRA ROAD LOWER, DRUMCONDRA, DUBLIN 9 CLIENT CWTC Multi Family ICAV acting on behalf of its sub-fund DBTR DR1 Fund DATE 3rd May 2021 1 HOLY CROSS COLLEGE SHD Community and Social Infrastructure Audit Contents Amendment Record This report has been issued and amended as follows: Issue Revision Description Date Prepared Checked by by 01 00 Draft 01/10/2020 DF PB 01 01 Final Draft for Pre-App 13/11/2020 DF PB 02 00 Final for Application 03/05/2021 ST PB Brady Shipman Martin www.bradyshipmanmartin.com DUBLIN Canal House Canal Road Dublin 6 + 353 1 208 1900 CORK Penrose Wharf Business Centre Penrose Wharf Cork +353 21 242 5620 LIMERICK 11 The Crescent Limerick +353 61 315 127 [email protected] 2 HOLY CROSS COLLEGE SHD Community and Social Infrastructure Statement TABLE OF CONTENTS 1. INTRODUCTION .................................................................................. 5 1.1 Dublin City Development Plan 2016-2022 ................................................... 5 1.2 Proposed Development ................................................................................ 6 1.3 Methodology ................................................................................................ 6 2. OVERVIEW OF COMMUNITY AND SOCIAL INFRASTRUCTURE ............ 7 2.1 Social / Community Facilities .......................................................................