Community Health Needs Assessment (CHNA) Conducted Collaboratively by Deaconess Health System, St
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Craig R. Ehlen 10929 Driver Drive Evansville, Indiana 47725
Craig R. Ehlen 10929 Driver Drive Evansville, Indiana 47725 812/867-6164 (Home) 812/464-1785 (Office) 812/465-1044 (Fax) [email protected] Education: Doctor of Business Administration (DBA) — Southern Illinois University at Carbondale (1994) Dissertation title: “An empirical examination of the fairness of AICPA- mandated peer and quality review decision-making procedures and their effects on reviewees’ attitudes toward the AICPA and the reviewer” Master of Accounting Science (MAS) — University of Illinois at Urbana-Champaign (1969) Bachelor of Science in Accountancy (BS) — University of Illinois at Urbana-Champaign (1968) Professional Certifications: Chartered Global Management Accountant — Indiana (2012) Certified Fraud Examiner (CFE) — Indiana (1997) Certified Public Accountant (CPA) — Illinois (1968) Affiliations: American Accounting Association American Institute of Certified Public Accountants Association of Certified Fraud Examiners Indiana CPA Society University of Illinois Alumni Association Major Awards and Honors: Indiana CPA Society “Outstanding Educator” Award (2001) USI College of Business “Excellence in Research” Award (2006, 2003, and 1999) USI College of Business Student Learning and Teaching Innovation Fellowship (2006) USI College of Business R. Malcolm Koch Research Fellowship (1998) Indiana CPA Educational Foundation Doctoral Loan/Grant (1994/1995) AICPA Doctoral Fellow (1991/1992 and 1990/1991) Bronze Tablet Scholar — University of Illinois (1968) 1 Teaching Experience: 2002 — present: Professor of Accounting Department -

History of Warrick and Its Prominent People : from the Earliest Time to The
Class _L5J3l2^^ Copyright N^ COPYRIGHT DEPOSIT. HISTORY i>T O F W A R R I C K AND ITS PROMINENT PEOPLE From the Earliest Time to the Present; Together with Interesting- Biographical Sketches, Reminiscences, Notes, Etc. '^Uvo-v-. LLUSTRATED NINETEEN HUNDRED AND NINE CRESCENT PUBLICATION COMPANY '^9 1 B o o n \ i 1 e , Indiana b V \H^ ^ TO T TI A T () X E Whose encouragenienl aiul aid resulted in this work THIS V O L U iM E is (iratefullv Dech'iated. LIBRARY of CONGRESS Two COBies Received MAY 17 1909 Copyriunt tntry g COPYRIGHT 1909 NO CLASS A[ ^ XXc. BY MONTE M. KATTERJOHf PREFACE. Tliis volume is doubtless one with many faults, for no history extant is free from errors. Great care was taken in preparing the matter found herein, and all discrepancies were eradicated. I n- just criticism cannot rectify the errors that are sure to apjiear, and the author feels assured that all thoughtful jjeople will recognize and a])preciate the undertaking, also realize that a i)ublic benefit has been accomplished. The biographical sectioii is devoted to the record of men, living and dead. If it is incomplete, the fault cannot be justly attributed to the author. Many people were solicited, but on mone- tary grounds refused to support the publication. Those who read this book, and who know what constitutes a true history, will agree with the author that this volume is sujierior to any ever published in this county, inasmuch as its fine illustra- tions are a single history within themselves. -

Morris Birkbeck's Estimate of the People of Princeton in 1817
Morris Birkbeck’s Estimate of the People of Princeton in 1817 By LUCIUSC. EMBREE. A paper read at the meeting of the Southwestern Indiana Historical Society, May 27, 1925, at Newburg. It is a matter challenging the notice of the people of south- western Indiana, and especially of those of them who are descended from the pioneers of the early years of the nine- teenth century, that, on the part of the biographers of Abra- ham Lincoln, apparently very little effort has been made to ascertain the degree that the development of his nature and character was infiuenced by his environment, and associa- tions, during the fourteen years that he spent as a boy and young man in Spencer County and the surrounding localities. The attitude seems to have been that Lincoln’s contacts and associations during this period were negligible, and the im- pression conveyed by some of them is that the people of south- western Indiana, at that day, were ignorant, uncouth and lawless. In view of this attitude, and of the impression which it engenders in the minds of the readers of these productions, it behooves the good peop!e of the locality in question, and those of them especially who are the descendants of the pioneers, to take up arms in defense of the character and qualities of those who have gone before them. Persistence in ignoring, and misrepresenting, the people with whom the boy Lincoln came in contact in his early years, while he was growing from child- hood to man’s estate in this region, and in conveying the im- pression that these people were ignorant, uncouth and lawless, not only becomes tiresome, but demonstrates that those who have assumed to portray the life of Lincoln, and to define the process by which he became the man he was, have been want- ing in industry, and have neglected one of the most promising fields of inquiry. -

Gibson County LRTP
LONG RANGE TRANSPORTATION PLAN Gibson County, Indiana Prepared by the Evansville Metropolitan Planning Organization LONG RANGE TRANSPORTATION PLAN Gibson County, Indiana ACKNOWLEDGEMENTS GIBSON COUNTY BOARD OF COMMISSIONERS Bob Townsend, President Gerald Bledsoe, Vice-President Alan Douglas, Member CITY OF PRINCETON UMBRELLA COMMITTEE Bob Hurst, Mayor Kelly Dillon, Toyota Motor Manufacturing Indiana Tim Burris, Hansen Corporation Peg Michas, Pride in Princeton Alan Douglas, Gibson County Commissioner Jason Spindler Kathy Cowling, Princeton Councilwoman Jami Allen, Fifth Third Bank Lynn Roach, WRAY Radio Gary Blackburn, Princeton Publishing Chris Hayes, Princeton Retail Merchants Helen Hauke Todd Mosby, Gibson County Economic Development Corporation Karen Thompson, Gibson County Chamber of Commerce Bob Shaw EVANSVILLE METROPOLITAN PLANNING ORGANIZATION Mr. Bradley G. Mills, Executive Director Mr. Vishu Lingala, Transportation Planner Mr. Craig Luebke, Transportation Planner Ms. Erin Mattingly, Transportation Planner TABLE OF CONTENTS CHAPTER 1: INTRODUCTION.......................................................................................... 1 A. Study Background ........................................................................................................................................... 1 B. Gibson County Transportation Planning Area ............................................................................................... 1 C. Plan Purpose ................................................................................................................................................... -
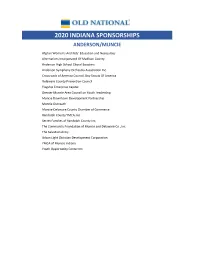
2020 Sponsorship Website Template.Xlsx
2020 INDIANA SPONSORSHIPS ANDERSON/MUNCIE Afghan Women's And Kids' Education and Necessities Alternatives Incorporated Of Madison County Anderson High School Choral Boosters Anderson Symphony Orchestra Association Inc. Crossroads of America Council, Boy Scouts Of America Delaware County Prevention Council Flagship Enterprise Capital Greater Muncie Area Council on Youth Leadership Muncie Downtown Development Partnership Muncie Outreach Muncie‐Delaware County Chamber of Commerce Randolph County YMCA, Inc. Secret Families of Randolph County Inc. The Community Foundation of Muncie and Delaware Co., Inc. The Salvation Army Urban Light Christian Development Corporation YMCA of Muncie Indiana Youth Opportunity Center Inc. BLOOMINGTON Amethyst House Inc. Bedford Clothe A Child Inc. Big Brothers Big Sisters of South Central Indiana Bloomington Health Foundation Bloomington PRIDE Boys and Girls Clubs of Bloomington Boys and Girls Club of Lawrence County Cardinal Stage Company Catholic Charities City of Bloomington Dr. Martin Luther King Jr. Birthday Celebration Commission Community Foundation of Bloomington and Monroe County Dimension Mill Inc. Dr Martin Luther King Commission City of Bloomington Ellettsville Chamber of Commerce Fairview Elementary School Foundation of Monroe County Community Schools Inc. Greater Bloomington Chamber of Commerce, Inc. Habitat for Humanity of Monroe County Indiana Hannah Center Inc. Hoosier Hills Food Bank Inc. Ivy Tech Foundation Kiwanis Club of South Central Indiana Lotus Education And Arts Foundation Inc. Monroe County Community School Corporation Monroe County YMCA Pantry 279 Inc. People and Animal Learning Services Inc. Radius Indiana Inc. Shalom Community Center Inc. Southern Indiana Exchange Clubs Foundation Inc. The Salvation Army of Monroe County United Way of Monroe County Indiana United Way of South Central IN/Lawrence County Wonderlab‐Museum Of Science Health and Technology Inc. -

Boonville Shopping Center
OFFERING MEMORANDUM BOONVILLE SHOPPING CENTER 802 W. MAIN ST | BOONVILLE, IN 47601 ™ LISTED BY CHUCK EVANS SENIOR ASSOCIATE DIRECT (310) 919-5841 MOBILE (925) 323-2263 [email protected] LIC # 01963473 (CA) BROKER OF RECORD KYLE MATTHEWS LIC # RC51700140 (IN) BOONVILLE SHOPPING CENTER OFFERING MEMORANDUM BOONVILLE SHOPPING CENTER 802 W. MAIN ST | BOONVILLE, IN 47601 04 | EXECUTIVE OVERVIEW 06 | PROPERTY OVERVIEW 10 | FINANCIAL OVERVIEW 14 | AREA OVERVIEW 3 SECTION I EXECUTIVE OVERVIEW 4 BOONVILLE SHOPPING CENTER INVESTMENT HIGHLIGHTS SALE PRICE: » Recently Extended Lease – Autozone just executed a lease $760,197.83 renewal until 2031 demonstrating a strong commitment to the site » Longevity of tenants – Most of the tenants in the shopping center have been there for the past 15 years » High Returns – True capitalization on an above market yield CAP RATE: 12.00% » Ideal placement – located on the main road from the city to the Walmart Supercenter which is the main shopping hub for the town » 19,000+ Vehicles per day » Capital Improvements: NOI: • Resurfaced and re-striped parking lot • The parking lot was cleaned, milled, and 350 tons of new asphalt $93,090.82 were laid on the parking lot. • 30% of roof was resurfaced with elastomeric coating • All parking lot and canopy lights replaced with LED lights and Four LED solar powered lights were installed as well. • In total, $86,000 were invested to improve the center in preparation for a sale. 5 SECTION II PROPERTY OVERVIEW 6 BOONVILLE SHOPPING CENTER PARCEL MAP PHYSICAL DESCRIPTION -

I LOVE, Ycqmmunitv SERVICE
If you have issues viewing or accessing this file contact us at NCJRS.gov. \ THE I LOVE,yCQMMUNITV SERVICE I COOKBOOK Easy-to-do recipes for community service that combine service-learning with Youth as Resources projects. This publication is made possible by the National Crime Prevention Council, the Indiana Department of Education, Youth Resources of Southwestern Indiana, the Evansville Courier Company, and Krieger-Ragsdale & Company. First Printing April,1994 Second Printing October, 1994 COPYRIGHT ©1994 YOUTH RESOURCES OF SOUTHWESTERN IN "Helping others really gave me a warm feeling. It really opened my eyes to the poverty that's right around me. It's not just in New York and L.A. - it's here in Evansville. Aislln Arney Harrison High School History Class Project with Christian Life Center () () "One thing I'm going to do differently because of the Helping Hands project is to help people Who are in need, and not look down on them." Jamie Benefiel, Harrison High School Ii "It [the project] made me feel happy. I helped someone." o Jamila, Caze Elementary School First Aid From ttl'e First Grade "The hardest part was doing the work after school, but the best part was going to the day care center to work with the kids. It made me feel good." 8th Grader, McGary Middle School "I got a lot of pleasure watching how well my Exploring Childhood students worked with children. We were all touched by the hugs and 'I love yo us' when we left each place. I was"troubled to learn of the number of hours some children spend away from their families. -

Download Download
Faulting in Posey and Gibson Counties, Indiana Curtis H. Ault, Dan M. Sullivan, and George F. Tanner Indiana Geological Survey, Bloomington, Indiana 47405 Introduction and History of Study In the fall of 1977 we began our investigation of the Wabash Valley Fault System to help characterize the tectonic processes in southwestern Indiana. It was part of a project funded by the Nuclear Regulatory Commission for geologists and geophysicists from various universities and geological surveys to study the tectonics, seismicity, and structure of the area within a 200-mile radius of New Madrid, Missouri. Since the early 1900's more than 6,000 petroleum test wells and other tests have been drilled in Posey County and southern Gibson County, which contain nearly all known faults of the Wabash Valley Fault System in Indiana. Detailed subsurface structural mapping by petroleum companies was conducted from the 1930's and 1940's until the late 1960's, when oil activity declined. But these studies have been proprietary, and the companies have released little or no structural data. Further, oil companies have usually focused attention on the reservoir rocks near the faults rather than on the complexity of the faults themselves. Part of the Ridgway Fault of the Wabash Valley Fault System in Illinois was early described by Cady in 1919 (4). As drilling for petroleum and mining for coal progressed in Illinois, the fault system was further defined in county reports and maps and other fault studies (Stonehouse and Wilson (11) for example). The most recent mapping of the faults in Illinois was completed by Bristol and Treworgy in 1979 (2). -

Posey County Comprehensive Plan.Indd
POSEY COUNTY FOR UNINCORPORATED POSEY COUNTY, POSEYVILLE, AND CYNTHIANA Final Comprehensive Plan Bernardin Lochmueller & Associates, Inc. Posey County Comprehensive Plan for unincorporated Posey County, Poseyville and Cynthiana Final Prepared for: Posey County Coliseum Building 126 East Third Street, Mount Vernon, Indiana 47620 Phone: (812) 838-1311 Prepared by: Bernardin, Lochmueller and Associates, Inc. Engineering, Planning, Surveying, Environmental Studies, Water/Wastewater 6200 Vogel Road, Evansville, Indiana 47715 Phone: (812) 479-6200 Draft Final Plan published: October 31, 2008 Posey County Area Plan Commission public hearing and plan adoption: November 13, 2008 Posey County Board of Commissioners plan adoption: November 18, 2008 Poseyville Town Council plan adoption: Cynthiana Town Council plan adoption: 11/13/2008 City of Mount Vernon Comprehensive Plan OUTLINE & Posey County Comprehensive Plan (Unincorporated Posey County, Poseyville & Cynthiana) A. Purpose of Public Hearing B. Planning Process Public Hearing C. Comprehensive Plan Benefits Posey CtCounty Area Plan Comm iiission Hovey House D. Comprehensive Plan Contents Fourth at Walnut Mount Vernon, Indiana 47620 E. Community Profile F. Future Vision November 13, 2008 at 6:00 PM G. Recommendations H. Next Steps A. Purpose of Public Hearing B. Planning Process 1. Receive public comment on two draft comprehensive plans: 1. Four meetings with Mount Vernon and Posey County Steering • Mount Vernon Committees over past 7 months • Posey County –> unincorporated Posey County and incorporated Poseyville and • Identify issues and leaders to be interviewed , and prepare survey (5/07 & 13/2008) Cynthiana • Develop future vision (7/15/2008) 2. Public hearing fulfills two purposes: • Develop future alternatives (9/20/2008) • Meets State statutory requirements for adoption of a new comprehensive plan • Develop recommendations (10/15/2008) • Fulfills Indiana Office of Community and Rural Affairs grant requirements for the separate grants funding each plan 2. -

Action News the Official Publication of the Southwestern Indiana Builders Association 2175 N
Action News The Official Publication of the Southwestern Indiana Builders Association 2175 N. Cullen Ave. Evansville, IN 47715 812-479-6026 www.SIBAonline.org February 2016 Upcoming Events IBA Legislative Conference February 1st SIBA Board Meeting February 9th Membership Meeting February 9th Page 6 Lunch and Codes February 17th 2016 SIBA President, Brian Murphy, (left) presents 2015 SIBA Spring Tour of Homes President, Aaron Miller, with a plaque of recognition. Miller March 5-6 wished Murphy all the best as 2016 President. Page 13 Spring Tour of Homes! March 5-6, Noon-4pm more on page 13 TOUR OF Advertise with HOMES the Parade! pages 18-19 “All you need is love. But a little chocolate now and then doesn’t hurt” Charles M. Schulz Providing Safe, Affordable Housing Since 1948 Page 2 FEBRUARY 2016 EDITION ACTION NEWS ACTION NEWS is the Official Publication of the Southwestern Indiana Builders Association Advertising Information available upon request. 2016 COMMITTEE CHAIRS SIBA STAFF SIBA REMODELERS EXECUTIVE DIRECTOR Bill Pedtke PARADE OF HOMES E-mail: [email protected] Matt Reinbrecht, Reinbrecht Homes Michelle Ferrero, Ferguson EVENTS COORDINATOR FALL TOUR OF HOMES Jamie A. Elliott Bill Kattmann, Kattmann Construction, Inc. E-mail: [email protected] SPRING TOUR OF HOMES Bill Kattmann, Kattmann Construction, Inc ACTION NEWS GOLF OUTING 2016 DEADLINES EXECUTIVE OFFICES Danny Davis, Davis Homes 2175 N. Cullen Avenue CODES Issue Deadline Evansville, Indiana 47715 Ron Dauby, Dauby Construction, Inc. February January 15 Phone: 812-479-6026 POLITICAL ACTION March February 12 Fax: 812-479-6340 Carl Shepherd, Shepherd Construction April March 18 Office Hours: May April 15 SCHOLARSHIP 8:30 a.m. -

Community Health Improvement Plan 2019-2021
COMMUNITY HEALTH IMPROVEMENT PLAN 2019-2021 Vanderburgh County Health Department TABLE OF CONTENTS Table of Contents Health Officer Vision .............................................................................................................................. 1 The Priorities ........................................................................................................................................... 2 Mental Health ........................................................................................................................................ 3 Substance Abuse ................................................................................................................................... 4 Food Insecurity ..................................................................................................................................... 5 Infant Mortality ..................................................................................................................................... 6 Input ......................................................................................................................................................... 7 Methods ................................................................................................................................................. 7 Community Partner Recommendations ................................................................................................ 7 Governing Entity/Policy Influencer Recommendations ...................................................................... -
![[ZIP] Dear Community State Bank of Southwestern Indiana Customer](https://docslib.b-cdn.net/cover/8840/zip-dear-community-state-bank-of-southwestern-indiana-customer-3988840.webp)
[ZIP] Dear Community State Bank of Southwestern Indiana Customer
[Date] [Name] [Address] [City], [State] [ZIP] Dear Community State Bank of Southwestern Indiana Customer: Earlier this year, Crane Credit Union (“Crane”), a community-chartered credit union located in Odon, Indiana, entered into an agreement to purchase all assets and assume certain liabilities (the “Transaction”) of Community State Bank of Southwestern Indiana (“CSBSWIN”). The purchase is expected to be effective on November 30, 2020, pending receipt of final regulatory approvals. It is with great excitement that we at Crane welcome you as a new member of Crane following completion of the Transaction. Upon completion of the Transaction, Crane will purchase and assume all of CSBSWIN’s loans and deposits and all bank accounts held by CSBSWIN will be transferred to Crane. Upon the completion of the Transaction, Crane’s Charter will be amended to include former CSBSWIN customers. Crane currently has a community field of membership that encompasses Central and Southern Indiana. Crane’s field of membership will be expanded, subject to regulatory approval, to serve persons who reside or work within Spencer County in Indiana, Henderson County in Kentucky and Clark County in Illinois. If, however, any CSBSWIN deposit customers do not qualify for membership, Crane holds a low-income designation from the National Credit Union Administration (the “NCUA”) that will allow Crane to hold non-member deposits. Thus, it is expected that all CSBSWIN customers will qualify as and become members of Crane and all deposits with CSBSWIN assumed by Crane will be insured by the NCUA (described further below). As a requirement of credit union membership, for any new member that does not have a savings account, Crane will open and fund a non-transaction share account with a balance of $5.00 for each such customer.