Theses Digitisation: This Is a Digitised
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Papers in Illinois History and Transactions for the Year
Publication Number Twenty-three OF THE ILLINOIS STATE HISTORICAL LIBRARY TRANSACTIONS OF THE Illinois State Historical Society FOR THE YEAR 1917 Eighteenth Annual Meeting of the Society, Springfield, Illinois, May 10-11, 1917 [Printed by authority of the State of Illinois.] Springfield, III. Illinois State Jouenal Co., State Printers. 19 17 282S—3M CONTENTS. PAGIC. Officers of the Society 5 Editorial Note 7 Constitution of the Illinois State Historical Society 8 An appeal to the Historical Society and the General Public 11 PART I.—RECORD OF OFFICIAL PROCEEDINGS, ANNUAL MEETING, 1917. Annual Meeting 15 Business Meeting 17 In Memoriam. John Howard Burnham. By Jessie Palmer Weber 32 James Haines. By W. R. Curran 37 PART II.—PAPERS READ AT THE ANNUAL MEETING, 1917. Jenkin Lloyd Jones, Annual Address. Contemporary Vandalism 47 Ernest L. Bogart. The Population of Illinois, 1870-1910 64 Verna Cooley. Illinois and the Underground Railroad to Canada 76 Stephen A. Day. A celebrated Illinois Case that made History 99 George A. Rogers. Reading, Reverie of Fifty Years. By Clark E. Carr. .109 P. C. Croll, D. D. Thomas Beard, the Pioneer and Founder of Beards- town, Illinois Ill Arthur C. Cole. Lincoln and the Presidential Election of 1864 130 PART III.—CONTRIBUTIONS TO STATE HISTORY. John Reynolds. The Agricultural Resources of Southern Illinois. Re- printed from Transactions of the Illinois State Agricultural Society, Vol. II., 1856 141 Index 161 List of Publications of the Illinois State Historical Library and Society.. 185 OFFICERS OF THE SOCIETY. Honorary President. Hon. Clark E. Carr Galesburg President. Dr. Otto L. Schmidt Chicago First Vice President. -

Heritage Highlights P a G E 2 a Note from the Director’S Desk
July, 2019 Heritage Volume 7 Highlights A Piece of History in Motion We were blessed with the dona- son’s sewing machines at Wa- tion feed invented by Allen B tion of a Civil War era Wheeler tertown, New York. To start Wilson (1824-1888). The under & Wilson treadle driven sewing with, production was slow, how- thread is contained in a disc machine which is now on dis- ever, by the bobbin which fits play in our ‘sewing room.’ One early years of loosely in a ring- of the most ingenious of the the 1860’s, it shaped holder sewing machine inventors was had increased that looks like a Mr. Allen B. Wilson. Born in from 20,000 to thin, metal Inside This Issue: New York in 1824, he later 30,000 & then doughnut. Inter- moved to Michigan where he 50,000 ma- locking of the two A Note from the 2 made a living as a journeyman chines, peak- threads occurs Director’s Desk cabinet maker. Around 1840 he ing a decade when the loops of Archivist’s Notes 2 began the development of a later at over the needle thread sewing machine, which was 128,000 per are caught & independent of the efforts being year. In 1856, extended by the A drawing of a treadle driven sewing Highlighting a Hero 3 made by other inventors in New the company revolving hook & England. In 1849 he devised was renamed machine taken from a 19th century passed under the the rotary hook and bobbin com- the Wheeler & Wheeler & Wilson advertisement bobbin. -

1940-Commencement.Pdf
c~ h' ( c\ '.\.\.\.. ( ~A { I , .f \,.' I f ;' \ . \ J University of Minnesota IJ • COMMENCEMENT CONVOCATION WINTER QUARTER 1940 NORTHROP MEMORIAL AUDITORIUM Thursday, March 21, 1940, Eleven O'Clock I I , ~ \ ' ,i ii, iii, ;, ' PROGRAM PRESIDENT GUY STANTON FORD, Presiding PROCESSIONAL-Finale from the Fourth Symphony Widor ARTHUR B. JENNINGS University Organist HYMN-"America" My country I 'tis of thee, Our fathers' God I to Thee, Sweet land of liberty, Author of Liberty, Of thee I sing; To Thee we sing; Land where our fathers died I Long may our land be bright Land of the Pilgrims' pride, With freedom's holy light; From every mountain side Protect us by Thy might Let freedom ring. Great God, our King I COMMENCEMENT ADDRESS- "Of Human Intercourse" HENRY NOBLE MACCRACKEN, Ph.D., LL.D., L.H.D. President, Vassar College CONFERRING OF DEGREES GUY STANTON FORD, Ph.D., LL.D., Litt.D., L.H.D. President of the University 2 ',' J I SONG-"Hail, Minnesota!" Minnesota, hail to thee I Like the stream that bends to sea, Hail to thee, our College dear I Like the pine that seeks the blue I Thy light shall ever be Minnesota, still for thee, A beacon bright and clear; Thy sons are strong and true. Thy sons and daughters true From thy woods and waters fair, Will proclaim thee near and far; From thy prairies waving far, They will guard thy fame At thy call they throng, And adore thy name; With their shout and song, Thou shalt be their Northern Star. Hailing thee their Northern Star. -

Monterey County, Are Looking at $10 the Figures and Conceding Defeat
Kiosk In This Issue Stillwell Children’s Pool Open! @ Lovers Point Until September 1 Fridays, Saturdays & Sundays (+ Labor Day) Noon-4:30 PM Monday-Thursday (starting June 9) 2:30 PM - 4:30 PM Weekdays - $2.00 per person Weekends - $4.00 per person Appointed - Page 7 And they’re off! - Page 11 Wharf Walk - Page 14 • June-August Summer preschool Mayflower Church 831-373-0226 Pacific Grove’s • Fri. June 6 First Friday Downtown Pacific Grove • Sat. June 7 Poetry in the Grove “Poets Laureate” Little House in Jewell Park 4-6 PM Free Times • June 6-12, 2014 Your Community NEWSpaper Vol. VI, Issue 39 Sat. June 7 First Saturday Book Sale PG Public Library Can you see it? • Sat. June 14 Measure O Howard Burnham as the 1st Earl of Halifax The Little House in Jewel Park goes down $10 “It ain't over 'til it's over,” as Yogi 5:30 p.m. Berra said, but even though some 22,969 • mail ballots and ballots delivered to poll- Thurs. June 19 ing places remain to be hand-counted, it's Meet The Author probably over for Measure O. Supporters of Peter Fischer the initiative, which would require a study PG Public Library into public ownership of water for a great Suggested donation portion of Monterey County, are looking at $10 the figures and conceding defeat. nonmembers • Public Water Now co-founder George Fri. June 20 Riley, the driving force behind Measure O, Avoiding Mail & Phone Scams said that he and Ron Cohen, Public Water on the Elderly Now's president, are likely going to close it Paul Gregory of Merrill, Lynch down soon and will not pursue public water Co-Sponsored by Madonna for a while yet. -

A. Sale of "Small Goods" W
TIIE SUNDAY OREGOXIAX, PORTLAND, NOVEMBER 3. 1913. 12. a pf living-roo- and which were so successful season sen's Hall, Friday, December Club member their friends assembled adorned the halls last George C. Denholm, S, at their home, 595 East Twenty-fift- h dining-roo- A large number of friends will begin again on Friday evening, members aTe: street, last Sunday. An elaborate sup- shared the pleasures of the affair. November 7 and will be held every G. Kirkland. W. K. Slater, William L. per was served and games and music first and. third Friday evenings. The Lightner, Carl Rosengreen; Fred S. enjoyed. Those present were: Mr. and Mrs. Jennie E. Burnham was hostess dancing parties will be held, on the Johnson, Harold Wilson, Roy Entler. Mrs. August Roeder, Rev. and Mrs. A. this week at a dinner party given In second, and fourth Friday evenings. Patronesses will be: Mrs. G. H. Den- Krause, Mr. and Mrs. G. Hoehlen and honor of Vancouver friends. Cards Every Friday evening will be club holm, Mrs. W. S. Johnson, Mrs. W. K. boy-shoul- d family, Mr. and Mrs. E. Keitzel, Mr. were laid for the following guests: night. The regular notices heretofore Slater, Mrs. Alfred Kirkland. Shelves full of Every Mrs. C. M. Hemmlch, Mr. mailed will be discontinued. When- and Mr. and Mrs. and Mrs. Allison Burnham, Mr. and Winslow-VIead- e Circle, No 7, y.enz, Mr. G. ever there is a fifth Friday it will be Ladies Violins play and Mrs. Kuhn, Mr. and Mrs. Mrs. Ralston Burnham, Mrs. -

The Oxford Democrat : Vol. 65. No. 32
The Oxford Democrat. VOLUME 65. SOUTH PARIS. MAINE, TUESDAY, AUGUST 9, 1898. NUMBEK 32. almost as m wniuuL inure is few or do live nun in and in that INFLUENCE OF FOOD ON MILK. THE TYRANT OF THE HOUSE. exactly Anci this te the reason elected to succeed 1874, It vm Ion# eu|«posed thorniercane course a to vowel, hut Beeches" AMONG THE FARMERS. PEARL "OF THE PACIFIC. of syllable every «re lout in an ordinary eruption. One 18tfl be diod And gave place to Liliuoka- was proof against all blights, but of lato "The While in and tlie can walk to the end of the lani. a new a· it were, lute at- ▲ HRITI3II DAIRYMAN'S COXCLISIOKS.— baby deep* ordinary rapid pronunciation np advanced years worm, We cannot Jump or de not· or rin(, effect is the same as in German a little of it on an irun Now, the ul<l royal line expired a* tacked it at the and Hie chance* M precisely stream, gather root, PARIS HILL, ME., JiOXfc TOO MICH Bt'TTRR AUK.—COK- 1*1*7 jolly «niiHn or do « thin* us and an or ah-oo, is a mold of desired •foresaid with King Lot, and Kiru an.· that the will η η<>ύ··. The flour Sjwniah—that is, rod, press it into any now sugar planters AC. DKXSRP MILK rACTORIRS RE DUCK SIR- To nmki might creak Hawaii Is Richly Endowed With HANITARIU Uww«Be»ito»c« on ow. aa in "uow." without and this Bill and Kalakaua, though of ancient renew few free, T<je*«U_Y, ThtraUi ami practical acrtrutsurml topic· If we xhotiM walk. -

Fischer Seated, Measure Q Fails
Kiosk In This Issue Nov. 4 - 21, 2010 THE LEGEND OF SLEEPY HOLLOW MPC Storybook Theater Call for times Info: (831) 646-4213 • Fri., Nov. 5 Until 8 PM FIRST FRIDAY Pacific Grove Merchants Enter for a chance to win - Page 19 Brown Bag Promotion Friends for Life - Page 8 Neville in November - Page 10 Free & Open to the Public • Sat. Nov. 6 9 AM - 3 PM Winter Craft Fair PG Middle School Gym Benefits Robert H Down School PTA • Sat. Nov. 6 2:00 PM Pacific Grove Feast of Lanterns Annual General Meeting Chautauqua Hall, Central and 17th • Times Sat., Nov. 6 Nov. 5-12, 2010 Pacific Grove Community News Vol. III, Issue 7 10:00 AM - 2:00 PM Soul Collage Workshop w/ Cathy Bruno $55 (materials included) Artisana Gallery 309 Forest Ave (831) 655-9775 • Sun., Nov. 7 Surf’s 6:30 PM “Go With the Tide” A dramatic tutorial about Ed “Doc” Ricketts up — Performed by Howard Burnham at The Works 667 Lighthouse, PG 774 Wave Street, Monterey way 831-915-7523 $10 door • Tuesday, November 9 up 6:30 PM Velvet Coat; the Ragged Luck of A storm at sea Robert Louis Stevenson brought high waves Monterey Public Library to the coast this 625 Pacific Street, Monterey past week -- but no 831- 646-3949 storm. That may •www.monterey.org/llibrary yet happen, but for RSVP • Free now it has been • blue skies and Wed., Nov. 10 sunshine. 2pm - 7pm 2010 Monterey Bay Green Building Expo Photo by 831.633.WISE Vince Tuminello or www.buildingwise.net • Sat., Nov. -

1 Almira S. Burnham (1840-1932)
1 Almira S. Burnham (1840-1932) At the turn of the twentieth century, when the public reception of visual arts in Bloomington, Illinois could be characterized as “tepid,” or indeed, “positively cold,” and “comparatively few people … [knew] to what extent genuine and meritorious works of art” were produced in the city, there remained a commitment on the part of local artists—largely women—and the media to elevate the appreciation and patronage of painting to levels achieved by music and literature.1 One such artist, Almira S. Burnham (1840-1932) helped shape the figurative landscape for local working painters with her very own prolific and profitable, oil-painted landscapes and still lifes. Almira Sarah Ives was born on November 2, 1840 in Oswego, Kendall County, Illinois to parents Almon and Sarah (Ervin) Ives.2 Almon, Almira’s father, was born in Chautauqua County, New York and was one of the early settlers of Kendall County. He and his family moved to that county around 1834, where and when he engaged in farming.3 However, owing to ill health, Almon gave up farming and turned instead to a career in law. He was one of the first students to attend the Chicago Law School in 1847, and went on to make part of his living a real estate attorney.4 In June 1853, Almon, Sarah, and their nine children moved from Kendall County to Bloomington, where Almira resided for the rest of her life.5 Shortly after the family arrived, Almira’s mother, Sarah, died in 1854. In 1857, Almira’s father married Lucindia Barker.6 It is said, on the account of the early death of their mother, that Almira’s oldest sister Mary “became like a mother to her [eight] brothers and sisters.”7 Almon passed away in 1887 at the age of 72.8 Little else is known about Almira’s youthful experience in Bloomington prior to marrying Captain John H. -

University of Minnesota
University of Minnesota COMMENCEMENT CONVOCATION WINTER QUARTER 1939 NORTHROP :MEMORIAL AUDITORIUM Thursday, March 23, 1939, Eleven O'Clock PROGRAM PRESIDENT GUY STANTON FORD, Presiding PROCESSIONAL-Allegro Gothique - - Boellmann ARTHUR B. JENNINGS University Organist HYMN-HAmerica" My country! 'tis of thee, Our fathers' God! to Thee, Sweet land of liberty, Author of Liberty Of thee I sing; To Thee we sing; Land where our fathers died ! Long may our land be bright Land of the Pilgrims' pride With freedom's holy light; From every mountain side Protect us by Thy might Let freedom ring. Great God our King. COMMENCEMENT ADDRESS- HOn Educating Whole Men" DIXON RYAN Fox, Ph.D., LL.D., D.C.L., L.H.D., Litt.D. President, Union College, Schenectady, New York CONFERRING OF DEGREES GUY STANTON FORD, Ph.D., LL.D., Litt.D. President of the University 2 SONG-"Hail, Minnesota!" Minnesota, hail to thee! Like the stream that bends to sea, Hail to thee, our College dear! Like the pine that seeks the blue! Thy light shall ever be Minnesota, still for thee, A beacon bright and clear; Thy: sons are strong and true. Thy sons and daughters true From thy woods and waters fair, Will proclaim thee near and far; From thy prairies waving far They will guard thy fame At thy call they throng, And adore thy name; With their shout and song, Thou shalt be their Northern Star. Hailing thee their Northern Star. POSTLUDE-Toccata Boellmann ARTHUR B. JENNINGS University Organist SMOKING As a courtesy to those attending functions, and out of respect for the character of the building, be it resolved by the Board of Regents that there be printed in the programs of aU functions held in the Cyrus Northrop Memorial Auditorium a request that smoking be confined to the outer lobby on the main floor, to the gallery lobbies, and to the lounge rooms. -

Raising the Revolutionaries' Banner 1775-1776
Vol. 4 No. 3_____________________________________________ __July-August-September 2007 Raising the Revolutionaries’ Banner 1775-1776 19th century magic lanternslide depicting SC Patriot Sgt. William Jasper of the 2d South Carolina Continental Line, commanded by Col. William Moultrie, heroically re-raising the battered South Carolina standard over the parapet of the sand and palmetto log Fort Sullivan during the British naval bombardment of June 28-29, 1776. Mike Coker, the South Carolina Historical Society’s image expert, reports that this image is from a lanternslide painted by artists at the C. W. Briggs Company. The title on the slide is: “Sergeant Jasper at Ft. Moultrie, 1776”; it is a transparency, collodion on glass; size 3 1/4 X 4 inches. The Briggs were an American family of lanternists, slide painters and manufacturers. Daniel Briggs started painting and selling slides in 1850. Later the firm became C. (Caspear) W. Briggs and Co. in Philadelphia. Slides were made from stock negatives and colored by hand. (1850-1930s) This slide’s artist is unknown. Image is courtesy of the SCII Regiment. Artist Lucy Brown made a painting of this image in 1975, the original of which hangs in the main offices of the South Carolina Forestry Commission, 5500 Broad River Road, Columbia. In This Edition: Native Americans and the Southern Revolution, Part II: Independence and the 1776 Cherokee War………......………21 Editor / Publisher’s Notes………………………....……….…2 Insubordination of Captain Polk’s Rangers During the Upcoming SCAR events……………………..……....3, 4 and 7 Summer of 1775….……………………….….………………....28 Southern Revolutionary War Institute…………………..…12 Subjects of the Crown “The Queen’s own Loyal Virginia Letters to the Editor…………………………….…..………..11 Regiment and Dunmore’s Ethiopian Regiment, 1775- Calendar of Upcoming Events………………….….…..……15 1776”……………………………..……………………………...34 “Under the Crown” Living History Event………………….19 1 Editor’s Notes flavor. -

Burnham Wood Charter School
DISTRICT 1 Receipt bynA: ______ Dale ofCommittee tlcvic:w: Dale ofSBOE RC'View: ------ _ Approved _ NOI Approved Beginning Dale ofOpcruion: Application for Approval of an Open-Enrollment Charter APPUCAnON [1Um.ctfO...: SIIb",;t four copi". 01 corrrplft~ app/icario" witlt 1M propouti dIarr.,. and tWUTancu 'igrwl by 1M Chief OperaIing OjfiCD' 01tM School and 1M evidnrt:. 01pcrtmllco_ry SIlppOr/ 101M T...... Edu&aIion Agmcy. Doc-JJI1t!nI COnl7'Ol C'nI~. [70/tHor/it Congr= Aw.. AILftirr, T= 7870/. For =Ul~'. C1Jnlaa 1M Ojfice 01 Chaner Schools at (512) 463-9575. Chief Operoing Officer of~Charter: Iris Burnham Name ofSponsoring Entity: El Paso Education Initiative, Inc. The applic:mt is an ·eligible entity~ under the following categoty (cheel< one): __ an institution oflrigher education (TEC 61.003); _X_ a tax-<:xempt org:miz.ation [501(cXJ)]; __ a priv3tofindependcnt institution oflrigher edu=:ion (TEe 61.003); __ a govemrnenl.ll entity, S~rA~~: 7310 Bishop Flores City: El Paso Zip: 79912 Phone Number: ( 9 1 5) 584 - 9499 FAX:(915) 585-8814 Name ofProp<lSed Charter: Burnham I'lood Charter Schools Charter Site Address:731 0 Bishop Flores City: El Paso Zip:7 991 2 PhoneNumber: (915) 584-9499 FAX: (915) 585-8814 ~~~~~~~~~ Gr.lde Expec-.ed Initial Projected Max. Leve!s:K------ 1 2 Enrollment: __1_4_0____ Enrollment: __1~3_0_0__________ The chaner will primarily serve an area tb.at is geographically: ~ urllan __X_ sub",'::an rural In succinct t=s describe the proposed school inclwling grade levels offered. stUdent populations served, educational focus and any other essential c:u.rac-.eristics. -
Alumni Register
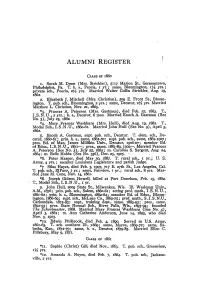
ALUMNI REGISTER CLASS OF 1860 I. Sarah M. Dunn (Mrs. Strickler), 5117 Marion St., Germantown, Philadelphia, Pa. T. h. s., Peoria, I yr.; same, Bloomington, I~ yrs.; private sch., Peoria, 2~ yrs. Married Walter Coffin Strickler, Aug. 19, 1862. 2. Elizabeth J. Mitchell (Mrs.. Christian), 509 E. Front St., Bloom ington. T. pub. sch., Bloomington, 2 yrs.; same, Decatur, 2~ yl·s. Married Matthew L. Christian. Nov. 21, 1865. *3. Frances A. Peterson (Mrs. Gastman), died Feb. 27, 1863. T., 1. S. N . U., 2 yrs.; h. 5., Decatur, 6 mos. Married Enoch A. Gastman (See NO.5), July 25, 1862. *4- Mary. Frances Washburn (Mrs. Hull), died Aug. 19, 1882. T., Model Sch., LS.N.U., 1860-61. Married John Hull (See NO.9), April 3, 1862. 5. Enoch A. Gastman, supt pub. sch., Decatur. T. elem. sch., De catur, 1860-61'; prin. h. s., same, 1862-70; supt. pub. sch., same, 1862-1907; pres. Bd. of Man. James Millikin Univ., Decatur, 1906-07; member Bd. of Educ., 1. S. N . U., 1871-; pres., same, 1881-8g, 1902-. -Married Frances A. Peterson (See NO.3), July 25, 1862; m. Caroline S. Sargent, Aug. 24. 1864; m. Belle Hobbs (See No. 356), Dec. 25, 1905. *6. Peter Harper, died May 30, 1887. T. rural sch., I yr.; U. S. Army, 4 yrs.; member Louisiana Legislature and parish ju51ge. *7 Silas Hayes, died Feb. 3, 1907, 717 E. 27th St., Los Angeles, Cal. T. pub. sch., EIPaso, 1 yr.; same, Fairview, I yr.; rural sch., 8 yrs. Mar ried Jane M.