Surgical Management of Jaw-Winking Synkinesis and Ptosis in Marcus Gunn Syndrome: a Systematic Outcomes Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Prevalence of Amblyopia in Congenital Blepharoptosis: a Systematic Review and Meta-Analysis
Int J Ophthalmol, Vol. 12, No. 7, Jul.18, 2019 www.ijo.cn Tel: 8629-82245172 8629-82210956 Email: [email protected] ·Meta-Analysis· Prevalence of amblyopia in congenital blepharoptosis: a systematic review and Meta-analysis Jia-Ying Zhang1,2, Xiao-Wei Zhu1,2, Xia Ding1,2, Ming Lin1,2, Jin Li1,2 1Department of Ophthalmology, Shanghai Ninth People’s and management of amblyopia should be integral to the Hospital, Shanghai Jiao Tong University School of Medicine, treatment of congenital ptosis. Shanghai 200011, China ● KEYWORDS: amblyopia; congenital ptosis; blepharophimosis; 2Shanghai Key Laboratory of Orbital Diseases and Ocular systematic review Oncology, Shanghai 200011, China DOI:10.18240/ijo.2019.07.21 Correspondence to: Jin Li. Department of Ophthalmology, Shanghai Ninth Peolple’s Hospital, Shanghai Jiao Tong Citation: Zhang JY, Zhu XW, Ding X, Lin M, Li J. Prevalence of University School of Medicine, No.639, Zhizaoju Road, amblyopia in congenital blepharoptosis: a systematic review and Shanghai 200011, China. [email protected] Meta-analysis. Int J Ophthalmol 2019;12(7):1187-1193 Received: 2018-09-25 Accepted: 2019-03-05 INTRODUCTION Abstract ongenital blepharoptosis is an eyelid disorder that ● AIM: To conduct a systematic review and Meta-analysis of C is characterized by an involuntary drooping of the the published literature to evaluate the pooled prevalence upper eyelid since birth. Etiologically, myogenic factors are rate of amblyopia in patients with congenital ptosis. most common, referring to dysgenesis or weakness of the ● METHODS: We searched the PubMed, Embase, the levator muscle and sometimes the superior rectus muscle. Cochrane Central Register of Controlled Trials, China The etiological subtypes of congenital ptosis include simple National Knowledge Infrastructure, Wanfang Data, and congenital ptosis, blepharophimosis-ptosis-epicanthus inversus Chongqing VIP databases for studies reporting the syndrome (BPES), Marcus Gunn jaw-winking syndrome prevalence of amblyopia in patients with congenital ptosis. -

PG Series Ophthalmology Buster
PG Series Ophthalmology Buster PG Series Ophthalmology Buster E Ahmed Formerly Head, Department of Ophthalmology Calcutta National Medical College Consultant, Eye Care and Research Centre Kolkata JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3, EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672, Rel: 32558559 Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite, Ahmedabad 380 015 Phones: +91-079-26926233, Rel: +91-079-32988717, Fax: +91-079-26927094 e-mail: [email protected] • 202 Batavia Chambers, 8 Kumara Krupa Road, Kumara Park East, Bangalore 560 001 Phones: +91-80-22285971, +91-80-22382956, Rel: +91-80-32714073, Fax: +91-80-22281761 e-mail: [email protected] • 282 IIIrd Floor, Khaleel Shirazi Estate, Fountain Plaza, Pantheon Road, Chennai 600 008 Phones: +91-44-28193265, +91-44-28194897, Rel: +91-44-32972089 Fax: +91-44-28193231 e-mail: [email protected] • 4-2-1067/1-3, 1st Floor, Balaji Building, Ramkote Cross Road, Hyderabad 500 095 Phones: +91-40-66610020, +91-40-24758498, Rel:+91-40-32940929 Fax:+91-40-24758499, e-mail: [email protected] • No. 41/3098, B & B1, Kuruvi Building, St. Vincent Road, Kochi 682 018, Kerala Phones: +91-0484-4036109, +91-0484-2395739, +91-0484-2395740 e-mail: [email protected] • 1-A Indian Mirror Street, Wellington Square, Kolkata 700 013 Phones: +91-33-22451926, +91-33-22276404, +91-33-22276415, Rel: +91-33-32901926 Fax: +91-33-22456075, e-mail: [email protected] • 106 Amit Industrial Estate, 61 Dr SS Rao Road, Near MGM Hospital, Parel, Mumbai 400 012 Phones: +91-22-24124863, +91-22-24104532, Rel: +91-22-32926896 Fax: +91-22-24160828, e-mail: [email protected] • “KAMALPUSHPA” 38, Reshimbag, Opp. -

Ocular Motility
10 Ocular Motility C. Denise Pensyl, William J. Benjamin linicians are faced with the challenge of differenti approximately 2 rnm, below which the effects of Cating the etiologies of asthenopia, blur, diplopia, reduced retinal illuminance and diffraction outweigh and headaches associated with the use of the eyes by the beneficial aspects ofan increase in depth offield and their patients. Oculomotor deficiencies can be one of reduction of ocular spherical aberration. The entrance several possible causes of such symptoms and are the pupil also controls blur circle size at the retina for object result of defects in the central nervous system, afferent rays not originating from the far point plane of the eye. or efferent nerve pathways, or local conditions of a The entrance pupil averages 3.5 mm in diameter in nature so as to impede appropriate oculomotor func adults under normal illumination but can range from tion. Oculomotor function will be extensively analyzed 1.3 mm to 10 mm. It is usually centered on the optic during phorometry (see Chapter 21) in terms of binoc axis of the eye but is displaced temporally away from ularity and muscle balance after the subjective refraction the visual axis or line of sight an average of 5 degrees. has been completed. This chapter focuses on clinical The entrance pupil is decentered approximately procedures that are typically used to analyze oculomo 0.15 mm nasally and 0.1 mm inferior to the geometric tor function before the subjective refraction is per center ofthe cornea. J This amount ofdecentration is not formed, though in some cases the practitioner may distinguished in casual observation or by the clinician's decide to use a few of these tests after the refraction is normal examination ofthe pupils. -

Frontalis Sling: a Modified Simple Technique
Br J Ophthalmol: first published as 10.1136/bjo.69.6.443 on 1 June 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 443-445 Frontalis sling: a modified simple technique S M BETHARIA From Dr Rajendra Prasad Centrefor Ophthalmic Sciences, Ansari Nagar, New Delhi 110029, India SUMMARY A modified simple technique of brow suspension by using 4-0 Supramid (non- absorbable thread) suture and only one skin incision is described in 25 eyes of 15 cases of ptosis, including cases of congenital and mechanical ptosis and ptosis with Marcus Gunn phenomenon. This technique avoids the use of any special instruments such as the Reese ptosis knife and Wright needle. A sling operation is by far the easiest of all ptosis with the Marcus Gunn phenomenon after disinser- operations to perform. Though it may have im- tion of levator muscle from the tarsal plate (Table 1). portant disadvantages, such as the risk of lagophthal- mos and lid lag in down gaze, it is the operation of SURGICAL PROCEDURE choice for certain cases of gross bilateral ptosis with The operation is carried out under general anaes- poor levator function as seen in the blepharophimosis thesia. The first step is to lift the lid with the help of syndrome, cases of mechanical ptosis, and in severe the index finger just medial to the centre of the upper unilateral ptosis covering the pupillary area to pre- lid and observe the contour of the lid margin in vent amblyopia before a definitive levator operation relation to the limbus. This gives an approximate idea can be carried out. -

A Dictionary of Neurological Signs.Pdf
A DICTIONARY OF NEUROLOGICAL SIGNS THIRD EDITION A DICTIONARY OF NEUROLOGICAL SIGNS THIRD EDITION A.J. LARNER MA, MD, MRCP (UK), DHMSA Consultant Neurologist Walton Centre for Neurology and Neurosurgery, Liverpool Honorary Lecturer in Neuroscience, University of Liverpool Society of Apothecaries’ Honorary Lecturer in the History of Medicine, University of Liverpool Liverpool, U.K. 123 Andrew J. Larner MA MD MRCP (UK) DHMSA Walton Centre for Neurology & Neurosurgery Lower Lane L9 7LJ Liverpool, UK ISBN 978-1-4419-7094-7 e-ISBN 978-1-4419-7095-4 DOI 10.1007/978-1-4419-7095-4 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2010937226 © Springer Science+Business Media, LLC 2001, 2006, 2011 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. While the advice and information in this book are believed to be true and accurate at the date of going to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. -

Ocular Manifestations of Inherited Diseases Maya Eibschitz-Tsimhoni
10 Ocular Manifestations of Inherited Diseases Maya Eibschitz-Tsimhoni ecognizing an ocular abnormality may be the first step in Ridentifying an inherited condition or syndrome. Identifying an inherited condition may corroborate a presumptive diagno- sis, guide subsequent management, provide valuable prognostic information for the patient, and determine if genetic counseling is needed. Syndromes with prominent ocular findings are listed in Table 10-1, along with their alternative names. By no means is this a complete listing. Two-hundred and thirty-five of approxi- mately 1900 syndromes associated with ocular or periocular manifestations (both inherited and noninherited) identified in the medical literature were chosen for this chapter. These syn- dromes were selected on the basis of their frequency, the char- acteristic or unique systemic or ocular findings present, as well as their recognition within the medical literature. The boldfaced terms are discussed further in Table 10-2. Table 10-2 provides a brief overview of the common ocular and systemic findings for these syndromes. The table is organ- ized alphabetically; the boldface name of a syndrome is followed by a common alternative name when appropriate. Next, the Online Mendelian Inheritance in Man (OMIM™) index num- ber is listed. By accessing the OMIM™ website maintained by the National Center for Biotechnology Information at http://www.ncbi.nlm.nih.gov, the reader can supplement the material in the chapter with the latest research available on that syndrome. A MIM number without a prefix means that the mode of inheritance has not been proven. The prefix (*) in front of a MIM number means that the phenotype determined by the gene at a given locus is separate from those represented by other 526 chapter 10: ocular manifestations of inherited diseases 527 asterisked entries and that the mode of inheritance of the phe- notype has been proven. -

Congenital Ptosis with Marcus Gunn Phenomenon: Unilateral Correction 6 Rohit Saiju MD 2
Vol. 5 Issue 1, January 2020 Eyelid Issue Asia Pacific Society of Ophthalmic Plastic & Reconstructive Surgery Official Newsletter of Asia Pacific Society of Ophthalmic Plastic & Reconstructive Surgery Asia Pacific Society of Ophthalmic Plastic & Reconstructive Surgery 1 In this Issue Editorial “The eyes are the window to your soul” – William Shakespeare 2 Ben Limbu MD President’s Corner President’s Corner 4 Raoul Paolo D. Henson, MD Original Article 1. Congenital Ptosis with Marcus Gunn Phenomenon: Unilateral correction 6 Rohit Saiju MD 2. Periorbital Aesthetics: Wrinkles, Hills, Valleys and Dark Circles 9 Milind Naik MD 3. Sub-Brow Incision Blepharoplasty (SBBP) for Dermatochalasis : My Experience 15 Masashi Mimura MD 4. Tearful Tear Trough : Anatomy, Grading and Management 19 Kasturi Bhattacharjee MS, Sripurna Ghosh MS, Lana Datuashvili MD Event News APSOPRS Goes to Cambodia 25 Dr. Akshay G Nair Asia Pacific Society of Ophthalmic Plastic & Reconstructive Surgery 3 Original Article Congenital Ptosis with Marcus Gunn Phenomenon: Unilateral correction Prof. Dr. Rohit Saiju MD Head Orbit and Oculoplasty Tilganga Institute of Ophthalmology,Nepal Corresponding Email: [email protected] The Marcus Gunn jaw- although patients are able to mask it after learning to winking phenomenon is control both their lid position and excursion [4]. a rare problem varying The quest for the ideal technique for the correction of in severity from a mild ptosis as well as jaw-winking phenomenon continues. disorder to a significant Various techniques have been proposed from times cosmetic disability. It immemorial. Although many surgical techniques to is a congenital clinical disable the levator complex have been described their entity characterized by results in terms of both jaw-winking, ptosis have reported. -
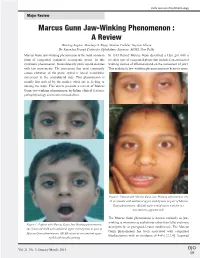
Marcus Gunn Jaw-Winking Phenomenon : a Review Dewang Angmo, Mandeep S
Delhi Journal of Ophthalmology Major Review Marcus Gunn Jaw-Winking Phenomenon : A Review Dewang Angmo, Mandeep S. Bajaj, Neelam Pushker, Supriyo Ghose Dr. Rajendra Prasad Centre for Ophthalmic Sciences, AIIMS, New Delhi Marcus Gunn jaw-winking phenomenon is the most common In 1883 Robert Marcus Gunn described a 15yr girl with a form of congenital synkinetic neurogenic ptosis. In this peculiar type of congenital ptosis that included an associated synkinetic phenomenon, the unilaterally ptotic eyelid elevates winking motion of affected eyelid on the movement of jaw1. with jaw movements. The movement that most commonly This synkinetic jaw-winking phenomenon now bears its name. causes elevation of the ptotic eyelid is lateral mandibular movement to the contralateral side. This phenomenon is usually first noticed by the mother when she is feeding or nursing the baby. This article presents a review of Marcus Gunn jaw-winking phenomenon including clinical features, pathophysiology and treatment modalities. Figure2: Patient with Marcus Gunn Jaw-Winking phenomenon. (A) 22 yrs female with unilateral upper eyelid ptosis as part of Marcus Gunn phenomenon. (B) Left upper eyelid raises with the jaw movement to opposite side. The Marcus Gunn phenomenon is known variously as jaw- winking (a misnomer as eyelid rises rather than falls) and more Figure 1: Patient with Marcus Gunn Jaw-Winking phenomenon. descriptively, as pterygoid-levator synkinesis2. The Marcus (A) 5year old child with unilateral upper eyelid ptosis as part of Gunn phenomenon has been associated with congenital Marcus Gunn phenomenon. (B) Elevation of concomitant upper blepharoptosis with an incidence of 4-6% [2,3,4]. -

A Study on Prevalence of Congenital Ocular Anomalies in Paediatric Age Group
Available online at: www.ijmrhs.com DOI: 10.5958/2319-5886.2015.00177.0 Research article Open Access A STUDY ON PREVALENCE OF CONGENITAL OCULAR ANOMALIES IN PAEDIATRIC AGE GROUP Tupe Parag N1, Chaudhari Sagar V2 ARTICLE INFO ABSTRACT th Introduction: Most congenital anomalies are present long before the time Received: 15 Sep 2015 th nd of birth, some in the embryonic period (up to the7 week of gestation) and Revised: 25 Sep 2015 th Accepted: 30th Sep 2015 other in the fetal period (8 week to term) Purpose: To study the incidence of congenital ocular anomalies in paediatric age group. Materials & 1 Authors details: Assistant Professor, Methods: In this study total 9350 patients were screened. The age and sex 2 Post graduate student, Department of of the patient, gestational age, occurrence of consanguineous, distribution Ophthalmology, Rural Medical of various subtype of congenital anomalies, subtype of congenital cataract, College, Loni, Ahmednagar, age at presentation and diagnosis were noted. Results: The age variation Maharashtra, in the study was between 0-12 years. The maximum number of patients Corresponding author: Tupe Parag N were in the age group of 0-2 years. Male: female ratio was 1:1.4. Number Assistant Professor, Department of cases were reported in anterior segment with full term delivery.32 cases Ophthalmology, Rural Medical having no positive history of consanguineous marriage. Total 12 cases College, Loni, Ahmednagar, were found about chronic dacryocystitis, 8 cases of coloboma of iris and Maharashtra, choroid and each 5 cases of congenital cataract and Microhthalmos were Email: [email protected] found. -

Excluded Conditions
Medical Diagnoses Not an Established Condition - 3 - Not an Established Condition 3-Methylcrotonyl-Coenzyme A (CoA) Carboxylase Deficiency 33-34 weeks EGA (if the birth weight is >1325 grams or 2 lbs 15 oz) 3rd Nerve Palsy (aka: Third Nerve Palsy; Third Cranial Nerve Palsy; 3rd Cranial Nerve Palsy; Oculomotor Palsy; Oculomotor Nerve Palsy; Cranial Nerve III Palsy) - 6 - Not an Established Condition 6th Nerve Palsy (aka: Abducens palsy; Lateral rectus palsy; Cranial mononeuropathy VI) - A - Not an Established Condition Aarskog-Scott syndrome Abnormal Neurological Exam at Discharge from NICU Absent Septum Pellucidum (aka: Absence Septum Pellucidum, Absent Cavum Septum Pellucidum) Achondroplasia Acute Lymphoid Leukemia (aka: ALL) Adams Oliver Syndrome (aka: AOS; Absence Defect of Limbs, Scalp, and Skull; Congenital Scalp Defects with Distal Limb Reduction Anomalies; Aplasia Cutis Congenita with Terminal Transverse Limb Defects) Adjustment Disorder (as defined within DC:0-3R, and diagnosed by specially-qualified professional) Alagille Syndrome (aka: AHD; Arteriohepatic Dysplasia; Cholestasis with Peripheral Pulmonary Stenosis; Syndromatic Hepatic Ductular Hypoplasia) Albinism (aka Ocular Cutaneous Albinism, Oculocutaneous Albinism, Ocular Albinism) Alcohol-Related Neurodevelopmental Disorder (aka: ARND; Fetal Alcohol Spectrum Disorder; FASD) Alport Syndrome (aka: Hematuria-Nephropathy Deafness; Hemorrhagic Familial Nephritis; Hereditary Deafness and Nephropathy; Hereditary Nephritis With Sensory Deafness; Hereditary Nephritis and Nerve Deafness) -

Delhi Journal of Ophthalmology Delhi Journal of Ophthalmology
Delhi Journal of Ophthalmology Delhi Journal of Ophthalmology Editor Rohit Saxena Managing Editor Rajesh Sinha Editorial Committee Editorial Board Parijat Chandra Jitendra Jithani Rajvardhan Azad Vimla Menon Rasik B Vajpayee Tushar Agarwal M.Vanathi Atul Kumar Pradeep Sharma Rajinder Khanna Shibal Bhartiya Prakash Chand Agarwal Ashok K Grover V P Gupta Harbans Lal Munish Dhawan Swati Phuljhele Mahipal S Sachdev S. Bharti Amit Khosla B Ghosh Harinder Sethi Reena Sharma Lalit Verma Ashok Garg Kirti Singh Raghav Gupta Varun Gogia Sharad Lakhotia P K Pandey B P Guliani Ashish Kakkar Sashwat Ray P V Chaddha Ramanjit Sihota S P Garg Rachana Meel Saptorshi Majumdar Dinesh Talwar Divender Sood Arun Baweja Digvijay Singh Shraddha Puranik K P S Malik Rishi Mohan Sanjay Mishra Tanuj Dada Namrata Sharma Tarun Sharma General Information Delhi Journal of Ophthalmology (DJO), once called Visiscan, is a quarterly journal brought out by the Delhi Ophthalmological Society. The journal aims at providing a platform to its readers for free exchange of ideas and information in accordance with the rules laid out for such publication. The DJO aims to become an easily readable referenced journal which will provide the specialists with up to date data and the residents with articles providing expert opinions supported with references. Contribution Methodology Author/Authors must have made significant contribution in carrying out the work and it should be original. It should be accompanied by a letter of transmittal.The article can be sent by email to the Editor or a hard copy posted. Articles receive will be sent to reviewers whose comment will be emailed to the author(s) within 4-6 weeks.