Subcellular Expression of Maspin in Colorectal Cancer: Friend Or Foe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Deciphering the Functions of Ets2, Pten and P53 in Stromal Fibroblasts in Multiple
Deciphering the Functions of Ets2, Pten and p53 in Stromal Fibroblasts in Multiple Breast Cancer Models DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Julie Wallace Graduate Program in Molecular, Cellular and Developmental Biology The Ohio State University 2013 Dissertation Committee: Michael C. Ostrowski, PhD, Advisor Gustavo Leone, PhD Denis Guttridge, PhD Dawn Chandler, PhD Copyright by Julie Wallace 2013 Abstract Breast cancer is the second most common cancer in American women, and is also the second leading cause of cancer death in women. It is estimated that nearly a quarter of a million new cases of invasive breast cancer will be diagnosed in women in the United States this year, and approximately 40,000 of these women will die from breast cancer. Although death rates have been on the decline for the past decade, there is still much we need to learn about this disease to improve prevention, detection and treatment strategies. The majority of early studies have focused on the malignant tumor cells themselves, and much has been learned concerning mutations, amplifications and other genetic and epigenetic alterations of these cells. However more recent work has acknowledged the strong influence of tumor stroma on the initiation, progression and recurrence of cancer. Under normal conditions this stroma has been shown to have protective effects against tumorigenesis, however the transformation of tumor cells manipulates this surrounding environment to actually promote malignancy. Fibroblasts in particular make up a significant portion of this stroma, and have been shown to impact various aspects of tumor cell biology. -

Genetic Basis of Simple and Complex Traits with Relevance to Avian Evolution
Genetic basis of simple and complex traits with relevance to avian evolution Małgorzata Anna Gazda Doctoral Program in Biodiversity, Genetics and Evolution D Faculdade de Ciências da Universidade do Porto 2019 Supervisor Miguel Jorge Pinto Carneiro, Auxiliary Researcher, CIBIO/InBIO, Laboratório Associado, Universidade do Porto Co-supervisor Ricardo Lopes, CIBIO/InBIO Leif Andersson, Uppsala University FCUP Genetic basis of avian traits Nota Previa Na elaboração desta tese, e nos termos do número 2 do Artigo 4º do Regulamento Geral dos Terceiros Ciclos de Estudos da Universidade do Porto e do Artigo 31º do D.L.74/2006, de 24 de Março, com a nova redação introduzida pelo D.L. 230/2009, de 14 de Setembro, foi efetuado o aproveitamento total de um conjunto coerente de trabalhos de investigação já publicados ou submetidos para publicação em revistas internacionais indexadas e com arbitragem científica, os quais integram alguns dos capítulos da presente tese. Tendo em conta que os referidos trabalhos foram realizados com a colaboração de outros autores, o candidato esclarece que, em todos eles, participou ativamente na sua conceção, na obtenção, análise e discussão de resultados, bem como na elaboração da sua forma publicada. Este trabalho foi apoiado pela Fundação para a Ciência e Tecnologia (FCT) através da atribuição de uma bolsa de doutoramento (PD/BD/114042/2015) no âmbito do programa doutoral em Biodiversidade, Genética e Evolução (BIODIV). 2 FCUP Genetic basis of avian traits Acknowledgements Firstly, I would like to thank to my all supervisors Miguel Carneiro, Ricardo Lopes and Leif Andersson, for the demanding task of supervising myself last four years. -

Biogenesis and Maintenance of Cytoplasmic Domains in Myelin of the Central Nervous System
Biogenesis and Maintenance of Cytoplasmic Domains in Myelin of the Central Nervous System Dissertation for the award of the degree “Doctor rerum naturalium” of the Georg-August-Universität Göttingen within the doctoral program Molecular Biology of Cells of the Georg-August University School of Science (GAUSS) submitted by Caroline Julia Velte from Usingen, Germany Göttingen 2016 Members of the Thesis Committee: Prof. Dr. Mikael Simons, Reviewer Max Planck Institute of Experimental Medicine, Göttingen Prof. Dr. Andreas Janshoff, Reviewer Georg-August University, Göttingen Prof. Dr. Dirk Görlich Max Planck Institute of Biophysical Chemistry, Göttingen Date of the thesis defense: 27th of June 2016 Don't part with your illusions. When they are gone, you may still exist, but you have ceased to live. (Mark Twain) III Affidavit I hereby declare that my PhD thesis “Biogenesis and Maintenance of Cytoplasmic Domains in Myelin of the Central Nervous System” has been written independently with no other aids or sources than quoted. Furthermore, I confirm that this thesis has not been submitted as part of another examination process neither in identical nor in similar form. Caroline Julia Velte April 2016 Göttingen, Germany V Publications Nicolas Snaidero*, Caroline Velte*, Matti Myllykoski, Arne Raasakka, Alexander Ignatev, Hauke B. Werner, Michelle S. Erwig, Wiebke Moebius, Petri Kursula, Klaus-Armin Nave, and Mikael Simons Antagonistic Functions of MBP and CNP Establish Cytosolic Channels in CNS Myelin, Cell Reports 18 *equal contribution (January 2017) E. d’Este, D. Kamin, C. Velte, F. Göttfert, M. Simons, S.W. Hell Subcortical cytoskeleton periodicity throughout the nervous system, Scientific Reports 6 (March 2016) K.A. -

SERPINB3/4 Polyclonal Antibody
PRODUCT DATA SHEET Bioworld Technology,Inc. SERPINB3/4 polyclonal antibody Catalog: BS60990 Host: Rabbit Reactivity: Human,Mouse,Rat BackGround: Swiss-Prot: Metastasis of a primary tumor to a distant site is deter- P29508/P48594 mined through signaling cascades that break down inter- Purification&Purity: actions between the cell and extracellular matrix proteins. The antibody was affinity-purified from rabbit antiserum Among the proteins mediating metastasis are serine by affinity-chromatography using epitope-specific im- prote-ases, such as neutrophil elastase. In 1985, Dr. Jim munogen and the purity is > 95% (by SDS-PAGE). Travis and Dr. R.W. Carrell designated an emerging fam- Applications: ily of serine protease inhibitors as the serpin fam-ily, WB: 1:500~1:1000 which share homology in both primary amino acid se- Storage&Stability: quence and tertiary structure. Serpins contain a stretch of Store at 4°C short term. Aliquot and store at -20°C long peptide that mimics a true substrate for a corresponding term. Avoid freeze-thaw cycles. serine protease. Serine proteases bind to this substrate Specificity: mimic in a 1:1 stoichiometric fashion and become cata- SERPINB3/4 polyclonal antibody detects endogenous lytically inactive. Aberrant ex-pression of serpin family levels of SERPINB3/4 protein. members can contribute to a number of conditions, in- DATA: cluding emphysema (a-1 antitrypsin deficiency), fatal bleeding (elastase to thrombin specificity) and thrombosis (antithrombin deficiency), and are indicators of cancer stage phenotypes (circulating levels of squamous cell car- cinoma antigen, known as SCCA1, increase in advancing stages of some cervical, lung, esophageal and head and neck cancers). -

A General Binding Mechanism for All Human Sulfatases by the Formylglycine-Generating Enzyme
A general binding mechanism for all human sulfatases by the formylglycine-generating enzyme Dirk Roeser*, Andrea Preusser-Kunze†, Bernhard Schmidt†, Kathrin Gasow*, Julia G. Wittmann*, Thomas Dierks‡, Kurt von Figura†, and Markus Georg Rudolph*§ *Department of Molecular Structural Biology, University of Go¨ttingen, Justus-von-Liebig-Weg 11, D-37077 Go¨ttingen, Germany; †Department of Biochemistry II, Heinrich-Du¨ker-Weg 12, University of Go¨ttingen, D-37073 Go¨ttingen, Germany; and ‡Department of Biochemistry I, Universita¨tsstrasse 25, University of Bielefeld, D-33615 Bielefeld, Germany Edited by Carolyn R. Bertozzi, University of California, Berkeley, CA, and approved November 8, 2005 (received for review September 1, 2005) The formylglycine (FGly)-generating enzyme (FGE) uses molecular tases, suggesting a general binding mechanism of substrate sulfa- oxygen to oxidize a conserved cysteine residue in all eukaryotic tases by FGE. sulfatases to the catalytically active FGly. Sulfatases degrade and The details of how O2-dependent cysteine oxidation is mediated remodel sulfate esters, and inactivity of FGE results in multiple by FGE are unknown. As a first step toward the elucidation of the sulfatase deficiency, a fatal disease. The previously determined FGE molecular mechanism of FGly formation, we have previously crystal structure revealed two crucial cysteine residues in the active determined crystal structures of FGE in various oxidation states site, one of which was thought to be implicated in substrate (8). FGE adopts a novel fold with surprisingly little regular sec- 2ϩ binding. The other cysteine residue partakes in a novel oxygenase ondary structure and contains two structural Ca ions and two mechanism that does not rely on any cofactors. -

Tissue-Type Plasminogen Activator Is a Target of the Tumor Suppressor Gene Maspin
Proc. Natl. Acad. Sci. USA Vol. 95, pp. 499–504, January 1998 Biochemistry Tissue-type plasminogen activator is a target of the tumor suppressor gene maspin SHIJIE SHENG*†,BINH TRUONG*, DEREK FREDRICKSON*, RUILIAN WU*, ARTHUR B. PARDEE‡, AND RUTH SAGER* *Division of Cancer Genetics and ‡Division of Cell Growth and Regulation, Dana–Farber Cancer Institute, Harvard Medical School, 44 Binney Street, Boston, MA 02115 Contributed by Arthur B. Pardee, November 10, 1997§ ABSTRACT The maspin protein has tumor suppressor that PAI-1 also inhibits cell motility via an integrin-mediated activity in breast and prostate cancers. It inhibits cell motility pathway by its interaction with cell surface-bound uPA and and invasion in vitro and tumor growth and metastasis in nude vitronectin (8, 9). mice. Maspin is structurally a member of the serpin (serine The RSL of maspin is shorter than that of other serpins (1), protease inhibitors) superfamily but deviates somewhat from casting doubt on its ability to act as a classical inhibitory serpin. classical serpins. We find that single-chain tissue plasmino- Pemberton et al. (10) reported that purified rMaspin(i) is a gen activator (sctPA) specifically interacts with the maspin substrate instead of an inhibitor to an array of serine proteases, reactive site loop peptide and forms a stable complex with including uPA and tissue-type plasminogen activator (tPA). recombinant maspin [rMaspin(i)]. Major effects of rMas- However, our evidence that the RSL is crucial for the biolog- pin(i) are observed on plasminogen activation by sctPA. First, ical activity of maspin would be consistent with maspin acting rMaspin(i) activates free sctPA. -

The Surface of Prostate Carcinoma DU145 Cells Mediates the Inhibition of Urokinase-Type Plasminogen Activator by Maspin1
[CANCER RESEARCH 60, 4771–4778, September 1, 2000] The Surface of Prostate Carcinoma DU145 Cells Mediates the Inhibition of Urokinase-type Plasminogen Activator by Maspin1 Richard McGowen, Hector Biliran, Jr., Ruth Sager,2 and Shijie Sheng3 Department of Pathology, Wayne State University School of Medicine, Detroit, Michigan 48201 [R. M., H. B., S. S.], and Division of Cancer Genetics, Dana-Farber Cancer Institute, Boston, Massachusetts 02115 [R. S.] ABSTRACT relation between maspin expression and the progression of breast cancer (1, 4). In addition, maspin expression is down-regulated in Maspin is a novel serine protease inhibitor (serpin) with tumor prostate carcinoma cells compared with that in immortalized normal suppressive potential in breast and prostate cancer, acting at the level of tumor invasion and metastasis. It was subsequently demonstrated prostate epithelial cells (5, 6). that maspin inhibits tumor invasion, at least in part, by inhibiting cell Biological studies demonstrate a tumor-suppressive role of maspin, motility. Interestingly, in cell-free solutions, maspin does not inhibit acting at the levels of tumor invasion and metastases. Mammary several serine proteases including tissue-type plasminogen activator carcinoma MDA-MB-435 cells transfected with maspin cDNA are and urokinase-type plasminogen activator (uPA). Despite the recent significantly inhibited in invasion and motility assays in vitro and are biochemical evidence that maspin specifically inhibits tissue-type plas- inhibited in tumor growth and metastasis in nude mice (1, 5, 7). It has minogen activator that is associated with fibrinogen or poly-L-lysine, been shown independently that induction of maspin expression in four the molecular mechanism underlying the tumor-suppressive effect of different breast tumor cell lines by ␥-linolenic acid dramatically maspin remains elusive. -

Adaptive Evolution and Divergence of SERPINB3: a Young Duplicate in Great Apes
Adaptive Evolution and Divergence of SERPINB3: A Young Duplicate in Great Apes Sı´lvia Gomes1*, Patrı´cia I. Marques1,2, Rune Matthiesen3, Susana Seixas1* 1 Institute of Molecular Pathology and Immunology of the University of Porto (IPATIMUP), Porto, Portugal, 2 Institute of Biomedical Sciences Abel Salazar (ICBAS), University of Porto, Porto, Portugal, 3 National Health Institute Doutor Ricardo Jorge (INSA), Lisboa, Portugal Abstract A series of duplication events led to an expansion of clade B Serine Protease Inhibitors (SERPIN), currently displaying a large repertoire of functions in vertebrates. Accordingly, the recent duplicates SERPINB3 and B4 located in human 18q21.3 SERPIN cluster control the activity of different cysteine and serine proteases, respectively. Here, we aim to assess SERPINB3 and B4 coevolution with their target proteases in order to understand the evolutionary forces shaping the accelerated divergence of these duplicates. Phylogenetic analysis of primate sequences placed the duplication event in a Hominoidae ancestor (,30 Mya) and the emergence of SERPINB3 in Homininae (,9 Mya). We detected evidence of strong positive selection throughout SERPINB4/B3 primate tree and target proteases, cathepsin L2 (CTSL2) and G (CTSG) and chymase (CMA1). Specifically, in the Homininae clade a perfect match was observed between the adaptive evolution of SERPINB3 and cathepsin S (CTSS) and most of sites under positive selection were located at the inhibitor/protease interface. Altogether our results seem to favour a coevolution hypothesis for SERPINB3, CTSS and CTSL2 and for SERPINB4 and CTSG and CMA1.A scenario of an accelerated evolution driven by host-pathogen interactions is also possible since SERPINB3/B4 are potent inhibitors of exogenous proteases, released by infectious agents. -

Pso P27, a SERPINB3/B4-Derived Protein, Is Most Likely a Common Autoantigen in Chronic Inflammatory Diseases
Clinical Immunology 174 (2017) 10–17 Contents lists available at ScienceDirect Clinical Immunology journal homepage: www.elsevier.com/locate/yclim Pso p27, a SERPINB3/B4-derived protein, is most likely a common autoantigen in chronic inflammatory diseases Ole-Jan Iversen a,⁎,HildeLysvanda, Geir Slupphaug b a Department of Laboratory Medicine, Children's and Women's Health, Faculty of Medicine, Norwegian University of Science and Technology, NTNU, Trondheim, Norway b Department of Cancer Research and Molecular Medicine, Faculty of Medicine and PROMEC Core Facility for Proteomics and Metabolomics, Norwegian University of Science and Technology, NTNU, Trondheim, Norway article info abstract Article history: Autoimmune diseases are characterized by chronic inflammatory reactions localized to an organ or organ- Received 17 October 2016 system. They are caused by loss of immunologic tolerance toward self-antigens, causing formation of autoanti- Received in revised form 1 November 2016 bodies that mistakenly attack their own body. Psoriasis is a chronic inflammatory autoimmune skin disease in accepted with revision 13 November 2016 which the underlying molecular mechanisms remain elusive. In this review, we present evidence accumulated Available online 15 November 2016 through more than three decades that the serpin-derived protein Pso p27 is an autoantigen in psoriasis and prob- ably also in other chronic inflammatory diseases. Keywords: Autoimmune diseases Pso p27 is derived from the serpin molecules SERPINB3 and SERPINB4 through non-canonical cleavage by mast Pso p27 cell chymase. In psoriasis, it is exclusively found in skin lesions and not in uninvolved skin. The serpins are cleaved SERPINB3/B4 into three fragments that remain associated as a Pso p27 complex with novel immunogenic properties and in- Mast cells creased tendency to form large aggregates compared to native SERPINB3/B4. -

Re-Activation of a Dormant Tumor Suppressor Gene Maspin by Designed Transcription Factors
Oncogene (2007) 26, 2791–2798 & 2007 Nature Publishing Group All rights reserved 0950-9232/07 $30.00 www.nature.com/onc SHORT COMMUNICATION Re-activation of a dormant tumor suppressor gene maspin by designed transcription factors A Beltran1, S Parikh1, Y Liu1, BD Cuevas1, GL Johnson1, BW Futscher2 and P Blancafort1 1Department of Pharmacology and the Lineberger Comprehensive Cancer Center, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA and 2Department of Pharmacology and Toxicology, Arizona Cancer Center and College of Pharmacy, University of Arizona, Tucson, AZ, USA The controlled and specific re-activation of endogenous Tumor progression is a dynamic process controlled by tumor suppressors in cancer cells represents an important multiple genetic factors, including oncogenes, which therapeutic strategy to block tumor growth and subse- facilitate tumor growth, and tumor suppressors, which quent progression. Other than ectopic delivery of tumor negatively regulate tumor growth and progression. Since suppressor-encoded cDNA, there are no therapeutic tools the discovery of the tumor suppressor p53, more than 15 able to specifically re-activate tumor suppressor genes that different tumor suppressor genes have been identified are silenced in tumor cells. Herein, we describe a novel (Sherr, 2003; McGarvey et al., 2006). The expression of approach to specifically regulate dormant tumor sup- tumor suppressors is downregulated in tumor cells by pressors in aggressive cancer cells. We have targeted means of genetic and epigenetic mechanisms (Baylin, the Mammary Serine Protease Inhibitor (maspin) 2005; Zardo et al., 2005). Given the importance of (SERPINB5) tumor suppressor, which is silenced by tumor suppressors in controlling primary tumor growth, transcriptionaland aberrant promoter methylation in many therapeutic strategies aim to restore their expres- aggressive epithelial tumors. -
Supplementary File 2A Revised
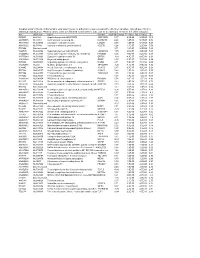
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -

Lysosomal Hydrolases: Conversion of Acidic to Basic Forms by Neuraminidase
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Volume 13, number 1 FEBS LETTERS February 1971 LYSOSOMAL HYDROLASES: CONVERSION OF ACIDIC TO BASIC FORMS BY NEURAMINIDASE Alfred GOLDSTONE, Philip KONECNY and Harold KOENIG Neurology Service, VA Research Hospital; and Departments of Neurology and Biochemistry, Northwestern University Medical School, Chicago, Illinois, USA Received 21 December 1970 1. Introduction intervals to avoid overheating). The lysosomal lysate was ultracentrifuged at 100,000 g for 30 min to give A number of hydrolytic enzymes of lysosomal a soluble enzyme fraction. This fraction also contains origin occur in multiple forms which differ in such an acidic lipoprotein [4]. The insoluble residue was physicochemical properties as solubility, heat and pH suspended in 0.05 M acetate buffer pH 5.0 with 0.2% stability, pH optima and electrophoretic mobility [I]. Triton X-100 and resonicated to release the bound ly- Recent studies in this laboratory indicate that essen- sosomal enzymes together with additional acidic lipo- tially all the enzyme proteins of rat kidney and liver protein ([4] and A. Goldstone and H. Koenig, unpu- lysosomes are glycoproteins, and that at least some of blished observations). All operations were carried out these glycoproteins contain sialic acid [2-41. The at 4’. acidic form of lysosomal N-acetylhexosaminidase from Aliquots of the soluble fraction containing about human spleen [ 51 and kidney [6] is converted into 2 mg of protein were incubated with neuraminidase the basic form by treatment with neuraminidase. We from Cl. perfringens (Type Vl enzyme supplied by now confirm this finding for rat kidney and show Sigma), 0.1 mg/ml, or V.