Final RBF Booklet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midlands Province Mobile Voter Registration Centres
Midlands Province Mobile Voter Registration Centres Chirumhanzu District Team 1 Ward Centre Dates 18 Mwire primary school 10/06/13-11/06/13 18 Tokwe 4 clinic 12/06/13-13/06/13 18 Chingegomo primary school 14/06/13-15/06/13 16 Chishuku Seondary school 16/06/13-18/06/13 9 Upfumba Secondary school 19/06/13-21/06/13 3 Mutya primary school 22/06/13-24/06/13 2 Gonawapotera secondary school 25/06/13-27/06/13 20 Wildegroove primary school 28/06/13-29/06/13 15 Kushinga primary school 30/06/13-02/07/13 12 Huchu compound 03/07/13-04/-07/13 12 Central estates HQ 5/7/13 20 Mtao/Fair Field compound 6/7/13 12 Chiudza homestead 07/07/13-08/06/13 14 Njerere primary school 9/7/13 Team 2 Ward Centre Dates 22 Hillview Secondary school 10/07/13-12/07/13 17 Lalapanzi Secondary school 13/07/13-15/07/13 16 Makuti homestead 16/06/13-17/06/13 1 Mapiravana Secondary school 18/06/13-19/06/13 9 Siyahukwe Secondary school 20/06/13-23/06/13 4 Chizvinire primary school 24/06/13-25/06/13 21 Mukomberana Seconadry school 26/06/13-29/06/13 20 Union primary school 30/06/13-01/07/13 15 Nyikavanhu primary school 02/07/13-03/07/13 19 Musens primary school 04/07/13-06/07/13 16 Utah primary school 07/7/13-09/07/13 Team 3 Ward Centre Dates 11 Faerdan primary school 10/07/13-11/07/13 11 Chamakanda Secondary school 12/07/13-14/07/13 11 Chamakanda primary school 15/07/13-16/07/13 5 Chizhou Secondary school 17/06/13-16/06/13 3 Chilimanzi primary school 21/06/13-23/06/13 25 Maponda primary school 24/06/13-25/06/13 6 Holy Cross seconadry school 26/06/13-28/06/13 20 New England Secondary -

Mashonaland Central Province Zimbabwe Vulnerability Assessment Committee (Zimvac) 2020 Rural Livelihoods Assessment Report Foreword
Mashonaland Central Province Zimbabwe Vulnerability Assessment Committee (ZimVAC) 2020 Rural Livelihoods Assessment Report Foreword The Zimbabwe Vulnerability Assessment Committee (ZimVAC) under the coordination of the Food and Nutrition Council, successfully undertook the 2020 Rural Livelihoods Assessment (RLA), the 20th since its inception. ZimVAC is a technical advisory committee comprised of representatives from Government, Development Partners, UN, NGOs, Technical Agencies and the Academia. In its endeavour to ‘promote and ensure adequate food and nutrition security for all people at all times’, the Government of Zimbabwe has continued to exhibit its commitment for reducing food and nutrition insecurity, poverty and improving livelihoods amongst the vulnerable populations in Zimbabwe through operationalization of Commitment 6 of the Food and Nutrition Security Policy (FNSP). As the country is grappling with the COVID-19 pandemic, this assessment was undertaken at an opportune time as there was an increasing need to urgently collect up to date food and nutrition security data to effectively support the planning and implementation of actions in a timely and responsive manner. The findings from the RLA will also go a long way in providing local insights into the full impact of the Corona virus on food and nutrition security in this country as the spread of the virus continues to evolve differently by continent and by country. In addition, the data will be of great use to Government, development partners, programme planners and communities in the recovery from the pandemic, providing timely information and helping monitor, prepare for, and respond to COVID-19 and any similar future pandemics. Thematic areas covered in this report include the following: education, food and income sources, income levels, expenditure patterns and food security, COVID-19 and gender based violence, among other issues. -

PLAAS RR46 Smeadzim 1.Pdf
Chrispen Sukume, Blasio Mavedzenge, Felix Murimbarima and Ian Scoones Faculty of Economic and Management Sciences Research Report 46 Space, Markets and Employment in Agricultural Development: Zimbabwe Country Report Chrispen Sukume, Blasio Mavedzenge, Felix Murimbarima and Ian Scoones Published by the Institute for Poverty, Land and Agrarian Studies, Faculty of Economic and Management Sciences, University of the Western Cape, Private Bag X17, Bellville 7535, Cape Town, South Africa Tel: +27 21 959 3733 Fax: +27 21 959 3732 Email: [email protected] Institute for Poverty, Land and Agrarian Studies Research Report no. 46 June 2015 All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means without prior permission from the publisher or the authors. Copy Editor: Vaun Cornell Series Editor: Rebecca Pointer Photographs: Pamela Ngwenya Typeset in Frutiger Thanks to the UK’s Department for International Development (DfID) and the Economic and Social Research Council’s (ESRC) Growth Research Programme Contents List of tables ................................................................................................................ ii List of figures .............................................................................................................. iii Acronyms and abbreviations ...................................................................................... v 1 Introduction ........................................................................................................ -

Cultural Practices Associated with Death in the North Nyanga District of Zimbabwe and Their Impact on Widows and Orphans +
The African e-Journals Project has digitized full text of articles of eleven social science and humanities journals. This item is from the digital archive maintained by Michigan State University Library. Find more at: http://digital.lib.msu.edu/projects/africanjournals/ Available through a partnership with Scroll down to read the article. Journal of Social Development in Africa (1996), 11,1, 79-86 Cultural Practices Associated with Death in the North Nyanga District of Zimbabwe and their Impact on Widows and Orphans + DREW, R S *; FOSTER, G *; CHITIMA, J ** ABSTRACT This survey examines the cultural practices associated with death in the Nyanga North area of Zimbabwe and their impact on widows and orphans in 211 families. In addition to the concepts of pre-planning for death, property and wife inheritance, relevant aspects of life such as marriage, patriarchal succession and sickness are also considered. It is unclear what pattern of care and support for widows is emerging to replace the declining practice of wife inheritance. The implication of these factors on the planning of effective intervention strategies is considered. Introduction AIDS has been spreading rapidly through Zimbabwe as in other sub-Saharan African countries. Serosurveillance studies (MOH, 1993) carried out in antenatal mothers have shown HIV prevalence levels of over 30% in urban areas and around 20% in rural areas. The Elim Pentecostal Church of Zimbabwe (EPCZ) administers a church centre in the communal lands in the northern part of Nyanga District in the north-eastern part of Zimbabwe close to the border with Mozambique. This centre provides educational and health services to the community in the surrounding area. -

For Human Dignity
ZIMBABWE HUMAN RIGHTS COMMISSION For Human Dignity REPORT ON: APRIL 2020 i DISTRIBUTED BY VERITAS e-mail: [email protected]; website: www.veritaszim.net Veritas makes every effort to ensure the provision of reliable information, but cannot take legal responsibility for information supplied. NATIONAL INQUIRY REPORT NATIONAL INQUIRY REPORT ZIMBABWE HUMAN RIGHTS COMMISSION ZIMBABWE HUMAN RIGHTS COMMISSION For Human Dignity For Human Dignity TABLE OF CONTENTS FOREWORD .................................................................................................................................................. vii ACRONYMS.................................................................................................................................................... ix GLOSSARY OF TERMS .................................................................................................................................. xi PART A: INTRODUCTION TO THE NATIONAL INQUIRY PROCESS ................................................................ 1 CHAPTER 1: INTRODUCTION ........................................................................................................................ 1 1.1 Establishment of the National Inquiry and its Terms of Reference ....................................................... 2 1.2 Methodology ..................................................................................................................................... 3 CHAPTER 2: THE NATIONAL INQUIRY PROCESS ......................................................................................... -

Zimbabwe.Beef.20190321.Approved V2
Value Chain Analysis for Development (VCA4D) is a tool funded by the European Commission / DEVCO and is implemented in partnership with Agrinatura. Agrinatura (http://agrinatura-eu.eu) is the European AllianCe of Universities and Research Centers involved in agricultural researCh and CapaCity building for development. The information and knowledge produCed through the value Chain studies are intended to support the Delegations of the European Union and their partners in improving poliCy dialogue, investing in value Chains and better understanding the Changes linked to their aCtions VCA4D uses a systematiC methodologiCal framework for analysing value Chains in agriCulture, livestoCk, fishery, aquaCulture and agroforestry. More information inCluding reports and communication material Can be found at: https://europa.eu/CapaCity4dev/value-chain-analysis-for- development-vca4d- Team Composition Ben Bennett, Team Leader and eConomist (NRI) Muriel Figué, social expert (CIRAD) Mathieu Vigne, environmental expert (CIRAD) Charles Chakoma, national consultant (independent) Pamela KatiC, support to economist (NRI) The report was produCed through the finanCial support of the European Union. Its content is the sole responsibility of its authors and does not neCessarily refleCt the views of the European Union. The report has been realised within a projeCt finanCed by the European Union (VCA4D CTR 2016/375-804). Citation of this report: Bennett, B., Chakoma, C., Figué, M, Vigne, M., KatiC, P.; 2019. Beef Value Chain Analysis in Zimbabwe. Report for the -
Back to Index MOBILE REGISTRATION PROGRAMME
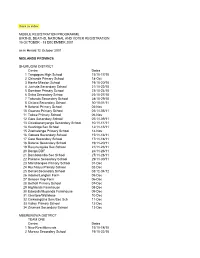
Back to index MOBILE REGISTRATION PROGRAMME BIRTHS, DEATHS, NATIONAL AND VOTER REGISTRATION 15 OCTOBER - 13 DECEMBER 2001 as in Herald 12 October 2001 MIDLANDS PROVINCE SHURUGWI DISTRICT Centre Dates 1 Tongogara High School 15/10-17/10 2 Chironde Primary School 18-Oct 3 Hanke Mission School 19/10-20/10 4 Juchuta Secondary School 21/10-22/10 5 Dombwe Primary School 23/10-24/10 6 Svika Secondary Schoo 25/10-27/10 7 Takunda Secondary School 28/10-29/10 8 Chitora Secondary School 30/10-01/11 9 Batanai Primary School 02-Nov 10 Gwanza Primary School 03/11-05/11 11 Tokwe Primary School 06-Nov 12 Gare Secondary School 07/11-09/11 13 Chivakanenyanga Secondary School 10/11-11/11 14 Kushinga Sec School 12/11-13/11 15 Zvamatenga Primary School 14-Nov 16 Gamwa Secondary School 15/11-16/11 17 Gato Secondary School 17/11-18/11 18 Batanai Secondary School 19/11-20/11 19 Rusununguko Sec School 21/11-23/11 20 Donga DDF 24/11-26/11 21 Dombotombo Sec School 27/11-28/11 22 Pakame Secondary School 29/11-30/11 23 Marishongwe Primary School 01-Dec 24 Ruchanyu Primary School 02-Dec 25 Dorset Secondary School 03/12-04/12 26 Adams/Longton Farm 05-Dec 27 Beacon Kop Farm 06-Dec 28 Bethall Primary School 07-Dec 29 Highlands Farmhouse 08-Dec 30 Edwards/Muponda Farmhouse 09-Dec 31 Glentore/Wallclose 10-Dec 32 Chikwingizha Sem/Sec Sch 11-Dec 33 Valley Primary School 12-Dec 34 Zvumwa Secondary School 13-Dec MBERENGWA DISTRICT TEAM ONE Centre Dates 1 New Resettlements 15/10-18/10 2 Murezu Secondary School 19/10-22/10 3 Chizungu Secondary School 23/10-26/10 4 Matobo Secondary -

Epidemiological Bulletin Number 30 Week 43 (Week Ending 25 October 2009)
Epidemiological Bulletin Number 30 Week 43 (week ending 25 October 2009) Foreword This is the 2nd combined epidemiological bulletin to be issued. Information on other epidemics that arise shall also be included in this bulletin. Bulletins are published weekly. Note that the epidemiological week runs from Sunday to Saturday. The bulletin provides a weekly overview of the outbreaks in Zimbabwe, including province by province data, to inform and improve the continuing public health response. It also provides guidance to agencies on issues relating to data collection, analysis and interpretation, and suggests operational strategies on the basis of epidemiological patterns so far. The C4 team welcomes feedback and data provided by individual agencies will be verified with MOHCW structures before publication. Please send any comments and feedback to the Cholera Control and Command Centre Email: [email protected]. Toll free number for alert by district and province is 08089001 or 08089002 or 08 089000 Mobile number for alerts is 0912 104 257 Acknowledgements We are very grateful to MoHCW District Medical Officers, District and Provincial Surveillance Officers, Provincial Medical Directors, Environmental Heath Officers, and MoHCW's department of surveillance, who have helped to gather and share the bulk of the information presented here. Likewise, we acknowledge agencies, including members of the Health and WASH clusters, who have kindly shared their data with our team. MoHCW recognizes and thanks the efforts made by NGOs and other partners assisting in the response and providing support to MoHCW. Source: Ministry of Health and Child Welfare Rapid Disease Notification System 1 Figures See also summary tables (annex 1), maps (annex 2) and graphs (annex 3). -

The Political Economy of Civilisation: Peasant-Workers in Zimbabwe and the Neo-Colonial World
The Political Economy of Civilisation: Peasant-Workers in Zimbabwe and the Neo-colonial World Paris Yeros Thesis submitted for the degree of Doctor of Philosophy in International Relations, London School of Economics and Political Science, University of London UMI Number: U172056 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. Dissertation Publishing UMI U172056 Published by ProQuest LLC 2014. Copyright in the Dissertation held by the Author. Microform Edition © ProQuest LLC. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 TW£&£ S S097 ABSTRACT This thesis provides a global political economy of the postwar period, with special reference to Zimbabwe. The conceptual aim is to connect the agrarian question with contemporary democratic theory, by inquiring into the global sources of ‘civil society’ and relating it to the phenomenon of semi-proletarianisation. There are three basic arguments. First, civil society cannot be understood in isolation from imperialism. The onset of the Cold War produced an ultra-imperial order under US leadership, with a ‘global development’ project crafted to its needs and a mode of rule preoccupied with the definition and enforcement of ‘civil society’. Second, capital accumulation in the postwar period has continued to operate in accordance with the laws of motion of the centre-periphery relationship; the main alteration has consisted in the closer integration of central-state economies with each other, along with a small number of industrial satellites. -

Midlands ZIMBABWE POPULATION CENSUS 2012
Zimbabwe Provincial Report Midlands ZIMBABWE POPULATION CENSUS 2012 Population Census Office P.O. Box CY342 Causeway Harare Tel: 04-793971-2 04-794756 E-mail: [email protected] Census Results for Midlands Province at a Glance Population Size Total 1 614 941 Males 776 787 Females 838 154 Annual Average Increase (Growth Rate) 2.2 Average Household Size 4.5 1 2 Table of Contents Table of Contents...............................................................................................................................3 List of Tables.....................................................................................................................................4 Foreword ...........................................................................................................................................9 Executive Summary.........................................................................................................................10 Midlands Fact Sheet (Final Results) .................................................................................................13 Chapter 1: ........................................................................................................................................14 Population Size and Structure .......................................................................................................14 Chapter 2: ........................................................................................................................................24 Population Distribution -
Covid-19 Addendum
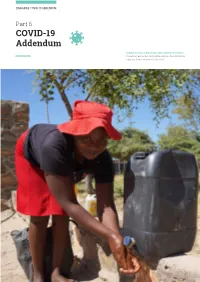
ZIMBABWE COVID-19 ADDENDUM Part 6 COVID-19 Addendum SHAMVA DISTRICT, MASHONALAND CENTRAL PROVINCE A beneficiary washes her hands before entering a food distribution in Shamva district. Photo:WFP/Claire Nevill 46 ZIMBABWE COVID-19 ADDENDUM COVID-19 Response at a Glance PEOPLE IN NEED PEOPLE TARGETED REQUIREMENTS (US$) OPERATIONAL PARTNERS 7.5M 5.9M $84.9M 37 People in Need and Targeted Requirements by Cluster H M Me Hurungwe Cy/ Mabani M F S M U Dwin Rushinga MASHONALAND CENTRAL Karoi M Guruve Mwi M Shamva M AIBA Kariba Zvimba B Pfungwe Cyi U M Mowe MASHONALAND EAST Education Ba Moko Nth MASHONALAND WEST Nton Goromonzi HARARE Mehwa B South Sanyati C Water S U Nanga V Monder M Kadoma M Town Seke U U C H WASH U MIDLANDS Mondera MANICALAND M-N Hdweza Rusape M Lupane Kwekwe MATEBELELAND NORTH K Nyi C N U M Hwange Redcliff M U C Ba urban Gutu Me Tsholotsho B Gweru U U P BV Byo C M MASVINGO I B C M Zvishavane U B Zvishavane U Z U U M C Potection Plumtree Mengwa MATEBELELAND SOUTH 2M C C Potection U U M Mobo M Gwanda Cedzi B SM M Propor IN Targeted B P geted U R 02M People in Need and Targeted by Cluster Operational Partners by Type Water S M H WASH 2M F S 0M M NNO Education M 9 M INO H M 18 0M PBV 2M 845K PP 22M UN 22 0 MS 20M 20 0M N 353K 2 S 91K In addition to the humanitarian response requirements, R 14K $4.5 million is needed to support Governance interventions 14K dination and $22.5 million for social protection, which will be 953 M 953 carried out by development actors. -

Fast Track Land Reform in Matepatepa Commercial Farming Area, Bindura District: Effects on Farm Workers, 2000 – 2010
Fast Track Land Reform in Matepatepa Commercial Farming Area, Bindura District: Effects on Farm Workers, 2000 – 2010. By Joyline Takudzwa Kufandirori THIS THESIS HAS BEEN SUBMITTED IN ACCORDANCE WITH THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS IN THE FACULTY OF THE HUMANITIES, FOR THE CENTRE OF AFRICA STUDIES AT THE UNIVERSITY OF THE FREE STATE. NOVEMBER 2015 SUPERVISOR: PROF. I. R. PHIMISTER CO-SUPERVISOR: DR. R. PILOSSOF Declaration I, Joyline Takudzwa Kufandirori declare that the Master’s research dissertation that I herewith submit for the Master’s Degree qualification, Arts at the University of the Free State is my own independent work, and that I have not previously submitted it for a qualification at another institution of higher learning. I, Joyline Takudzwa Kufandirori , hereby declare that I am aware that the copyright is vested in the University of the Free State. I, Joyline Takudzwa Kufandirori, hereby declare that all royalties as regards intellectual property that was developed during the course of and/ or in connection with the study at the University of the Free State, will accrue to the University. ……………………… ……………………… Joyline Takudzwa Kufandirori Bloemfontein 1 Table of Contents Abstract……………………………………………………………………………………………………………………………….i Acknowledgements..................................................................................................................iii Dedication …………………………………………………………………………………………………………………….……iv Acronyms……………………………………………………………………………………………………………………………iv Chapter One: Introduction and