HIF-1A Regulates IL-1B and IL-17 in Sarcoidosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review the Significance of Interleukin-6
Review The significance of interleukin-6 and C-reactive protein in systemic sclerosis: a systematic literature review C. Muangchan1,2,3, J.E. Pope2 1Research Fellow, Rheumatology; ABSTRACT Introduction 2Schulich School of Medicine & Dentistry, Objectives. Interleukin-6 (IL-6) may Systemic sclerosis (SSc) or scleroder- Western University of Canada (formerly play a role in the pathogenesis of SSc. ma is a systemic autoimmune rheumat- University of Western Ontario), St Joseph C-reactive protein (CRP), an acute ic disease characterised by autoimmun- Health Care, London, ON; 3Division of Rheumatology, Department of phase reactant induced by IL-6, may be ity; fibrosis and dysfunction in vascular Medicine, Faculty of Medicine, Mahidol a prognostic marker in SSc. The goal of regulatory mechanisms highlighted by University, Siriraj Hospital, Bangkok, this systematic review was to address vasculopathy of microcirculation (1). Thailand. the significance and clinical applica- SSc has increased extracellular matrix Chayawee Muangchan, Research Fellow tion of IL-6 and CRP in systemic scle- protein deposition due to increased fi- Janet Elizabeth Pope, MD rosis (SSc). broblast biosynthetic activity (2). SSc is Please address correspondence Methods. A literature search was con- rare and has a female predisposition (3, and reprint requests to: ducted to identify English-language 4). It is classified into diffuse cutane- Dr Janet Pope, original articles within PubMed, Sco- ous SSc (dcSSc) and limited cutaneous St. Joseph’s Health Care, London, SSc (lcSSc) subsets according to extent 268 Grosvenor St., pus, and Medline database from incep- London N6A 4V2, ON, Canada. tion to May 30, 2013 using keywords of cutaneous involvement (5). -

Chronic Mtor Activation Induces a Degradative Smooth Muscle Cell Phenotype
The Journal of Clinical Investigation RESEARCH ARTICLE Chronic mTOR activation induces a degradative smooth muscle cell phenotype Guangxin Li,1,2 Mo Wang,1 Alexander W. Caulk,3 Nicholas A. Cilfone,4 Sharvari Gujja,4 Lingfeng Qin,1 Pei-Yu Chen,5 Zehua Chen,4 Sameh Yousef,1 Yang Jiao,1 Changshun He,1 Bo Jiang,1 Arina Korneva,3 Matthew R. Bersi,3 Guilin Wang,6 Xinran Liu,7,8 Sameet Mehta,9 Arnar Geirsson,1,10 Jeffrey R. Gulcher,4 Thomas W. Chittenden,4 Michael Simons,5,10 Jay D. Humphrey,3,10 and George Tellides1,10,11 1Department of Surgery, Yale School of Medicine, New Haven, Connecticut, USA. 2Department of Breast and Thyroid Surgery, Peking University Shenzhen Hospital, Shenzhen, Guangdong Province, China. 3Department of Biomedical Engineering, Yale School of Engineering and Applied Science, New Haven, Connecticut, USA. 4Computational Statistics and Bioinformatics Group, Advanced Artificial Intelligence Research Laboratory, WuXi NextCODE, Cambridge, Massachusetts, USA. 5Internal Medicine, 6Molecular Biophysics and Biochemistry, and 7Cell Biology, Yale School of Medicine, New Haven, Connecticut, USA. 8Center for Cellular and Molecular Imaging, EM Core Facility, Yale School of Medicine, New Haven, Connecticut, USA. 9Genetics and 10Program in Vascular Biology and Therapeutics, Yale School of Medicine, New Haven, Connecticut, USA. 11Veterans Affairs Connecticut Healthcare System, West Haven, Connecticut, USA. Smooth muscle cell (SMC) proliferation has been thought to limit the progression of thoracic aortic aneurysm and dissection (TAAD) because loss of medial cells associates with advanced disease. We investigated effects of SMC proliferation in the aortic media by conditional disruption of Tsc1, which hyperactivates mTOR complex 1. -

The Regulation of Interleukin 7 Receptor Alpha Internalization, Recycling and Degradation by IL-7
Universidade de Lisboa Faculdade de Medicina Unidade de Biologia do Cancro, Instituto de Medicina Molecular The regulation of Interleukin 7 receptor alpha internalization, recycling and degradation by IL-7 - Possible implications in T-cell homeostasis, migration and leukaemogenesis - Catarina Martins de Oliveira Henriques Doutoramento em Ciências Biomédicas For the degree of Doctor of Philosophy 2009 Universidade de Lisboa Faculdade de Medicina Unidade de Biologia do Cancro, Instituto de Medicina Molecular The regulation of Interleukin 7 receptor alpha internalization, recycling and degradation by IL-7 - Possible implications in T-cell homeostasis, migration and leukaemogenesis - Catarina Martins de Oliveira Henriques (Recipient of a scholarship- SFRH7BD/21940/2005 from Fundação para a Ciência e Tecnologia) Tese orientada pelo Doutor João T. Barata, Prof Doutor.Gerard Graham e Prof. Doutora Leonor Parreira Doutoramento em Ciências Biomédicas, especialidade em Ciências Biopatológicas For the degree of Doctor of Philosophy 2009 As opiniões expressas são da exclusiva responsabilidade do seu autor A impressão desta dissertação foi aprovada pela Comissão Coordenadora do Conselho Científico da Faculdade de Medicina de Lisboa em reunião de 13 de Outubro de 2009. Para a Prof. Filomena Mota. Sem o seu apoio e inspiração há muitos anos atrás, eu não seria hoje uma bióloga nem esta tese teria alguma vez existido… Table of Contents Table of contents……………………………………………………….………………….................. i Aknowledgements……………………………………………………………………………………………. -
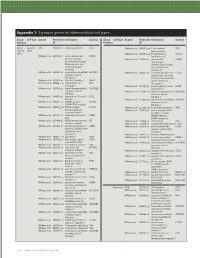
Technical Note, Appendix: an Analysis of Blood Processing Methods to Prepare Samples for Genechip® Expression Profiling (Pdf, 1
Appendix 1: Signature genes for different blood cell types. Blood Cell Type Source Probe Set Description Symbol Blood Cell Type Source Probe Set Description Symbol Fraction ID Fraction ID Mono- Lympho- GSK 203547_at CD4 antigen (p55) CD4 Whitney et al. 209813_x_at T cell receptor TRG nuclear cytes gamma locus cells Whitney et al. 209995_s_at T-cell leukemia/ TCL1A Whitney et al. 203104_at colony stimulating CSF1R lymphoma 1A factor 1 receptor, Whitney et al. 210164_at granzyme B GZMB formerly McDonough (granzyme 2, feline sarcoma viral cytotoxic T-lymphocyte- (v-fms) oncogene associated serine homolog esterase 1) Whitney et al. 203290_at major histocompatibility HLA-DQA1 Whitney et al. 210321_at similar to granzyme B CTLA1 complex, class II, (granzyme 2, cytotoxic DQ alpha 1 T-lymphocyte-associated Whitney et al. 203413_at NEL-like 2 (chicken) NELL2 serine esterase 1) Whitney et al. 203828_s_at natural killer cell NK4 (H. sapiens) transcript 4 Whitney et al. 212827_at immunoglobulin heavy IGHM Whitney et al. 203932_at major histocompatibility HLA-DMB constant mu complex, class II, Whitney et al. 212998_x_at major histocompatibility HLA-DQB1 DM beta complex, class II, Whitney et al. 204655_at chemokine (C-C motif) CCL5 DQ beta 1 ligand 5 Whitney et al. 212999_x_at major histocompatibility HLA-DQB Whitney et al. 204661_at CDW52 antigen CDW52 complex, class II, (CAMPATH-1 antigen) DQ beta 1 Whitney et al. 205049_s_at CD79A antigen CD79A Whitney et al. 213193_x_at T cell receptor beta locus TRB (immunoglobulin- Whitney et al. 213425_at Homo sapiens cDNA associated alpha) FLJ11441 fis, clone Whitney et al. 205291_at interleukin 2 receptor, IL2RB HEMBA1001323, beta mRNA sequence Whitney et al. -
Lysosomal Membrane Glycoproteins Bind Cholesterol and Contribute to Lysosomal Cholesterol Export
1 Lysosomal membrane glycoproteins bind cholesterol and 2 contribute to lysosomal cholesterol export 3 4 Jian Li and Suzanne R. Pfeffer* 5 Department of Biochemistry, Stanford University School of Medicine 6 Stanford, CA USA 94305-5307 7 8 *Correspondence to: [email protected]. 9 10 Abstract: LAMP1 and LAMP2 proteins are highly abundant, ubiquitous, mammalian proteins 11 that line the lysosome limiting membrane, and protect it from lysosomal hydrolase action. 12 LAMP2 deficiency causes Danon’s disease, an X-linked hypertrophic cardiomyopathy. LAMP2 13 is needed for chaperone-mediated autophagy, and its expression improves tissue function in 14 models of aging. We show here that LAMP1 and LAMP2 bind cholesterol in a manner that 15 buries the cholesterol 3β-hydroxyl group; they also bind tightly to NPC1 and NPC2 proteins that 16 export cholesterol from lysosomes. Quantitation of cellular LAMP2 and NPC1 protein levels 17 suggest that LAMP proteins represent a significant cholesterol binding site at the lysosome 18 limiting membrane, and may signal cholesterol availability. Functional rescue experiments show 19 that the ability of LAMP2 to facilitate cholesterol export from lysosomes relies on its ability to 20 bind cholesterol directly. 21 22 23 Introduction 24 Eukaryotic lysosomes are acidic, membrane-bound organelles that contain proteases, lipases and 25 nucleases and degrade cellular components to regenerate catabolic precursors for cellular use (1- 26 3). Lysosomes are crucial for the degradation of substrates from the cytoplasm, as well as 27 membrane bound compartments derived from the secretory, endocytic, autophagic and 28 phagocytic pathways. The limiting membrane of lysosomes is lined with so-called lysosomal 29 membrane glycoproteins (LAMPs) that are comprised of a short cytoplasmic domain, a single 30 transmembrane span, and a highly, N- and O-glycosylated lumenal domain (4-6). -

Sensitization to the Lysosomal Cell Death Pathway by Oncogene- Induced Down-Regulation of Lysosome-Associated Membrane Proteins 1 and 2
Research Article Sensitization to the Lysosomal Cell Death Pathway by Oncogene- Induced Down-regulation of Lysosome-Associated Membrane Proteins 1 and 2 Nicole Fehrenbacher,1 Lone Bastholm,2 Thomas Kirkegaard-Sørensen,1 Bo Rafn,1 Trine Bøttzauw,1 Christina Nielsen,1 Ekkehard Weber,3 Senji Shirasawa,4 Tuula Kallunki,1 and Marja Ja¨a¨ttela¨1 1Apoptosis Department and Centre for Genotoxic Stress Response, Institute for Cancer Biology, Danish Cancer Society; 2Institute of Molecular Pathology, Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark; 3Institute of Physiological Chemistry, Medical Faculty, Martin-Luther-University Halle-Wittenberg, Halle, Germany; and 4Department of Cell Biology, School of Medicine, Fukuoka University, Fukuoka, Japan Abstract molecules of the cell to breakdown products available for Expression and activity of lysosomal cysteine cathepsins metabolic reuse (3, 4). Cathepsin proteases are among the best- correlate with the metastatic capacity and aggressiveness of studied lysosomal hydrolases. They are maximally active at the tumors. Here, we show that transformation of murine acidic pH of lysosomes (pH 4–5). However, many of them can be Y527F embryonic fibroblasts with v-H-ras or c-src changes the active at the neutral pH outside lysosomes, albeit with a decreased distribution, density, and ultrastructure of the lysosomes, efficacy and/or altered specificity (5). For example, transformation and tumor environment enhance the expression of lysosomal decreases the levels of lysosome-associated membrane pro- teins (LAMP-1 and LAMP-2) in an extracellular signal- cysteine cathepsins and increase their secretion into the extracel- regulated kinase (ERK)- and cathepsin-dependent manner, lular space (6). Once outside the tumor cells, cathepsins stimulate and sensitizes the cells to lysosomal cell death pathways angiogenesis, tumor growth, and invasion in murine cancer induced by various anticancer drugs (i.e., cisplatin, etoposide, models, thereby enhancing cancer progression (7, 8). -

Abnormal Lysosomal Trafficking and Enhanced Exosomal Export of Cisplatin in Drug-Resistant Human Ovarian Carcinoma Cells
1595 Abnormal lysosomal trafficking and enhanced exosomal export of cisplatin in drug-resistant human ovarian carcinoma cells Roohangiz Safaei, Barrett J. Larson, of human ovarian carcinoma cells selected for stable Timothy C. Cheng, Michael A. Gibson, resistance to CDDP is markedly reduced in size, and that Shinji Otani, Wiltrud Naerdemann, these cells abnormally sort some lysosomal proteins and Stephen B. Howell and the putative CDDP transporters into an exosomal pathway that also exports CDDP. [Mol Cancer Ther 2005; Rebecca and John Moore University of California at San Diego 4(10):1595–604] Cancer Center, University of California at San Diego, La Jolla, California Introduction Repeated exposure of tumor cells to cisplatin (CDDP) Abstract results in rapid development of resistance, which eventu- Previous work has shown that cisplatin (CDDP) becomes ally contributes to therapeutic failure (1). Resistance to concentrated in lysosomes, and that acquired resistance CDDP is often accompanied by resistance to metalloids to CDDP is associated with abnormalities of protein and is associated with alterations in DNA repair (2), thiol trafficking and secretion. The lysosomal compartment in content (3), and drug accumulation (4). Recent studies have CDDP-sensitive 2008 human ovarian carcinoma cells was linked the expression of several transporters, particularly compared with that in CDDP-resistant 2008/C13*5.25 the copper export proteins ATP7A and ATP7B, with CDDP subline using deconvoluting imaging and specific dyes and resistance and suggest that they play a direct role in the antibodies. The lysosomal compartment in CDDP-resistant efflux of CDDP (5). cells was reduced to just 40% of that in the parental In tumor cells, CDDP accumulates in a variety of vesic- CDDP-sensitive cells (P < 0.002). -

Protein Network Analyses of Pulmonary Endothelial Cells In
www.nature.com/scientificreports OPEN Protein network analyses of pulmonary endothelial cells in chronic thromboembolic pulmonary hypertension Sarath Babu Nukala1,8,9*, Olga Tura‑Ceide3,4,5,9, Giancarlo Aldini1, Valérie F. E. D. Smolders2,3, Isabel Blanco3,4, Victor I. Peinado3,4, Manuel Castell6, Joan Albert Barber3,4, Alessandra Altomare1, Giovanna Baron1, Marina Carini1, Marta Cascante2,7,9 & Alfonsina D’Amato1,9* Chronic thromboembolic pulmonary hypertension (CTEPH) is a vascular disease characterized by the presence of organized thromboembolic material in pulmonary arteries leading to increased vascular resistance, heart failure and death. Dysfunction of endothelial cells is involved in CTEPH. The present study describes for the frst time the molecular processes underlying endothelial dysfunction in the development of the CTEPH. The advanced analytical approach and the protein network analyses of patient derived CTEPH endothelial cells allowed the quantitation of 3258 proteins. The 673 diferentially regulated proteins were associated with functional and disease protein network modules. The protein network analyses resulted in the characterization of dysregulated pathways associated with endothelial dysfunction, such as mitochondrial dysfunction, oxidative phosphorylation, sirtuin signaling, infammatory response, oxidative stress and fatty acid metabolism related pathways. In addition, the quantifcation of advanced oxidation protein products, total protein carbonyl content, and intracellular reactive oxygen species resulted increased -
Reprogramming of Lysosomal Gene Expression by Interleukin-4 and Stat6 Brignull Et Al
Reprogramming of lysosomal gene expression by interleukin-4 and Stat6 Brignull et al. Brignull et al. BMC Genomics 2013, 14:853 http://www.biomedcentral.com/1471-2164/14/853 Brignull et al. BMC Genomics 2013, 14:853 http://www.biomedcentral.com/1471-2164/14/853 RESEARCH ARTICLE Open Access Reprogramming of lysosomal gene expression by interleukin-4 and Stat6 Louise M Brignull1†, Zsolt Czimmerer2†, Hafida Saidi1,3, Bence Daniel2, Izabel Villela4,5, Nathan W Bartlett6, Sebastian L Johnston6, Lisiane B Meira4, Laszlo Nagy2,7 and Axel Nohturfft1* Abstract Background: Lysosomes play important roles in multiple aspects of physiology, but the problem of how the transcription of lysosomal genes is coordinated remains incompletely understood. The goal of this study was to illuminate the physiological contexts in which lysosomal genes are coordinately regulated and to identify transcription factors involved in this control. Results: As transcription factors and their target genes are often co-regulated, we performed meta-analyses of array-based expression data to identify regulators whose mRNA profiles are highly correlated with those of a core set of lysosomal genes. Among the ~50 transcription factors that rank highest by this measure, 65% are involved in differentiation or development, and 22% have been implicated in interferon signaling. The most strongly correlated candidate was Stat6, a factor commonly activated by interleukin-4 (IL-4) or IL-13. Publicly available chromatin immunoprecipitation (ChIP) data from alternatively activated mouse macrophages show that lysosomal genes are overrepresented among Stat6-bound targets. Quantification of RNA from wild-type and Stat6-deficient cells indicates that Stat6 promotes the expression of over 100 lysosomal genes, including hydrolases, subunits of the vacuolar H+ ATPase and trafficking factors. -

Full-Text.Pdf
Existence of Conventional Dendritic Cells in Gallus gallus Revealed by Comparative Gene Expression Profiling This information is current as Thien-Phong Vu Manh, Hélène Marty, Pierre Sibille, Yves of September 24, 2021. Le Vern, Bernd Kaspers, Marc Dalod, Isabelle Schwartz-Cornil and Pascale Quéré J Immunol 2014; 192:4510-4517; Prepublished online 16 April 2014; doi: 10.4049/jimmunol.1303405 Downloaded from http://www.jimmunol.org/content/192/10/4510 Supplementary http://www.jimmunol.org/content/suppl/2014/04/16/jimmunol.130340 Material 5.DCSupplemental http://www.jimmunol.org/ References This article cites 34 articles, 13 of which you can access for free at: http://www.jimmunol.org/content/192/10/4510.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 24, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2014 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Existence of Conventional Dendritic Cells in Gallus gallus Revealed by Comparative Gene Expression Profiling Thien-Phong Vu Manh,*,†,‡,1 He´le`ne Marty,†,x,{,1 Pierre Sibille,‖ Yves Le Vern,x,{ Bernd Kaspers,# Marc Dalod,*,†,‡,2 Isabelle Schwartz-Cornil,‖,2 and Pascale Que´re´x,{,2 The existence of conventional dendritic cells (cDCs) has not yet been demonstrated outside mammals. -

Glycosylation Inhibition Reduces Cholesterol Accumulation in NPC1 Protein-Deficient Cells
Glycosylation inhibition reduces cholesterol accumulation in NPC1 protein-deficient cells Jian Li1, Maika S. Deffieu1, Peter L. Lee1, Piyali Saha, and Suzanne R. Pfeffer2 Department of Biochemistry, Stanford University School of Medicine, Stanford, CA 94305-5307 Edited by Stuart A. Kornfeld, Washington University School of Medicine, St. Louis, MO, and approved October 28, 2015 (received for review October 16, 2015) Lysosomes are lined with a glycocalyx that protects the limiting In this paper, we have used two approaches to modify the gly- membrane from the action of degradative enzymes. We tested the cocalyx. Alteration of glycosylation decreases lysosomal cholesterol hypothesis that Niemann-Pick type C 1 (NPC1) protein aids the transfer levels in NPC1-deficient Chinese hamster ovary (CHO) and human of low density lipoprotein-derived cholesterol across this glycocalyx. A cells. These experiments support a model in which NPC1 protein prediction of this model is that cells will be less dependent upon NPC1 functions to help cholesterol traverse the glycocalyx that lines the if their glycocalyx is decreased in density. Lysosome cholesterol content interior of lysosome limiting membranes. was significantly lower after treatment of NPC1-deficient human fibroblasts with benzyl-2-acetamido-2-deoxy-α-D-galactopyrano- Results and Discussion side, an inhibitor of O-linked glycosylation. Direct biochemical LAMP1 and LAMP2 proteins represent the major glycoproteins measurement of cholesterol showed that lysosomes purified from of the lysosome membrane (12). These proteins are glycosylated NPC1-deficient fibroblasts contained at least 30% less cholesterol on both asparagine residues (N linked) and serine or threonine when O-linked glycosylation was blocked. -

LAMP2 Gene Lysosomal Associated Membrane Protein 2
LAMP2 gene lysosomal associated membrane protein 2 Normal Function The LAMP2 gene provides instructions for making a protein called lysosomal associated membrane protein-2 (LAMP-2), which, as its name suggests, is found in the membrane of cellular structures called lysosomes. Lysosomes are compartments in the cell that digest and recycle materials. The role the LAMP-2 protein plays in the lysosome is unclear. Some researchers think the LAMP-2 protein may help transport cellular materials or digestive enzymes into the lysosome. The transport of cellular materials into lysosomes requires the formation of cellular structures called autophagic vacuoles ( or autophagosomes). Cellular material that will be degraded in a lysosome is first enclosed in an autophagic vacuole inside the cell. The autophagic vacuole attaches ( fuses) to a lysosome to transfer the cellular material into the lysosome where it can be broken down. The LAMP-2 protein may be involved in the fusion between autophagic vacuoles and lysosomes. Slightly different versions (isoforms) of the LAMP-2 protein are produced: LAMP-2A, LAMP-2B, and LAMP-2C. These isoforms are found in different tissues throughout the body. LAMP-2B is the main isoform found in the heart and the muscles used for movement (skeletal muscles). Health Conditions Related to Genetic Changes Danon disease There are many mutations in the LAMP2 gene that can cause Danon disease. Danon disease is a condition characterized by weakening of the heart muscle (cardiomyopathy) , weakening of skeletal muscles (myopathy), and intellectual disability. This condition affects men more severely than women. The LAMP2 gene mutations that cause Danon disease lead to the production of very little or no LAMP-2 protein.