Changing Patterns of Malaria in Grande Comore After a Drastic Decline: Importance of Fine-Scale Spatial Analysis to Inform Future Control Actions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Centre Souscentreserie Numéro Nom Et Prenom
Centre SousCentreSerie Numéro Nom et Prenom MORONI Chezani A1 2292 SAID SAMIR BEN YOUSSOUF MORONI Chezani A1 2293 ADJIDINE ALI ABDOU MORONI Chezani A1 2297 FAHADI RADJABOU MORONI Chezani A4 2321 AMINA ASSOUMANI MORONI Chezani A4 2333 BAHADJATI MAOULIDA MORONI Chezani A4 2334 BAIHAKIYI ALI ACHIRAFI MORONI Chezani A4 2349 EL-ANZIZE BACAR MORONI Chezani A4 2352 FAOUDIA ALI MORONI Chezani A4 2358 FATOUMA MAOULIDA MORONI Chezani A4 2415 NAIMA SOILIHI HAMADI MORONI Chezani A4 2445 ABDALLAH SAID MMADINA NABHANI MORONI Chezani A4 2449 ABOUHARIA AHAMADA MORONI Chezani A4 2450 ABOURATA ABDEREMANE MORONI Chezani A4 2451 AHAMADA BACAR MOUKLATI MORONI Chezani A4 2457 ANRAFA ISSIHAKA MORONI Chezani A4 2458 ANSOIR SAID AHAMADA MORONI Chezani A4 2459 ANTOISSI AHAMADA SOILIHI MORONI Chezani D 2509 NADJATE HACHIM MORONI Chezani D 2513 BABY BEN ALI MSA MORONI Dembeni A1 427 FAZLAT IBRAHIM MORONI Dembeni A1 464 KASSIM YOUSSOUF MORONI Dembeni A1 471 MOZDATI MMADI ADAM MORONI Dembeni A1 475 SALAMA MMADI ALI MORONI Dembeni A4 559 FOUAD BACAR SOILIHI ABDOU MORONI Dembeni A4 561 HAMIDA IBRAHIM MORONI Dembeni A4 562 HAMIDOU BACAR MORONI Dembeni D 588 ABDOURAHAMANE YOUSSOUF MORONI Dembeni D 605 SOIDROUDINE IBRAHIMA MORONI FoumboudzivouniA1 640 ABDOU YOUSSOUF MORONI FoumboudzivouniA1 642 ACHRAFI MMADI DJAE MORONI FoumboudzivouniA1 643 AHAMADA MOUIGNI MORONI FoumboudzivouniA1 654 FAIDATIE ABDALLAH MHADJOU MORONI FoumbouniA4 766 ABDOUCHAKOUR ZAINOUDINE MORONI FoumbouniA4 771 ALI KARIHILA RABOUANTI MORONI FoumbouniA4 800 KARI BEN CHAFION BENJI MORONI FoumbouniA4 840 -

Ecosystem Profile Madagascar and Indian
ECOSYSTEM PROFILE MADAGASCAR AND INDIAN OCEAN ISLANDS FINAL VERSION DECEMBER 2014 This version of the Ecosystem Profile, based on the draft approved by the Donor Council of CEPF was finalized in December 2014 to include clearer maps and correct minor errors in Chapter 12 and Annexes Page i Prepared by: Conservation International - Madagascar Under the supervision of: Pierre Carret (CEPF) With technical support from: Moore Center for Science and Oceans - Conservation International Missouri Botanical Garden And support from the Regional Advisory Committee Léon Rajaobelina, Conservation International - Madagascar Richard Hughes, WWF – Western Indian Ocean Edmond Roger, Université d‘Antananarivo, Département de Biologie et Ecologie Végétales Christopher Holmes, WCS – Wildlife Conservation Society Steve Goodman, Vahatra Will Turner, Moore Center for Science and Oceans, Conservation International Ali Mohamed Soilihi, Point focal du FEM, Comores Xavier Luc Duval, Point focal du FEM, Maurice Maurice Loustau-Lalanne, Point focal du FEM, Seychelles Edmée Ralalaharisoa, Point focal du FEM, Madagascar Vikash Tatayah, Mauritian Wildlife Foundation Nirmal Jivan Shah, Nature Seychelles Andry Ralamboson Andriamanga, Alliance Voahary Gasy Idaroussi Hamadi, CNDD- Comores Luc Gigord - Conservatoire botanique du Mascarin, Réunion Claude-Anne Gauthier, Muséum National d‘Histoire Naturelle, Paris Jean-Paul Gaudechoux, Commission de l‘Océan Indien Drafted by the Ecosystem Profiling Team: Pierre Carret (CEPF) Harison Rabarison, Nirhy Rabibisoa, Setra Andriamanaitra, -

Early Recovery Plan
UNION OF COMOROS COMOROS FLOODING 2012 Early Recovery Plan Moroni, August 2012 TABLE OF CONTENTS ACRONYMS AND ABBREVIATIONS ..................................................................................................................... 3 FOREWORD ....................................................................................................................................................... 4 STATEMENT BY H.E. DR IKILILOU DHOININE, PRESIDENT OF THE UNION OF COMOROS .......................................................... 4 FOREWORD ....................................................................................................................................................... 5 STATEMENT BY MR DOUGLAS CASSON COUTTS, UNITED NATIONS RESIDENT COORDINATOR .................................................. 5 ACKNOWLEDGEMENTS ...................................................................................................................................... 6 EXECUTIVE SUMMARY....................................................................................................................................... 7 BASIC HUMANITARIAN AND DEVELOPMENT INDICATORS FOR THE UNION OF COMOROS ................................. 8 TABLE I. SUMMARY OF REQUIREMENTS – BY SECTOR.......................................................................................... 8 TABLE II. SUMMARY OF REQUIREMENTS – BY UN ORGANIZATION.......................................................................... 9 1. CONTEXT AND HUMANITARIAN CONSEQUENCES ..................................................................................... -

Plan D'aménagement Et De Gestion Du Parc National Cœlacanthe 2017
Parcs Nationaux RNAPdes Comores UNION DES COMORES Unité – Solidarité – Développement Vice-Présidence Chargée du Ministère de l’Agriculture, de la Pêche, de l’Environnement, de l’Aménagement du Territoire et de l’Urbanisme Parcs Nationaux des Comores Plan d’Aménagement et De Gestion du Parc National Cœlacanthe 2017-2021 Janvier 2018 Les avis et opinions exprimés dans ce document sont celles des auteurs, et ne reflètent pas forcément les vues de la Vice Présidence - Ministère de l’Agriculture, de la Pêche, de l’Environnement, de l’Aménagement du Territoire et de l’Urbanisme, ni du PNUD, ni du FEM (UNDP - GEF) Mandaté par L’Union des Comores, Vice-Présidence Chargée du Ministère de l’Agriculture, de la Pêche, de l’Environnement, de l’Aménagement du Territoire et de l’Urbanisme, Parcs nationaux des Comores Et le Programme des Nations Unies pour le Développement, PNUD Fonds Mondial pour l’Environnement, FEM Maison du PNUD, Hamramba BP. 648, Moroni, Union des Comores T +269 7731558/9, F +269 7731577 www.undp.org Titre du Projet d’appui RNAP Développement d’un réseau national d’aires protégées terrestres et marines représentatives du patrimoine naturel unique des Comores et cogérées par les communautés villageoises locales. PIMS : 4950, ID ATLAS : 00090485 Citation : Parcs nationaux des Comores (2017). Plan d’Aménagement et de Gestion du Parc National Cœlacanthe. 2017-2021. 134 p + Annexes 98 p. Pour tous renseignements ou corrections : Lacroix Eric, Consultant international UNDP [email protected] Fouad ABDOU RABI, Coordinateur RNAP [email protected] Plan d’aménagement et de gestion du Parc national Cœlacanthe - 2017 2 Avant-propos Depuis 1994 le souhait des Comoriennes et Comoriens et de leurs amis du monde entier est de mettre en place un Système pour la protection et le développement des aires protégées des Comores. -

Union Des Comores Évaluation De Niveau National
UNION DES COMORES ÉVALUATION DE NIVEAU NATIONAL Rapport de synthèse Volume 2: Annexes Novembre 2006 Evaluation pour le compte de la Commission Européenne LES COMORES : EVALUATION DE NIVEAU NATIONAL EGEVAL Cette Evaluation a été réalisée à la demande de: l’Unité d’Evaluation commune à: l’Office de la Coopération EuropeAid la Direction Générale pour le Développement et la Direction des Relations Extérieurs Cette évaluation a été réalisée par EGEVAL L’évaluation a été gérée par l’Unité d’Evaluation, laquelle a également présidé le groupe de référence composé des membres des services EuropeAid, DG Développement et la Délégation de la CE à Maurice Les opinions exprimées dans ce document représentent les points de vue des auteurs et ne reflètent pas nécessairement celles de la Commission Européenne ou celles des autorités de l’Union des Comores 1 LES COMORES : EVALUATION DE NIVEAU NATIONAL EGEVAL Rapport Final Volume 1 Rapport sans annexes Volume 2 Annexes Volume 3 Matrice d’information 2 LES COMORES : EVALUATION DE NIVEAU NATIONAL EGEVAL Volume 2 – Annexes Table des matières ANNEXE 1 : TERMES DE RÉFÉRENCE 4 ANNEXE 2 : FICHES DE PROJET 20 ANNEXE 3 : PRÉSENTATION SUCCINCTE DE L’ÉQUIPE DES ÉVALUATEURS 33 ANNEXE 4 : ÉTAT DES ENGAGEMENTS 35 ANNEXE 5 : MÉTHODOLOGIE DE LA PHASE DE TERRAIN 44 ANNEXE 6 : BIBLIOGRAPHIE 48 ANNEXE 7 : ETAT DE LA DOCUMENTATION DES PROJETS DISPONIBLE 52 ANNEXE 8 : LISTE DES PERSONNES RENCONTRÉES 56 3 LES COMORES : EVALUATION DE NIVEAU NATIONAL EGEVAL Annexe 1 : Termes de référence 4 SOMMAIRE 1. MANDAT ET OBJECTIFS 3 2. CONTEXTE 3 3. CHAMP DE L’EVALUATION 4 4. -
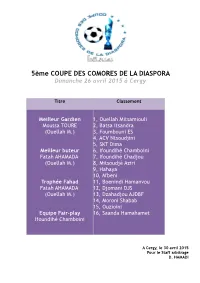
Résultats CCD 5
5ème COUPE DES COMORES DE LA DIASPORA Dimanche 26 avril 2015 à Cergy Titre Classement Meilleur Gardien 1, Ouellah Mitsamiouli Moussa TOURE 2, Batsa Itsandra (Ouellah M.) 3, Foumbouni ES 4, ACV Ntsoudjini 5, SKT Dima Meilleur buteur 6, Ifoundihé Chamboini Fatah AHAMADA 7, Ifoundihé Chadjou (Ouellah M.) 8, Mitsoudjé Aziri 9, Hahaya 10, M'beni Trophée Fahad 11, Boenindi Hamanvou Fatah AHAMADA 12, Djomani DJS (Ouellah M.) 13, Dzahadjou AJDBF 14, Moroni Shabab 15, Ouzioini Equipe Fair-play 16, Saanda Hamahamet Ifoundihé Chamboini A Cergy, le 30 avril 2015 Pour le Staff arbitrage D. HAMADI CCD 2015 / POULE A Tableau des matches Matches Équipes Scores Équipes Foumbouni E-S 2 – 0 AJDBF Dzahadjou Ouzioini 0 – 1 Mitsoudjé AZIRI AJDBF Dzahadjou 0 – 2 Mitsoudjé AZIRI Foumbouni E-S 3 – 0 Ouzioini Foumbouni E-S 2 – 2 Mitsoudjé AZIRI Ouzioini 1 – 1 AJDBF Dzahadjou Tableau des points 1er Match 2ème Match 3ème Match Total Diff. Foumbouni E-S 3 3 1 7 7 AJDBF Dzahadjou 0 0 1 1 / Ouzioini 0 0 1 1 / Mitsoudjé AZIRI 3 3 1 7 5 Rappel : victoire : + 3 / nul : + 1 / défaite : 0 Premier : Foumbouni ES / Deuxième : Mitsoudjé AZIRI CCD 2015 / POULE B Tableau des matches Matches Équipes Scores Équipes Ifoundihé Chamboini 1 – 1 Ifoundihé Chadjou Djomani DJS 1 – 0 Hahaya Ifoundihé Chadjou 0 – 1 Hahaya Djomani DJS 0 – 1 Ifoundihé Chamboini Ifoundihé Chadjou 5 – 2 Djomani DJS Hahaya 0 – 0 Ifoundihé Chamboini Tableau des points 1er Match 2ème Match 3ème Match Total Diff. Ifoundihé Chamboini 1 3 1 5 / Ifoundihé Chadjou 1 0 3 4 6 Djomani DJS 3 0 0 3 3 Hahaya 0 3 1 4 / Rappel : victoire : + 3 / nul : + 1 / défaite : 0 Premier : Ifoundihé Chamboini / Deuxième : Ifoundihé Chadjou CCD 2015 / POULE C Tableau des matches Matches Équipes Scores Équipes Batsa Itsandra 0 – 0 ACV Ntsoudjini Moroni Al-Shabab 2 – 1 Saada Hamahamet ACV Ntsoudjini 2 – 0 Saada Hamahamet Batsa Itsandra 2 – 0 Moroni Al-Shabab Moroni Al-Shabab 1 – 3 ACV Ntsoudjini Saada Hamahamet 0 – 2 Batsa Itsandra Tableau des points 1er Match 2ème Match 3ème Match Total Diff. -

Mission 1 Cadre Institutionnel
UNION DES COMORES --------------------- VICE –PRESIDENCE EN CHARGE DU MINISTERE DE LA PRODUCTION, DE L’ENVIRONNEMENT, DE L’ENERGIE, DE L’INDUSTRIE ET DE L’ARTISANAT ------------------- DIRECTION GENERALE DE L’ENERGIE, DES MINES ET DE L’EAU (DGEME) UNITE DE GESTION DU PROJET ALIMENTATION EN EAU POTABLE ET ASSAINISSEMENT --------------------- PROJET D ’A LIMENTATION EN EAU POTABLE ET D SSAINISSEMENT DANS LES ILES DE ’A (AEPA) 3 L’U NION DES COMORES (F INANCEMENT BAD) ETUDES TECHNIQUES, DU CADRE INSTITUTIONNEL ET DU PROGRAMME NATIONAL D’AEPA Mission 1 : Elab oration du cadre institutionnel, o rganisationnel et financier du s ecteur d’AEPA Edition définitive JUIN 2013 71, Avenue Alain Savary Bloc D – 2ème étage - App 23 ENTREPRISE D’ETUDES DE DEVELOPPEMENT RURAL 1003 Cité El Khadra - Tunis EEDR MAMOKATRA S.A. Tél : (216) 71 809 686 Société Anonyme au capital de 20.000.000 d’Ariary Fax : (216) 71 806 313 Siège social : Villa Mamokatra Nanisana E-mail : [email protected] 101 ANTANANARIVO Site web : www.hydroplante.com …: (261.20) 22 402-14 ; 22 403-78 * 961 E-mail : [email protected] 1 Elaboration du cadre institutionnel, organisationnel et financier du secteur de l’AEPA des Comores PAEPA PREFACE L’élaboration du cadre institutionnel, organisationnel et financier du secteur d’eau potable et d’Assainissement s’inscrit dans le cadre de la composante 1 du Projet d’Alimentation en Eau Potable et d’Assainissement (PAEPA – Comores – projet n : P-KM-EA0-001) financé par un don de la Banque Africaine de Développement. Tel que défini par le rapport d’évaluation du projet, le PAEPA comprend quatre (4) composantes: (i) l’Etude du Cadre institutionnel, organisationnel et financier ainsi que l’élaboration d’un plan stratégique à l’horizon 2030; (ii) le développement et la réhabilitation des infrastructures d’alimentation en eau potable et d’assainissement (AEPA) de plusieurs localités dont Moroni, Ouani, Mutsamudu, Fomboni et Mbéni; (iii) l’Appui Institutionnel et (iv) la Gestion du Projet. -

Vol. 22 - Comoros
Marubeni Research Institute 2016/09/02 Sub -Saharan Report Sub-Saharan Africa is one of the focal regions of Global Challenge 2015. These reports are by Mr. Kenshi Tsunemine, an expatriate employee working in Johannesburg with a view across the region. Vol. 22 - Comoros June 10, 2016 It was well known that Marilyn Monroe wore Chanel No. 5 perfume when she went to bed. Did you know that Chanel No. 5’s essence (essential oils) comes from the flower called ylang-ylang, which is found in the African country of Comoros? Comoros is also where the so-called “living fossils”, a rare pre-historic species of fish called coelacanths, discovered in 1938 in South Africa after having thought to be extinct, are mostly found. So this time I would like to introduce the country of Comoros, fascinating like Marilyn Monroe and a little mysterious like the coelacanths. Table 1: Comoros Country Information The Union of the Comoros is an archipelago island nation located off the coast of East Africa east of Mozambique and northwest from Madagascar. 4 main islands make up the Comoros archipelago, Grande Comore, Moheli, Anjouan and Mayotte, with Grande Comore, Moheli, and Anjouan forming the Union of Comoros and Mayotte falling under French jurisdiction as an ‘overseas department” or region. The population of the 3 islands making up the Union of the Comoros is about 800,000, while their total land area comes to 2,236 square kilometers, about the same land size as Tokyo, which makes it quite a small country. Nominal GDP is roughly $600 million, which is second from the bottom among the 45 sub-Saharan African countries, just above Sao Tome and Principe, and its population is the 5th lowest (note 1). -

Comoros Mission Notes
Peacekeeping_4.qxd 1/14/07 2:29 PM Page 109 4.5 Comoros The 2006 elections in the Union of the support for a solution that preserves the coun- Comoros marked an important milestone in the try’s unity. After Anjouan separatists rejected peace process on the troubled archipelago. New an initial deal in 1999, the OAU, under South union president Ahmed Abdallah Mohamed African leadership, threatened sanctions and Sambi won 58 percent of the vote in elections, military action if the island continued to pur- described by the African Union as free and fair, sue secession. All parties eventually acceded and took over on 27 May 2006, in the islands’ to the 2001 Fomboni Accords, which provided first peaceful leadership transition since 1975. for a referendum on a new constitution in The AU Mission for Support to the Elections in advance of national elections. the Comoros (AMISEC), a short-term mission The core of the current deal is a federated devoted to the peaceful conduct of the elections, structure, giving each island substantial auton- withdrew from Comoros at the end of May, hav- omy and a turn at the presidency of the union, ing been declared a success by the AU and the which rotates every four years. Presidential Comorian government. The Comoros comprises three islands: Grande Comore (including the capital, Moroni), Anjouan, and Moheli. Following independ- ence from France in 1975, the country experi- enced some twenty coups in its first twenty- five years; meanwhile, Comoros slid ever deeper into poverty, and efforts at administra- tive centralization met with hostility, fueling calls for secession and/or a return to French rule in Anjouan and Moheli. -

Eies) Et Plan De Gestion Environnementale Et Sociale (Pges) Du Projet Comoresol – Grandes Comores
UNION DES COMORES Unité – Solidarité – Développement ---------------- MINISTERE DES FINANCES ET DU BUDGET ---------------- PROGRAMME REGIONAL D’INFRASTRUCTURES DE COMMUNICATION RCIP-4 ------ ETUDE D’IMPACT ENVIRONNEMENTAL ET SOCIAL (EIES) ET PLAN DE GESTION ENVIRONNEMENTALE ET SOCIALE (PGES) DU PROJET COMORESOL – GRANDES COMORES Version finale Novembre 2019 SOMMAIRE SOMMAIRE 1 - RESUME EXECUTIF EN FRANCAIS ..................................................................... 7 2 - UFUPIZI WA MTRILIYO NDZIANI .................................................................... 27 3 - CONTEXTE GENERAL, OBJECTIFS ET METHODOLOGIE D’ELABORATION DE L’EIES ........................................................................................................................ 46 4 - BREVE DESCRIPTION DU PROJET ................................................................... 51 5 - CADRE JURIDIQUE ET LES POLITIQUES DE SAUVEGARDE DE LA BANQUE MONDIALE .............................................................................................................. 81 6 - DESCRIPTION ET ANALYSE DE L’ETAT INITIAL DU SITE ET DE SON ENVIRONNEMENT .................................................................................................. 97 7 - CONSULTATION DU PUBLIC .......................................................................... 154 8 - ANALYSE ET EVALUATION DES IMPACTS ENVIRONNEMENTAUX ET SOCIAUX DU PROJET ........................................................................................... 155 ETUDE D’IMPACT ENVIRONNEMENTAL -

Socmon Comoros NOAA
© C3 Madagascar and Indian Ocean Islands Programme 2010 C3 Madagascar and Indian Ocean Islands Programme is a collaborative initiative between Community Centred Conservation (C3), a non-profit company registered in England no. 5606924 and local partner organizations. The study described in this report was funded by the NOAA Coral Reef Conservation Program. Suggested citation: C3 Madagascar and Indian Ocean Islands Programme (2010) SOCIO- ECONOMIC ASSESSMENT AND IDENTIFICATION OF POTENTIAL SITES FOR COMMUNITY-BASED CORAL REEF MANAGEMENT IN THE COMOROS. A Report Submitted to the NOAA Coral Reef Conservation Program, USA 22pp FOR MORE INFORMATION C3 Madagascar and Indian Ocean NOAA Coral Reef Conservation Program Islands Programme (Comoros) Office of Response and Restoration BP8310 Moroni NOAA National Ocean Service Iconi 1305 East-West Highway Union of Comoros Silver Spring, MD 20910 T. +269 773 75 04 USA CORDIO East Africa Community Centred Conservation #9 Kibaki Flats, Kenyatta Beach, (C3) Bamburi Beach www.c-3.org.uk PO BOX 10135 Mombasa 80101, Kenya [email protected] [email protected] Cover photo: Lobster fishers in northern Grande Comore SOCIO-ECONOMIC ASSESSMENT AND IDENTIFICATION OF POTENTIAL SITES FOR COMMUNITY-BASED CORAL REEF MANAGEMENT IN THE COMOROS Edited by Chris Poonian Community Centred Conservation (C3) Moroni 2010 ACKNOWLEDGEMENTS This report is the culmination of the advice, cooperation, hard work and expertise of many people. In particular, acknowledgments are due to the following for their contributions: COMMUNITY CENTRED -
Towards a More United & Prosperous Union of Comoros
TOWARDS A MORE UNITED & PROSPEROUS Public Disclosure Authorized UNION OF COMOROS Systematic Country Diagnostic Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized ABBREVIATIONS & ACRONYMS i CPIA Country Policy and Institutional Assessment CSOs Civil Society Organizations DeMPA Debt Management Performance Assessment DPO Development Policy Operation ECP Economic Citizenship Program EEZ Exclusive Economic Zone EU European Union FDI Foreign Direct Investment GDP Gross Domestic Product GNI Gross National Income HCI Human Capital Index HDI Human Development Index ICT Information and Communication Technologies IDA International Development Association IFC International Finance Corporation IMF International Monetary Fund INRAPE National Institute for Research on Agriculture, Fisheries, and the Environment LICs Low-income Countries MDGs Millennium Development Goals MIDA Migration for Development in Africa MSME Micro, Small, and Medium Enterprises NGOs Non-profit Organizations PEFA Public Expenditure and Financial Accountability PPP Public/Private Partnerships R&D Research and Development SADC Southern African Development Community SDGs Sustainable Development Goals SOEs State-Owned Enterprises SSA Sub-Saharan Africa TFP Total Factor Productivity WDI World Development Indicators WTTC World Travel & Tourism Council ii ACKNOWLEDGEMENTS We would like to thank members of the Comoros Country Team from all Global Practices of the World Bank and the International Finance Corporation, as well as the many stakeholders in Comoros (government authorities, think tanks, academia, and civil society organizations, other development partners), who have contributed to the preparation of this document in a strong collaborative process (see Annex 1). We are grateful for their inputs, knowledge and advice. This report has been prepared by a team led by Carolin Geginat (Program Leader EFI, AFSC2) and Jose Luis Diaz Sanchez (Country Economist, GMTA4).