Seizures (Epilepsy) and Brain Tumours - Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Status Epilepticus Clinical Pathway
JOHNS HOPKINS ALL CHILDREN’S HOSPITAL Status Epilepticus Clinical Pathway 1 Johns Hopkins All Children's Hospital Status Epilepticus Clinical Pathway Table of Contents 1. Rationale 2. Background 3. Diagnosis 4. Labs 5. Radiologic Studies 6. General Management 7. Status Epilepticus Pathway 8. Pharmacologic Management 9. Therapeutic Drug Monitoring 10. Inpatient Status Admission Criteria a. Admission Pathway 11. Outcome Measures 12. References Last updated: July 7, 2019 Owners: Danielle Hirsch, MD, Emergency Medicine; Jennifer Avallone, DO, Neurology This pathway is intended as a guide for physicians, physician assistants, nurse practitioners and other healthcare providers. It should be adapted to the care of specific patient based on the patient’s individualized circumstances and the practitioner’s professional judgment. 2 Johns Hopkins All Children's Hospital Status Epilepticus Clinical Pathway Rationale This clinical pathway was developed by a consensus group of JHACH neurologists/epileptologists, emergency physicians, advanced practice providers, hospitalists, intensivists, nurses, and pharmacists to standardize the management of children treated for status epilepticus. The following clinical issues are addressed: ● When to evaluate for status epilepticus ● When to consider admission for further evaluation and treatment of status epilepticus ● When to consult Neurology, Hospitalists, or Critical Care Team for further management of status epilepticus ● When to obtain further neuroimaging for status epilepticus ● What ongoing therapy patients should receive for status epilepticus Background: Status epilepticus (SE) is the most common neurological emergency in children1 and has the potential to cause substantial morbidity and mortality. Incidence among children ranges from 17 to 23 per 100,000 annually.2 Prevalence is highest in pediatric patients from zero to four years of age.3 Ng3 acknowledges the most current definition of SE as a continuous seizure lasting more than five minutes or two or more distinct seizures without regaining awareness in between. -

Cognitive Impairment: Causes, Diagnosis and Treatment
NEUROLOGY - LABORATORY AND CLINICAL RESEARCH DEVELOPMENTS COGNITIVE IMPAIRMENT: CAUSES, DIAGNOSIS AND TREATMENT No part of this digital document may be reproduced, stored in a retrieval system or transmitted in any form or by any means. The publisher has taken reasonable care in the preparation of this digital document, but makes no expressed or implied warranty of any kind and assumes no responsibility for any errors or omissions. No liability is assumed for incidental or consequential damages in connection with or arising out of information contained herein. This digital document is sold with the clear understanding that the publisher is not engaged in rendering legal, medical or any other professional services. NEUROLOGY – LABORATORY AND CLINICAL RESEARCH DEVELOPMENTS SERIES Intracranial Hypertension Stefan Mircea Iencean and Alexandru Vladimir Ciurea 2009 ISBN: 978-1-60741-862-7 (Hardcover Book) Intracranial Hypertension Stefan Mircea Iencean and Alexandru Vladimir Ciurea 2009 ISBN: 978-1-60876-549-2 (Online Book) Cerebral Blood Flow Regulation Nodar P. Mitagvaria and Haim (James) I. Bicher 2009 ISBN: 978-1-60692-163-0 Cerebral Ischemia in Young Adults: Pathogenic and Clinical Perspectives Alessandro Pezzini and Alessandro Padovani (Editors) 2009 ISBN: 978-1-60741-627-2 Dizziness: Vertigo, Disequilibrium and Lightheadedness Agnes Lindqvist and Gjord Nyman (Editors) 2009: ISBN 978-1-60741-847-4 Somatosensory Cortex: Roles, Interventions and Traumas Niels Johnsen and Rolf Agerskov (Editors) 2009. ISBN: 978-1-60741-876-4 Cognitive Impairment: Causes, Diagnosis and Treatment Melanie L. Landow (Editor) 2009. ISBN: 978-1-60876-205-7 NEUROLOGY - LABORATORY AND CLINICAL RESEARCH DEVELOPMENTS COGNITIVE IMPAIRMENT: CAUSES, DIAGNOSIS AND TREATMENT MELANIE L. -

A Rare Case of Immune Reconstitution Inflammatory Syndrome Development in an Immunocompromised Patient with Progressive Multifocal Leukoencephalopathy And
Hindawi Publishing Corporation Case Reports in Neurological Medicine Volume 2013, Article ID 460701, 5 pages http://dx.doi.org/10.1155/2013/460701 Case Report A Rare Case of Immune Reconstitution Inflammatory Syndrome Development in an Immunocompromised Patient with Progressive Multifocal Leukoencephalopathy and Multicentric Castleman’s Disease Mohankumar Kurukumbi,1 Sheldon Steiner,1,2 Shariff Dunlap,1 Sherita Chapman,3 Noha Solieman,1 and Annapurni Jayam-Trouth1 1 Department of Neurology, Howard University Hospital, 2041 Georgia Avenue, Washington, DC 20060, USA 2 Department of Neurology, Howard University College of Medicine, Washington, DC 20060, USA 3 Department of Neurology, University of Virginia, Charlottesville, VA 22908, USA Correspondence should be addressed to Mohankumar Kurukumbi; [email protected] Received 27 June 2013; Accepted 17 July 2013 AcademicEditors:T.K.Banerjee,J.L.Gonzalez-Guti´ errez,´ R. Hashimoto, J. C. Kattah, and Y. Wakabayashi Copyright © 2013 Mohankumar Kurukumbi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Immune reconstitution inflammatory syndrome (IRIS) development in HIV with preexistent progressive multifocal leukoen- cephalopathy (PML) has been extensively studied. PML-IRIS typically manifests clinically as new or worsening neurologic symptoms in conjunction with enlarging CNS lesions and occurs in approximately 10–20 percent of HIV-infected patients with PML who begin HAART. Likewise, Multicentric Castleman’s Disease (MCD), a rare malignant lymphoproliferative disorder, has a strong and well-known association with HIV. Our case provides a rare instance of PML-IRIS in combination with MCD in an HIV-positive individual. -

Epilepsy Syndromes E9 (1)
EPILEPSY SYNDROMES E9 (1) Epilepsy Syndromes Last updated: September 9, 2021 CLASSIFICATION .......................................................................................................................................... 2 LOCALIZATION-RELATED (FOCAL) EPILEPSY SYNDROMES ........................................................................ 3 TEMPORAL LOBE EPILEPSY (TLE) ............................................................................................................... 3 Epidemiology ......................................................................................................................................... 3 Etiology, Pathology ................................................................................................................................ 3 Clinical Features ..................................................................................................................................... 7 Diagnosis ................................................................................................................................................ 8 Treatment ............................................................................................................................................. 15 EXTRATEMPORAL NEOCORTICAL EPILEPSY ............................................................................................... 16 Etiology ................................................................................................................................................ 16 -
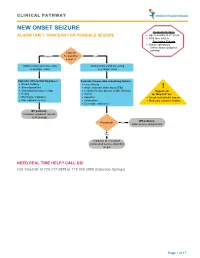
Seizure, New Onset
CLINICAL PATHWAY NEW ONSET SEIZURE Inclusion Criteria ALGORITHM 1. CONCERN FOR POSSIBLE SEIZURE • Age 6 months to 21 years • First-time seizure Exclusion Criteria • Status epilepticus (refer to status epilepticus pathway) Concern Unsure for possible Yes seizure? Obtain history and screening Obtain history and screening neurologic exam neurologic exam Consider differential diagnoses: Evaluate for possible provoking factors: • Breath holding • Fever/illness • Stereotypies/tics • Acute traumatic brain injury (TBI) ! • Vasovagal/syncope/vertigo • Central nervous system (CNS) infection Urgent call • Reflux • Tumor to ‘OneCall’ for: • Electrolyte imbalance • Ingestion • Suspected infantile spasm • Non epileptic seizure • Intoxication • Medically complex children • Electrolyte imbalance Off pathway: Consider outpatient referral to Neurology Off pathway: Provoked? Yes Address provoking factors No Continue to new onset unprovoked seizure algorithm on p.2 NEED REAL TIME HELP? CALL US! Call ‘OneCall’ at 720-777-3999 or 719-305-3999 (Colorado Springs) Page 1 of 17 CLINICAL PATHWAY ALGORITHM 2. NEW ONSET UNPROVOKED SEIZURE Inclusion Criteria • Age 6 months to 21 years New onset unprovoked • First-time unprovoked seizure seizure • Newly recognized seizure or epilepsy syndrome Exclusion Criteria • Provoked seizure: any seizure as a symptom of fever/illness, acute traumatic brain injury (TBI), Has central nervous system (CNS) infection, tumor, patient returned ingestion, intoxication, or electrolyte imbalance Consult inpatient • to baseline within No -

Myoclonic Atonic Epilepsy Another Generalized Epilepsy Syndrome That Is “Not So” Generalized
EDITORIAL Myoclonic atonic epilepsy Another generalized epilepsy syndrome that is “not so” generalized John M. Zempel, MD, Myoclonic atonic/astatic epilepsy (MAE), first described have shown predominant thalamic activation PhD well by Doose1 (pronounced dough sah: http://www. and default mode network deactivation.6–8 Even Tadaaki Mano, MD, PhD youtube.com/watch?v5hNNiWXV2wF0), is a general- Lennox-Gastaut syndrome, a devastating epileptic ized electroclinical syndrome with early onset charac- encephalopathy with EEG findings of runs of slow terized by myoclonic, atonic/astatic, generalized spike and wave and paroxysmal higher frequency Correspondence to tonic-clonic, and absence seizures (but not tonic activity, has fMRI correlates that are more focal than Dr. Zempel: [email protected] seizures) in association with generalized spike-wave expected in a syndrome with widespread EEG (GSW) discharges. Thought to have a genetic com- abnormalities.9,10 Neurology® 2014;82:1486–1487 ponent that has proven to be complicated,2 MAE EEG-fMRI is maturing as a research and clinical sometimes occurs in children who have otherwise technique. Recording scalp EEG in an electrically been developing normally and has variable outcome. hostile environment is not an easy task. Substantial MAE is typically treated with antiseizure medications technical artifacts, such as changing imaging gradients that are used for generalized epilepsy syndromes, with and ballistocardiogram (ECG-linked artifact observed perhaps a best response to valproate, felbamate, or the in the scalp electrodes), contaminate the EEG signal. ketogenic diet.3,4 However, the relatively distinctive EEG discharges in In this issue of Neurology®, Moeller et al.5 report patients with epilepsy have partially circumvented on the fMRI correlates of GSW discharges as mea- this problem. -
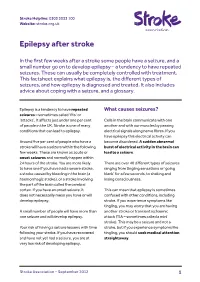
Epilepsy After Stroke
Stroke Helpline: 0303 3033 100 Website: stroke.org.uk Epilepsy after stroke In the first few weeks after a stroke some people have a seizure, and a small number go on to develop epilepsy – a tendency to have repeated seizures. These can usually be completely controlled with treatment. This factsheet explains what epilepsy is, the different types of seizures, and how epilepsy is diagnosed and treated. It also includes advice about coping with a seizure, and a glossary. Epilepsy is a tendency to have repeated What causes seizures? seizures – sometimes called ‘fits’ or ‘attacks’. It affects just under one per cent Cells in the brain communicate with one of people in the UK. Stroke is one of many another and with our muscles by passing conditions that can lead to epilepsy. electrical signals along nerve fibres. If you have epilepsy this electrical activity can Around five per cent of people who have a become disordered. A sudden abnormal stroke will have a seizure within the following burst of electrical activity in the brain can few weeks. These are known as acute or lead to a seizure. onset seizures and normally happen within 24 hours of the stroke. You are more likely There are over 40 different types of seizures to have one if you have had a severe stroke, ranging from tingling sensations or ‘going a stroke caused by bleeding in the brain (a blank’ for a few seconds, to shaking and haemorrhagic stroke), or a stroke involving losing consciousness. the part of the brain called the cerebral cortex. If you have an onset seizure, it This can mean that epilepsy is sometimes does not necessarily mean you have or will confused with other conditions, including develop epilepsy. -

“Seizures (Epilepsy)” a Seizure: Partial – Start in a Specific Part of the Brain, Not in the Whole � Is a Symptom of an Electrical Disturbance in the Brain Brain
“Seizures (Epilepsy)” A seizure: Partial – start in a specific part of the brain, not in the whole Is a symptom of an electrical disturbance in the brain brain. Unlike generalized seizures, partial seizures can have a Is a rare event warning before they occur (aura). Auras are actually a kind of Has a typical beginning (best clue for accurate diagnosis) seizure. There are several different kinds of partial seizures: Is involuntary simple (motor, sensory or psychological), complex, partial Lasts only a short time (90% complete in 90 seconds) seizure with secondary generalization. May cause post seizure impairments. Most seizures do not involve convulsions. Accurate seizure diagnosis by the health care provider is very The most common type of seizure is one mostly involving important because the medications used to treat seizures often vary loss of awareness. depending on the type. There are 20 types of seizures in the Seizures can be very subtle and hard to notice. International Classification of Seizures (over 2,000 types reported in the literature). Examples of post-seizure impairments: A detailed description of the seizure by the person observing the Post ictal confusion (length is individual) seizure is necessary for accurate diagnosing. Having a seizure while in Initial difficulty speaking the doctor’s office is very rare. Confusion about when, where, or what was just happening Memory disturbance which can last a while (behaving Seizure observation: - 3 important ones to make (in order of usual normally but can’t retain/absorb information) importance): Headache with some kinds of seizures What happened right as the seizure was beginning? What is epilepsy? What happened after the seizure was over? What happened during the seizure? Epilepsy is a condition where a person has “recurrent, unprovoked” seizures. -

Supplementary Table Term* Revised Term** Focal Seizure Without Impairment of a Subjective Sensory Or Psychic Experience As Part of Migraine Or Epilepsy
Supplementary table Term* Revised term** Focal seizure without impairment of A subjective sensory or psychic experience as part of migraine or epilepsy. In epilepsy it is a focal consciousness or awareness Aura seizure without loss of consciousness (a simple partial seizure). It may or may not be followed by involving subjective sensory or other seizure manifestations. psychic phenomena only Automatic behaviour associated with loss of awareness, such as lip smacking or hand wringing, Automatism Focal dyscognitive seizure occurring as part of a complex partial seizure. Convulsion (previously "grand Tonic-clonic seziure, convulsive Seizure with involuntary, irregular myoclonic, clonic or tonic–clonic movements of one or more mal") seizure limbs. Onset may be focal or primary generalised. Literally ‘already seen’, this refers to a false impression that a present experience is familiar. It is used to refer to something heard, experienced or seen. It can be the aura of a temporal lobe Déjà vu seizure, but also happens in other settings (normal experience, intoxication, migraine, psychiatric). Focal seizure (previously "partial, Focal seizure A seizure originating in a specific cortical location. May be due to a structural lesion. localization related") Literally a ‘blow’. Usually used for an epileptic seizure (but can refer to other paroxysmal events, Ictus such as migraine, transient neurological events and stroke). Similarly pre- and post-ictal are used may for the period before and after a seizure. Idiopathic Genetic In relation to epilepsy, this implies that there is an underlying genetic cause. Literally ‘never seen’, this refers to a false impression that a present experience is unfamiliar. It is Jamais vu used for something seen, heard or experienced. -

Multimodal Longitudinal Imaging of Focal Status Epilepticus
CASE REPORT Multimodal Longitudinal Imaging of Focal Status Epilepticus Colin P. Doherty, Andrew J. Cole, P. Ellen Grant, Alan Fischman, Elizabeth Dooling, Daniel B. Hoch, Tessa Hedley White, G. Rees Cosgrove ABSTRACT: Background: Little is understood about the evolution of structural and functional brain changes during the course of uncontrolled focal status epilepticus in humans. Methods: We serially evaluated and treated a nine-year-old girl with refractory focal status epilepticus. Long-term EEG monitoring, MRI, MRA, SPECT, intraoperative visualization of affected cortex, and neuropathological examination of a biopsy specimen were conducted over a three year time span. Imaging changes were correlated with simultaneous treatment and EEG findings. Results: The EEG monitoring showed almost continuous spike discharges emanating initially from the right frontocentral area. These EEG abnormalities were intermittently suppressed by treatment with anesthetics. Over time, additional brain areas developed epileptiform EEG abnormalities. Serial MRI studies demonstrated an evolution of changes from normal, through increased regional T2 signal to generalized atrophy. An MRAdemonstrated dilatation of the middle cerebral artery stem on the right compared to the left with a broad distribution of flow-related enhancement. An 18FDG-PET scan showed a dramatically abnormal metabolic profile in the same right frontocentral areas, which modulated in response to treatment during the course of the illness. A right frontotemporal craniotomy revealed a markedly hyperemic cortical focus including vascular shunting. A sample of resected cortex showed severe gliosis and neuronal death. Conclusions: The co-registration of structural and functional imaging and its correlation with operative and pathological findings in this case illustrates the relentless progression of regional and generalized abnormalities in intractable focal status epilepticus that were only transiently modified by exhaustive therapeutic interventions. -

Managing Children with Epilepsy School Nurse Guide
MANAGING CHILDREN WITH EPILEPSY SCHOOL NURSE GUIDE ACKNOWLEDGEMENTS TO THOSE WHO HAVE CONTRIBUTED TO THE NOTEBOOK Children’s Hospital of Orange County Melodie Balsbaugh, RN Sue Nagel, RN Giana Nguyen, CHOC Institutes Fullerton School District Jane Bockhacker, RN Orange Unified School District Andrea Bautista, RN Martha Boughen, RN Karen Hanson, RN TABLE OF CONTENTS I. EPILEPSY What is epilepsy? Facts about epilepsy Basic neuroanatomy overview Classification of epileptic seizures Diagnostic Tests II. TREATMENT Medications Vagus Nerve Stimulation Ketogenic Diet Surgery III. SAFETY First Aid IV. SPECIAL CONCERNS MedicAlert Helmets Driving Employment and the law V. EPILEPSY AT SCHOOL School epilepsy assessment tool Seizure record Teaching children about epilepsy lesson plan Creating your own individualized health care plan VI. RESOURCES/SUPPORT GROUPS VII. ACCESS TO HEALTHCARE CHOC Epilepsy Center After-Hours Care After Hours Health Care Advice Healthy Families California Kids MediCal CHOC Clinics Healthy Tomorrows VIII. REFERENCES EPILEPSY WHAT IS EPILEPSY? Epilepsy is a neurological disorder. The brain contains millions of nerve cells called neurons that send electrical charges to each other. A seizure occurs when there is a sudden and brief excess surge of electrical activity in the brain between nerve cells. This results in an alteration in sensation, behavior, and consciousness. Seizures may be caused by developmental problems before birth, trauma at birth, head injury, tumor, structural problems, vascular problems (i.e. stroke, abnormal blood vessels), metabolic conditions (i.e. low blood sugar, low calcium), infections (i.e. meningitis, encephalitis) and idiopathic causes. Children who have idiopathic seizures are most likely to respond to medications and outgrow seizures. -
“Top Neurology Cases” Ohsui.E
“Top Neurology Cases” OHSUi.e. Headache, etc. Doernbecher Annual Review DATE: October 3, 2019 BY: Kaitlin Greene, MD Director, Pediatric Headache OHSU Department of Pediatrics, Division of Pediatric Neurology Disclosures OHSU• None Outline: • Case 1: Headache • Case 2: Seizure • Case 3: Stroke OHSU• Discussion and Questions! 33 Case 1: Headache • Goals: • Review indications for imaging in patient presenting with headache • Review diagnostic criteria for migraine and migraine with aura in children and adolescents • Outline approach to acute and preventive treatment of headaches OHSU• Be comfortable prescribing a triptan! Case 1: Headache • 13 year old girl presenting with worsening headaches • When did headaches start? • Six months ago Age 8 • Short (~1 hour), infrequent (<1x/month), typically triggered by illness or dehydration, improved with ibuprofen • Over the past two years, frequency gradually increased to OHSU2x/month, then 4x/month, then to 2x/week by about 6 months ago Case 1: Headache • What are the headaches like? • Location: Mostly front, sometime back, sometimes more on one side or the other • Quality: Pressure (throbbing when severe) • Severity: Usually moderate, at least 2/month severe • What are the associated features • “Sensory sensitivity”: Light, sound, smell OHSU• Nausea when severe • Sees “flashes of light” for a few seconds with more severe headaches Itsoktobeweird.com Case 1: Headache • PMH: None • Family history: • Mom with “stress headaches” (Gets sensitive to light/noise, has to lie down) • Younger sister gets headaches when sick • Medications: • Ibuprofen 200 mg as needed for headache • Exam: Wt 50 kg. Normal including fundoscopic OHSUexam. Case 1: Headache - Diagnosis • What is the diagnosis? Migraine! With Aura? • BUT first have to answer two questions: 1.