1 Ben -Shoshan PN Version 3 February 8, 2018 1 Peanut/Tree Nut
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tree Nut Allergy
TREE NUT ALLERGY Tree nut allergy is one of the most common food allergies in children and adults, and can cause a severe, potentially fatal allergic reaction (anaphylaxis). Tree nuts include, but are not limited to: almond, Brazil nut, cashew, hazelnut, macadamia, pecan, pine nut, pistachio and walnut. These are not to be confused or grouped together with peanut, which is a legume, or seeds, such as sunflower or sesame. What is a food allergy? test results with the information given Severe Symptoms or Anaphylaxis in your medical history for a diagnosis. Food allergy is a serious medical These tests may include: LUNG: Shortness of breath, condition affecting up to 32 million wheezing, repetitive cough people in the United States, including ● Skin prick test 1 in 13 children. Food allergy happens ● Blood test HEART: Pale or bluish skin, when your body’s immune defenses ● Oral food challenge faintness, weak pulse, dizziness that normally fight disease attack a ● Trial elimination diet food protein instead. The food protein THROAT: Tight or hoarse throat, is called an allergen, and your body’s Oral food challenges are considered the trouble breathing or swallowing response is called an allergic reaction. gold standard for definitive diagnosis. MOUTH: Significant swelling of the How common are nut allergies? Depending on your medical history and tongue or lips initial test results, you may need to take Nine foods account for a majority of more than one test before receiving your SKIN: Many hives over body, reactions: milk, eggs, peanuts, tree nuts, diagnosis. widespread redness soy, wheat, fish, sesame and shellfish. -

An Update on Food Allergen Management and Global Labeling
An Update on Food Allergen Management and Global Labeling Regulations A Thesis SUBMITTED TO THE FACULTY OF UNIVERSITY OF MINNESOTA BY Xinyu Diao IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE Advisor: David Smith, Ph.D. Aug 2017 © {Xinyu Diao} {2017} Acknowledgements I would like to thank my advisor Dr. David Smith for his guidance and support throughout my Master’s program. With his advice to join the program, my wonderful journey at the University of Minnesota began. His tremendous support and encouragement motivates me to always dream big. I would like to also thank Dr. Jollen Feritg, Dr. Len Marquart and Dr. Adam Rothman for being willing to take their valuable time to serve as my committee members. I am grateful to many people whose professional advice is invaluable over the course of this project. I would like to take this opportunity to show appreciation for Dr. Gerald W. Fry for being a role model for me as having lifetime enthusiasm for the field you study. I wouldn’t be where I am now without the support of my friends. My MGC (Graduate Student Club) friends who came all around the world triggered my initial interest to investigate a topic which has been concerned in a worldwide framework. Finally, I would like to give my most sincere gratitude to my family, who provide me such a precious experience of studying abroad and receiving superior education. Thank you for your personal sacrifices and tremendous support when I am far away from home. i Dedication I dedicate this thesis to my father, Hongquan Diao and my mother, Jun Liu for their unconditional love and support. -
Apr2018training.Pdf
AccommodatingChildrenwithSpecial Dietary Needs in the School Nutrition Programs; Guidance for School Foodservice Staff Celiac disease evidence analysis project. Celiac disease (CD) evidence-based nutrition practice guideline. Wheat allergy. Wheat allergy symptoms. The gluten-free nutrition guide. Guidance related to the ADAamendments act. Food allergies: What you need to know. Celiac Disease Food Allergens Food Allergy: Tree Nut & Wheat Post Test – April 2018 Please keep this test and certificate in your files for Licensing. You do not need to send it in to our office or the State. 1. Disclosure on food labels of all tree nuts is required by _____. 2. Tree nuts tend to cause particularly severe ______ _______, even if very small amounts are consumed. 3. Tree nuts can be found in household products such as lotions and soaps. True or False? 4. A product that is labeled as being produced in a facility with tree nuts can be safely consumed by an individual with a tree nut allergy. True or False? 5. Nutmeg and water chestnuts are safe for a person with tree nut allergies because nutmeg is a _______and water chestnut is a _______. 6. Wheat allergy is an abnormal immune system reaction to one of the four _________ found in wheat: gluten, albumin, globulin, gliadin. 7. Many condiments such as soy sauce, ketchup and mustard can contain wheat. True or False? 8. Barley, chickpea, cornmeal and quinoa are all considered good wheat alternatives. True or False? 9. Life‐threatening food allergies are considered ____________. 10. Celiac disease is an inherited or genetic autoimmune disease characterized by sensitivity to the protein ___________. -
Peanut and Tree Nut Allergy
In partnership with Primary Children’s Hospital Peanut and Tree Nut Allergy What is a peanut or tree nut allergy? Your child may need to avoid products that could A peanut allergy is an immune reaction to proteins have a high risk for cross-contamination. For this in peanuts. A tree nut allergy is an immune reaction reason your child may need to avoid all peanuts and to proteins in various tree nuts. Some children may tree nuts. be allergic to only certain types of tree nuts. Some Cross-reactivity can also occur. This is when the children may be allergic to both peanuts and various proteins in one food are similar to those in another. types of tree nuts. The immune system sees them as the same and can Some common symptoms of allergy reactions include: cause an allergic reaction. Your child’s doctor will best be able to tell you your child’s risk for cross-reactivity Skin: reactions. They can tell you whether or not to avoid • itchy red rash • flushing additional foods that may cause those reactions. • hives • swelling of face What do I look for when I read the • eczema food labels? Digestive system: 1 Labels on food, that are regulated by the FDA, • belly pain • severe nausea have to say if the food contains the 8 most • blood or mucous in • cramping common food allergens: milk, egg, soy, wheat, stools • itching or swelling of peanuts, tree nuts, shellfish, or fish. Always read • severe diarrhea the lips, mouth, tongue the ingredient list to be sure and check all food • vomiting or throat. -

Pdf/13 243135 a Food When Compared with the Lower Grades
446 Letters / Ann Allergy Asthma Immunol 120 (2018) 429–447 ‡Allergy/Immunology Associates, Inc [4] Lawson E, Bond K, Churchill D, Walker-Bone K. A case of immune reconstitu- Mayfield Heights, Ohio tion syndrome: adult-onset Still’s disease in a patient with HIV infection. Rheumatology. 2009;48:446–447. [email protected] [5] Takeuchi T, Nakagawa T, Maeda Y, et al. Functional defect of B lymphocytes in a patient with selective IgM deficiency associated with systemic lupus erythe- matosus. Autoimmunity. 2001;34:115–122. [6] Kimura S, Tanigawa M, Nakahashi Y, et al. Selective IgM deficiency in a patient References with Hashimoto’s disease. Intern Med. 1993;32:302–307. [7] Antar M, Lamarche J, Peguero A, Reiss A, Cole S. A case of selective immuno- [1] Louis AG, Gupta S. Primary selective IgM deficiency: an ignored immunodefi- globulin M deficiency and autoimmune glomerulonephritis. Clin Exp Allergy. 2008; ciency. Clin Rev Allergy Immunol. 2014;46:104–111. 12:300–304. [2] Efthimiou P, Paik PK, Bielory L. Diagnosis and management of adult onset Still’s [8] Inoue T, Okumura Y, Shirama M, Ishbashi H, Kashiwagi S, Okubo H. Selective disease. Ann Rheum Dis. 2006;65:564–572. partial IgM deficiency: functional assessment of T and B lymphocytes in vitro. [3] Lee SJ, Cho YN, Kim TJ, et al. Natural killer T cell deficiency in active adult- J Clin Immunol. 1986;6:130–135. onset Still’s disease: correlation of deficiency of natural killer T cells [9] Ideura G, Agematsu K, Komatsu Y, et al. Selective IgM deficiency accompanied with dysfunction of natural killer cells. -

Tree Nut Allergy
Allergy and Immunology Tree Nut Allergy The term tree nuts refers to nuts other than peanut and includes - cashew, walnut, almond, pecan, pistachio, brazil nut, hazelnut and macadamia. These nuts contain protein that can cause an allergic reaction for around 2% of children. The type and severity of reactions to tree nuts can vary together with peanut, tree nuts are the most common foods to cause anaphylaxis in Australia, particularly cashews. Most people allergic to one tree nut do not have allergies to any other nuts but approximately 30% will have another tree nut allergy. Common coexisting tree nut allergies are cashew-pistachio and walnut-pecan. Your doctor will tell you which nuts you should avoid based on allergy testing, your child’s age and severity of past reactions. Will my child grow out of their tree nut allergy? Around 10% of children with an allergy to any of the tree nuts may outgrow one or all of their allergies. The doctors will determine whether your child has outgrown any of the tree nut allergies by a combination of allergy testing and food challenge. Allergy testing may be periodically repeated to monitor your child’s allergies. Challenges should only be performed by experienced medical staff with emergency resuscitation medications and facilities available. Once your child is safely eating certain nuts it is advisable to continue to include them as a regular part of your child’s diet. For younger children or those that do not like to eat nuts this can be done in a ground form added to other foods such as cereal, baked goods or yoghurt. -
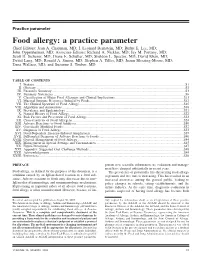
Food Allergy: a Practice Parameter (2006)
Practice parameter Food allergy: a practice parameter Chief Editors: Jean A. Chapman, MD; I. Leonard Bernstein, MD; Rufus E. Lee, MD; John Oppenheimer, MD; Associate Editors: Richard A. Nicklas, MD; Jay M. Portnoy, MD; Scott H. Sicherer, MD; Diane E. Schuller, MD; Sheldon L. Spector, MD; David Khan, MD; David Lang, MD; Ronald A. Simon, MD; Stephen A. Tilles, MD; Joann Blessing-Moore, MD; Dana Wallace, MD; and Suzanne S. Teuber, MD TABLE OF CONTENTS I. Preface.................................................................................................................................................................................S1 II. Glossary...............................................................................................................................................................................S2 III. Executive Summary ............................................................................................................................................................S3 IV. Summary Statements ..........................................................................................................................................................S6 V. Classification of Major Food Allergens and Clinical Implications ................................................................................S11 VI. Mucosal Immune Responses Induced by Foods..............................................................................................................S12 VII. The Clinical Spectrum of Food Allergy ..........................................................................................................................S15 -

The Peanut / Nut Allergy Handout
The Peanut / Nut Allergy Handout Dr. Antony Ham Pong answers some common peanut and tree nut allergy questions in this handout (updated in 2008) that he shares with AllergicLiving.com’s audience. Dr. Ham Pong has a private allergy and asthma practice in Ottawa and practises at the chest clinic in the Children’s Hospital of Eastern Ontario. By Dr. Antony Ham Pong Peanut and tree nut allergies are the most common life-threatening food allergies in children. They are often lifelong but between one in 10 and one in 20 children can outgrow a peanut allergy . Children with peanut allergy often cannot stand the smell of peanut, may refuse to touch it, and do not want to stay around when peanut butter is being eaten. This type of violent rejection of peanut butter may be the first sign that a child is peanut allergic even if the child has never eaten it. Sometimes these children get hives or rash where peanut butter touches the face or skin. If a peanut allergic child touches peanut and then rubs his or her eyes, the eyes may become very swollen and puffy. Q. What can happen during an allergic reaction to peanut? A. An allergic reaction to a food usually begins within minutes but may be delayed for 2 to 4 hours and usually lasts only several hours, occasionally a day. The more severe the allergy, the smaller the amount required to cause a reac tion. Typical immediate allergic reactions to foods include hives or blotching around the mouth, which may spread to the rest of the body, immediate runny nose, sneezing and itchy watery eyes, coughing, choking or gagging, wheezing and trouble breathing, and cramps, vomiting and diarrhea. -
Peanut and Tree Nut Allergy
Peanut and tree nut allergy Background Nut allergy, to both peanuts and tree nuts, is one of the commonest food allergies, affecting about 1-2% (1 in 100 to 1 in 50) of children in Britain. The prevalence of nut allergy, as with all allergic conditions, is increasing. Risk factors for the development of nut allergy are a family history with an affected brother or sister, moderate to severe eczema and/or egg allergy. There is no evidence that if a mother eats nuts when she is pregnant or breast-feeding that her child is at greater risk of developing nut allergy; indeed recent evidence suggests that early contact (from 4 months old) may prevent the child from developing nut allergy. This has recently been confirmed by the LEAP study in children with egg allergy or severe eczema. As well as being one of the commonest food allergies, nut allergy is unfortunately also one of the most dangerous as it can cause severe reactions (anaphylaxis). Some children are very sensitive and only very small amounts of nut (2-5mg) are needed to trigger a full allergic or anaphylactic reaction (compared with 300- 500mg of egg). Non-ingestion contact, from touching nuts or inhaling airborne allergens (dust), is very unlikely to trigger a severe reaction. The peanut is not really a nut. It belongs to the legume family and is related to beans, peas, lentils, soya and lupin. Children who are peanut allergic rarely react to the other legumes (only around 5%). By contrast, children who are allergic to one tree nut a have a greater risk (about 40%) of allergy to another tree nut. -

Grass Pollens • Almond Is the Edible Seed of a Drupe in This Series
Legumes, Nuts & Seeds Allergy – Which allergens? Author: Dr Harris Steinman, Allergy Resources International, P O Box 565, Milnerton 7435, South Africa, [email protected]. All rights reserved. No part of this publication may be reproduced in any form without the written consent of Phadia AB. ©Phadia AB, 2008 Design: RAK Design AB, 2008 Printed by: X-O Graf Tryckeri AB, Uppsala, Sweden ISBN 91-970475-5-4 Contents Introduction ............................................................................. 5 f20 Almond (Amygdalus communis) ..................................... 9 f6 Barley (Hordeum vulgare) ............................................ 15 f310 Blue vetch (Lathyrus sativus) ....................................... 22 f18 Brazil nut (Bertholletia excelsa) ................................... 26 f11 Buckwheat (Fagopyrum esculentum) ............................ 32 f202 Cashew nut (Anacardium occidentale) .......................... 41 f309 Chick pea (Cicer arietinus) .......................................... 49 f36 Coconut (Cocos nucifera) ............................................. 54 f55 Common millet (Panicum milliaceum) .......................... 59 f305 Fenugreek (Trigonella foenum-graecum) ........................ 64 f56 Foxtail millet (Setaria italica) ....................................... 67 f79 Gluten (from Triticum aestivum) ................................... 70 f315 Green bean (Phaseolus vulgaris) ................................... 77 f17 Hazel nut (Corylus avellana) ....................................... -

Novel Sources of Food Allergens
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Dissertations, Theses, & Student Research in Food Science and Technology Food Science and Technology Department Spring 5-2021 NOVEL SOURCES OF FOOD ALLERGENS Lee Palmer University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/foodscidiss Part of the Food Chemistry Commons Palmer, Lee, "NOVEL SOURCES OF FOOD ALLERGENS" (2021). Dissertations, Theses, & Student Research in Food Science and Technology. 116. https://digitalcommons.unl.edu/foodscidiss/116 This Article is brought to you for free and open access by the Food Science and Technology Department at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Dissertations, Theses, & Student Research in Food Science and Technology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. NOVEL SOURCES OF FOOD ALLERGENS by Lee Palmer A DISSERTATION Presented to the Faculty of The Graduate College at the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Doctor of Philosophy Major: Food Science and Technology Under the Supervision of Professor Philip E. Johnson Lincoln, Nebraska May 2021 NOVEL SOURCES OF FOOD ALLERGENS Lee Palmer, Ph.D. University of Nebraska, 2021 Advisor: Philip E. Johnson Technological advancement and globalization have led to the spread of foods to countries where the food does not yet have a documented history of consumption, in other words, novel foods. Novel foods also encompass truly novel foods, foods that have been processed in a novel manner, and novel means of exposure. With novel foods comes the potential of food allergens that pose an uncharacterized risk to those with food allergies. -
Tree Nut Allergy and Tree Nut Free Diet
Tree nut allergy and tree nut free diet What are tree nuts? tree nuts often happens the first time a child is known to eat the nut, often around 2-4 years of age. The term tree nut is used to mean nuts including: How common is tree nut allergy? Almond, Brazil, In Western communities, about 1 in 500 children (0.2%) Cashew, have a reaction to tree nuts by the age of 5 years. Allergy Chestnut, to some tree nuts, e.g. cashew nut, is becoming more Hazelnut, common. Children are more likely to have a tree nut Hickory, allergy if they have other allergic diseases (asthma, atopic Macadamia, dermatitis, and other food allergies). Pecan What are the symptoms of tree nut allergy? Pistachio Walnut Reactions can range from mild to severe. These are different from peanuts (known as groundnuts) Mild to moderate reactions include: because tree nuts come from a different plant family. hives or welts People who are allergic to peanuts are not always allergic swelling of the lips/face/eyes to tree nuts. People who are allergic to one tree nut are tingling of the mouth often allergic to other tree nuts. (Pine nuts are seeds. abdominal pain or vomiting. Coconuts are not tree nuts) Severe reactions (anaphylaxis) include: What is tree nut allergy? difficulty/noisy breathing Tree nut allergy is a reaction that happens soon after swelling of the tongue eating tree nuts. The symptoms can be within minutes swelling or tightness in the throat but can be up to 2 hours after eating the nut.