National Leprosy Eradication Program Guidelines for Primary, Secondary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
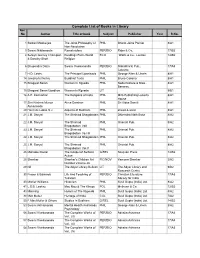
Complete List of Books in Library Acc No Author Title of Book Subject Publisher Year R.No
Complete List of Books in Library Acc No Author Title of book Subject Publisher Year R.No. 1 Satkari Mookerjee The Jaina Philosophy of PHIL Bharat Jaina Parisat 8/A1 Non-Absolutism 3 Swami Nikilananda Ramakrishna PER/BIO Rider & Co. 17/B2 4 Selwyn Gurney Champion Readings From World ECO `Watts & Co., London 14/B2 & Dorothy Short Religion 6 Bhupendra Datta Swami Vivekananda PER/BIO Nababharat Pub., 17/A3 Calcutta 7 H.D. Lewis The Principal Upanisads PHIL George Allen & Unwin 8/A1 14 Jawaherlal Nehru Buddhist Texts PHIL Bruno Cassirer 8/A1 15 Bhagwat Saran Women In Rgveda PHIL Nada Kishore & Bros., 8/A1 Benares. 15 Bhagwat Saran Upadhya Women in Rgveda LIT 9/B1 16 A.P. Karmarkar The Religions of India PHIL Mira Publishing Lonavla 8/A1 House 17 Shri Krishna Menon Atma-Darshan PHIL Sri Vidya Samiti 8/A1 Atmananda 20 Henri de Lubac S.J. Aspects of Budhism PHIL sheed & ward 8/A1 21 J.M. Sanyal The Shrimad Bhagabatam PHIL Dhirendra Nath Bose 8/A2 22 J.M. Sanyal The Shrimad PHIL Oriental Pub. 8/A2 Bhagabatam VolI 23 J.M. Sanyal The Shrimad PHIL Oriental Pub. 8/A2 Bhagabatam Vo.l III 24 J.M. Sanyal The Shrimad Bhagabatam PHIL Oriental Pub. 8/A2 25 J.M. Sanyal The Shrimad PHIL Oriental Pub. 8/A2 Bhagabatam Vol.V 26 Mahadev Desai The Gospel of Selfless G/REL Navijvan Press 14/B2 Action 28 Shankar Shankar's Children Art FIC/NOV Yamuna Shankar 2/A2 Number Volume 28 29 Nil The Adyar Library Bulletin LIT The Adyar Library and 9/B2 Research Centre 30 Fraser & Edwards Life And Teaching of PER/BIO Christian Literature 17/A3 Tukaram Society for India 40 Monier Williams Hinduism PHIL Susil Gupta (India) Ltd. -

Constituent Assembly Debates
Thursday, 17th November, 1949 14-11-1949 Volume XI to 26-11-1949 CONSTITUENT ASSEMBLY DEBATES OFFICIAL REPORT REPRINTED BY LOK SABHA SECRETARIAT, NEW DELHI SIXTH REPRINT 2014 Printed at JAINCO ART INDIA, New Delhi. THE CONSTITUENT ASSEMBLY OF INDIA President: THE HONOURABLE DR. RAJENDRA PRASAD. Vice-President: DR. H.C. MOOKHERJEE. Constitutional Adviser: SIR B.N. RAU, C.I.E. Secretary: SHRI H.V.R. IENGAR, C.I.E., I.C.S. Joint Secretary: MR. S.N. MUKHERJEE. Deputy Secretary: SHRI JUGAL KISHORE KHANNA. Marshal: SUBEDAR MAJOR HARBANS LAL JAIDKA. CONTENTS Volume XI—14th to 26th November 1949 PAGES PAGES Monday, 14th November 1949— Monday, 21st November 1949— Draft Constitution—(Contd.) .............. 459—502 Draft Constitution—(Contd.) ............. 721—772 (Amendment of articles) Tuesday, 22nd November 1949— Tuesday, 15th November 1949— Draft Constitution—(Contd.) ............. 773—820 Draft Constitution—(Contd.) .............. 503—556 Wednesday, 23rd November 1949— [Amendments of Articles—(Contd.)] Draft Constitution—(Contd.) ............. 821—870 Thursday, 24th November 1949— Wednesday, 16th November 1949— Taking the Pledge and Signing Draft Constitution—(Contd.) .............. 557—606 the Register ..................................... 871 [Amendment of Articles—(Contd.)] Draft Constitution—(Contd.) ............. 871—922 Thursday, 17th November 1949— Friday, 25th November 1949— Draft Constitution—(Contd.) .............. 607—638 Government of India Act [Third Reading] (Amendment) Bill ........................... 923—938 Friday, 18th November 1949— Draft Constitution—(Contd.) ............. 938—981 Draft Constitution—(Contd.) .............. 639—688 Saturday, 26th November 1949— Saturday, 19th November 1949— Announcement re States .................... 983 Draft Constitution—(Contd.) .............. 689—720 Draft Constitution—(Contd.) ............. 983—996 DRAFT CONSTITUTION 607 CONSTITUENT ASSEMBLY OF INDIA Thursday, the 17th November 1949 ———— The Constituent Assembly of India met in the Constitution Hall, New Delhi, at Ten of the Clock, Mr. -

S NO PRODUCT CODE Accountname 1 CD PS
S NO PRODUCT AccountName Address CODE 1 CD P.S. MAUNI HOUSE NO 257 CHEENA KHAN LINE TLT. 2 CD MAHILA UTTHAN GRAMODYOG SANSTH CHANDRA NIWAS P.O MLT. 3 CD KUMAR JITENDRA 18 BARUM VILLA SHER KA DANDA 4 CD SAMEER CONSTRUCTION NTL. 5 CD PRITHVI RATAN GRAMODYOG SANSTH CHAUKRI TEHSIL- DIDIHAT 6 CD HEMLATA JOSHI BHOWALI NIWAS KAILAKHAN TLT. 7 CD SHARDOTSAVA SAMITI C/O NAGAR PALIKA 8 CD HINA TRAVELS MALL ROAD 9 CD RIFFLE CLUB NTL. 10 CD STAFF SECUTITIES FORFEITURE A/ SEVEN OAKS MLT. 11 CD SUNDRY DEPOSIT NAINITAL BANK LTD. SEVEN OAKS MALLITAL 12 CD KISHAN SINGH BISHT NTL. MALLITAL NAINITAL 13 CD HOTEL AMBASSADOR THE MALL 14 SB J.C JOSHI B.V.M 15 SB BANWARI LAL TANDON LUCKNOW 16 SB MANI RAM GOVT. HOUSE 17 SB SUBODH KUMAR NAINITAL 18 SB PADMA DATT TRIPATHI NAINITAL 19 SB DISTT. BEE KEEPING ASSOCIATION NAINITAL 20 SB HEERA BALLABH PATHAK M.E.S STORES 21 SB MADAN MOHAN LAL C/O S.P SAXENA DEUTY COMM 22 SB P.S MEHTA MEHRA NIWAS 23 SB HEMA SAH NAINITAL 24 SB PARMANAND KANDPAL NAINITAL 25 SB HARISH CHANDRA BHATT NAINITAL 26 SB BRIJ MOHAN PANT DURGA PUR 27 SB KRISHAN LAL SAH S/O B.D.SAH LALA BAZAR ALMORA 28 SB S.D. SINGH B.V.M NAINITAL 29 SB G.I.C. COOPERATIVE SOCIETY NAINITAL 30 SB SOBAN SINGH NAINITAL 31 SB NARAIN SWAMI HIGHER SECONDARY SCHOOL RAMGAR 32 SB COOPRETIVE SOCIETY GETHIA GETHIA 33 SB CIVIL ESRVICE CLUB NAINITAL 34 SB J.P. -

RACHAIAH, SHRI B. : B.Sc., BL; Congress (Karnataka)
R RACHAIAH, SHRI B. : B.Sc., B.L.; Congress (Karnataka); s. of Shri Basavaiah; b. August 10, 1922; m. Shrimati Goramma, 2 s. and 5 d.; Member, Karnataka Legislative Assembly, 1952-70; Minister, Government of Mysore, 1962-70; Member, Rajya Sabha, 3-4-1974 to 21-3-1977; Died. Obit. on 23-2-2000. RADHAKRISHNA, SHRI PUTTAPAGA : M.A., LL.B.; T.D.P. (Andhra Pradesh); s. of Shri Puttapaga Buddaiah; b. February 13, 1944; m. Shrimati P. Karunamani, 2 s. and 2 d.; Member, Rajya Sabha, 10-4-1984 to 9-4-1990. Per. Add. : H. No. 2-2-1/5, Opp. Collector’s Office, Mahabubnagar (Andhra Pradesh). RAFIQUE ALAM, SHRI : M.A., LL.B.; Congress (I) (Bihar); s. of Md. Khalilur Rahman; b. June 1, 1929; m. Shrimati Alam Ara, 5 s. and 4 d.; Member, Bihar Vidhan Sabha, 1962-67 and 1969-80; Minister, Government of Bihar; Chairman, Estimates Committee, Bihar Legislative Assembly, 1969-70; Member, Rajya Sabha, 3-4-1982 to 2-4-1988 and 3-4-1988 to 2-4-1994; Chairman, Committee on Petitions, Rajya Sabha, 1986-88; Union Deputy Minister/Minister of State holding portfolios of Petroleum and Natural Gas, Textiles and Health and Family Welfare , February, 1988 to November , 1 9 8 9 ; President, Bihar P.C.C. (I), 1980-83; Recipient of National Integration Award, 1988. Per. Add. : Village Gauramani, Post Office Gangi Hat, via KishanGanj, Purnea District (Bihar). RAGHAVAN, SHRI V. V. : Matriculation; C.P.I. (Kerala); s. of Shri Velappan; b. June 23, 1923; m. Shrimati Sathya Bhama, 1 s. -

Languages of the World--Indo-Pacific Fascicle Eight
REPORT RESUMES ED 010 367 48 LANGUAGES OF THE WORLD--INDO-PACIFIC FASCICLE EIGHT. ST- VOEGELI1, C.F. VOEGELIN, FLORENCE M. INDIANA UNIV., BLOOMINGTON REPORT NUMBER NDEA- VI -63 -20 PUB DATE. APR 66 CONTRACT OEC-SAE-9480 FURS PRICE MF-$Q.18HC-52.80 70P. ANTHROPOLOGICAL LINGUISTICS, 8(4)/1-64, APRIL 1966 DESCRIPTORS- *LANGUAGES, *INDO PACIFIC LANGUAGES, ARCHIVES OF LANGUAGES OF THE WORLD, BLOOMINGTON, INDIANA THIS REPORT DESCRIBES SOME OF THE LANGUAGES AND LANGUAGE FAMILIES OF THE SOUTH AND SOUTHEAST ASIA REGIONS OF THE INDO-PACIFIC AREA. THE LANGUAGE FAMILIES DISCUSSED WERE JAKUM, SAKAI, SEMANG, PALAUNG-WA (SALWEEN), MUNDA, AND DRAVIDIAN. OTHER LANGUAGES DISCUSSED WERE ANDAMANESE, N/COBAnESE, KHASI, NAHALI, AND BCRUSHASKI. (THE REPORT IS PART OF A SERIES, ED 010 350 TO ED 010 367.) (JK) +.0 U. S. DEPARTMENT OF HEALTH, EDUCATION AND WELFARE b D Office of Education tr's This document has been reproduced exactlyas received from the S.,4E" L es, C=4.) person or organiz3t1on originating It. Points of view or opinions T--I stated do not nocessart- represent official °dice of Edumdion poeWon or policy. AnthropologicalLinguistics Volume 8 Number 4 April 116 6 LANGUAGES OF THE WORLD: INDO- PACIFIC FASCICLE EIGHT A Publication of the ARCHIVES OFLANGUAGES OF THEWORLD Anthropology Department Indiana University ANTHROPOLOGICAL LINGUISTICS is designed primarily, but not exclusively, for the immediate publication of data-oriented papers for which attestation is available in the form oftape recordings on deposit in the Archives of Languages of the World. -

Surveyed During the Tenure of This Project
Endangered Archives Programme British Library, UK A Report on the Pilot Project Entitled “Private Records of Some Leading Business Families of Early Colonial Bengal” (EAP 906) By EAP: 906 Research Team Dr. Tridibsantapa Kundu, Principal Investigator Dr. Sudip Chakraborty, Joint Investigator Ayan Kundu, Research Assistant Krishnapriya Chakravarti, Research Assistant Report of EAP 906 Acknowledgement For implementation of this Pilot Project we received support and encouragement from many people and institutions. We would like to thank Professor Anuradha Ray of Jadavpur University for her deep concern about this project. Similarly Professor Sudeshna Banerjee also provided useful suggestions for implementation of the project. Professor Chittabrata Palit shared his vast knowledge on the business families of colonial Bengal which benefited us tremendously. We would like to thank all the members of the families we surveyed during the tenure of this project. Special thanks to the members of Endangered Archives Programme (EAP) for supporting this project which provided us with an excellent opportunity to carry out this challenging survey. We would like to convey our heartfelt thanks to the authorities of Centre for Studies in Social Sciences (Kolkata), the archival partner of this project for their invaluable guidance and cooperation. Special thanks to Mr. Abhijit Bhattacharya and his team members of Centre’s Urban History Documentation Archive. This Pilot Project could not be implemented without the hard work of two young and energetic Research Assistants, Ayan Kundu and Krishnapriya Chakravarti. We wish to acknowledge their contribution to this project. Finally, I am thankful to my college authority for providing all sorts of support for successful completion of the project. -

Chapter 1 Nation and Nationalism
University of Warwick institutional repository: http://go.warwick.ac.uk/wrap A Thesis Submitted for the Degree of PhD at the University of Warwick http://go.warwick.ac.uk/wrap/60257 This thesis is made available online and is protected by original copyright. Please scroll down to view the document itself. Please refer to the repository record for this item for information to help you to cite it. Our policy information is available from the repository home page. “The Home and the World” Representations of English and Bhashas in Contemporary Indian Culture Vedita Cowaloosur A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy in English and Comparative Literary Studies University of Warwick Department of English and Comparative Literary Studies June 2013 [S]he wanted words with the heft of stainless steel, sounds that had been boiled clean, like a surgeon’s instruments, with nothing attached except meanings that could be looked up in a dictionary— —Amitav Ghosh, The Hungry Tide vvv […] there are no “neutral” words and forms—words and forms can belong to “no one;” language has been completely taken over, shot through with intentions and accents. —Mikhail Bakhtin, The Dialogic Imagination 4 TABLE OF CONTENTS LIST OF IMAGES 6 ACKNOWLEDGEMENTS 7 DECLARATION 8 ABSTRACT 9 ABBREVIATIONS 10 INTRODUCTION 11 A. AAMCHI MUMBAI 11 B. INDIAN FICTION AND THE POLITICS OF LANGUAGE 25 C. THESIS STRUCTURE 36 CHAPTER 1 NATION AND NATIONALISM 40 1.1. LANGUAGE AND THE “NATION” QUESTION 42 1.2. LINGUISTIC NATIONALISM IN THE INDIAN SUBCONTINENT 47 1.3. -

From Krishna Pal to Lal Behari Dey: Indian Builders of the Church in India Or Native Agency in Bengal 1800-1880
From Krishna Pal to Lal Behari Dey: Indian Builders of the Church in India or Native Agency in Bengal 1800-1880 Eleanor Jackson Senior Lecturer in Religious Studies, University of Derby [email protected] __________ This title has a distinctly eighteenth century ring to it, being a composite title created from my original title and that which was assigned to it in the 1997 Edinburgh North Atlantic Missiology Project consultation programme. It encapsulates the change in attitude to 'native agents' since the paternalism of the era so famously described in V.S. Azariah's address to delegates to the Edinburgh 1910 World Missionary Conference.(l) On the other hand, the problem in using my title is that the names of Krishna Pal (l764-1822) and Lal Behari Dey (l824-1894) are relatively unknown, although this would not have been the case during the years when they were active in mission service, and missionary magazines were required reading on the Victorian Sabbath both in Britain and Europe.(2) Hence the descriptive clause, 'Indian Builders of the Indian churches.' 'Indian Builders of the Indian Churches' is also more appropriate in the jubilee year of the Church of South India, at a time of celebrations for fifty years of Indian independence, and it is within that conceptual framework that this paper is constructed. In each clause a chronological span is suggested. For in the first, Krishna Pal was the first Indian Baptist convert, baptised 28 December 1800 and received into full membership of the Church in Serampore on the first Saturday in 1801, and Lal Behari Dey, active even in retirement from his professorship, died at a venerable age in 1894 after more than forty years as missionary and minister of the Free Church of Scotland Mission. -

Purba Bardhaman District at a Glance
PURBA BARDHAMAN DISTRICT AT A GLANCE The name Burdwan is the anglicized form of Barddhaman. (also spelled as Burdwan or Burdhman) is a district in West Bengal. There are two schools of thoughts about the name Barddhaman. It might have been named after the 24th Jaina Tirthankar. According to Kalpasutra of the Jains, Mahavira spent sometime in Astikagram which was formerly known as Barddhaman. According to the second school, Barddhaman means prosperous growth centre. In the progress of Aryanisation from Upper Ganges valley, the frontier colony was called Barddhaman as a landmark of growth and prosperity. The name came to stay as the Aryans failed to consolidate their gains further east. District : Purba Bardhaman, State : West Bengal Social & Resource Map Showing River System of Purba Bardhaman District The main towns of the district is Burdwan, Kalna & Katwa Geography: Total Geographical Area: 5432.69 sq. km. The district extends from 22°56' to 23°53' N latitude and from 86°48' to 88°25' E longitudes. Lying within Burdwan Division, the district is bounded on the north by Birbhum and Murshidabad, on the east by Nadia, on the south by Hooghly, Bankura and Purulia and on the west by Paschim Bardhaman districts. RIVERS : The river system in Purba Barddhaman includes the Bhagirathi-Hooghly in the east, the Ajoy and its tributaries in the north and the Dwarakeswar, the Damodar and its branches in the south-west. Besides, there are innumerable Khals and old river beds all over the area. WATER RESOURCES : There are many tanks, wells, canals, swamps and bils are found all over the district. -

State District Branch Address Centre Ifsc
STATE DISTRICT BRANCH ADDRESS CENTRE IFSC CONTACT1 CONTACT2 CONTACT3 MICR_CODE A.N.REDDY NAGAR ANDHRA A N REDDY BR,NIRMAL,ANDHRA PRADESH ADILABAD NAGAR PRADESH NIRMAL ANDB0001972 8734243159 NONMICR 3-2-29/18D, 1ST CH.NAGAB FLOOR, AMBEDKAR HUSHANA ANDHRA CHOWK ADILABAD - M 08732- PRADESH ADILABAD ADILABAD 504 001 ADILABAD ANDB0000022 230766 TARA COMPLEX,MAIN ANDHRA ROAD,ASIFABAD,ADI 08733 PRADESH ADILABAD ASIFABAD LABAD DT - 504293 ASIFABAD ANDB0002010 279211 504011293 TEMPLE STREET, BASARA ADILABAD, ANDHRA ADILABAD, ANDHRA 986613998 PRADESH ADILABAD BASARA PRADESH-504104 BASAR ANDB0001485 1 Bazar Area, Bellampally , Adilabad G.Jeevan Reddy ANDHRA Dist - - 08735- PRADESH ADILABAD Bellampalli Bellampalli ADILABAD ANDB0000068 504251 2222115 ANDHRA BANK, BHAINSA BASAR P.SATYAN ROAD BHAINSA- ARAYANA - ANDHRA 504103 ADILABAD 08752- PRADESH ADILABAD BHAINSA DIST BHAINSA ANDB0000067 231108 D.NO 4-113/3/2,GOVT JUNIOR COLLEGE ROAD,NEAR BUS ANDHRA STAND,BOATH - 949452190 PRADESH ADILABAD BOATH 504305 BOATH ANDB0002091 1 MAIN ROAD,CHENNUR, ADILABAD DIST, ANDHRA CHENNUR, ANDHRA 087372412 PRADESH ADILABAD CHENNUR PRADESH-504201 CHINNOR ANDB0000098 36 9-25/1 BESIDE TANISHA GARDENS, ANDHRA DASNAPUR, PRADESH ADILABAD DASNAPUR ADILABAD - 504001 ADILABAD ANDB0001971 NO NONMICR ORIENT CEMENT WORKS CO, DEVAPUR,ADILABAD DIST, DEVAPUR, ANDHRA ANDHRA PRADESH- 08736 PRADESH ADILABAD DEVAPUR 504218 DEVAPUR ANDB0000135 240531 DOWEDPALLI, LXXETTIPET 08739- ANDHRA VILLAGE, GANDHI DOWDEPAL 233666/238 PRADESH ADILABAD DOWDEPALLI CHOWK LI ANDB0000767 222 H NO 1-171 VILL -

Whatever Happened to Hindustani?
WHATEVER HAPPENED TO HINDUSTANI? LANGUAGE POLITICS IN LATE COLONIAL INDIA A THESIS SUBMITTED TO THE GRADUATE DIVISION OF THE UNIVERSITY OF HAWAI‘I AT MĀNOA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS IN HISTORY DECEMBER 2012 By Richard Forster Thesis Committee: Ned Bertz, Chairperson Peter H. Hoffenberg Miriam Sharma ii Acknowledgements In the course of completing this thesis and other requirements for the MA degree I have become indebted to numerous individuals as well as several institutions for various forms of encouragement and support. Firstly and above all I want to thank Lorinda and Lichen for putting up with me and my often irascible temperament, almost always without complaint, and for supporting me so selflessly that I have been largely free to pursue my studies over the last several years. Without your hard work and many sacrifices it would surely have been impossible for me to spend so much time trying to learn something more about South Asian history and culture, and I am more grateful to both of you than you can know. Similarly, our extended family in both Australia and the USA have been consistently generous, offering both material and moral support without which this study would have so much more challenging. This thesis concerns aspects of the history of certain South Asian languages, in particular Hindi and Urdu, (or Hindustani), but in a way, Sanskrit and Persian as well. Now that I take stock of my attempts to learn each of these languages I realize that I have been assisted in no small way by a rather large cohort of language teachers, for each of whom I hold enormous fonts of respect, affection and gratitude. -
A Revised and En Larged Account of the Bobbili Zeiviindari
A REV I SED AN D EN LARGED ACCO UNT O F T H E BOBBI LI ZEIVI I N DARI , CO M PI LE D BY M A HA - RAJ AH SA H E B M E H A R BAN - I - DO STA N MAHA- RAJAH SR I RAO SI R V E N KATA SWETAC HA LA PATI K C I E . N G - RAO B H D U R . RA A A A , , B B MA HARAJ AH O F BO I L I . SECO N D ED I TI O N . M A D R AS PR I NTE D BY AD D I SO N 6: CO . P R E F A C E . ( F I R S T E D I T I O N ) . H E “ T compiler of the Bobbili Zemindari , 1 889 which was publ ished i n , made a gross mistake as to the Founder o f the Sama sth an am n t o ; and subseque t its publication , some more records and further accounts have been obtained from several sources . I t o have , therefore , undertaken write this Revised and Enlarged History o f the Zemindari , and it took m e more than a year t o identify the Founder of the Sam asth an am . R . B O B B I L I . , V S , 66 71 1 9 0 8 0 2 . 0 . This Second Edition published in 1 907 brings the History of the S am asth an am up to date . R . V .