RUG01-000789517 2010 0001 AC.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
HS and Product Codes
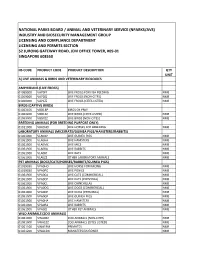
NATIONAL PARKS BOARD / ANIMAL AND VETERINARY SERVICE (NPARKS/AVS) INDUSTRY AND BIOSECURITY MANAGEMENT GROUP LICENSING AND COMPLIANCE DEPARTMENT LICENSING AND PERMITS SECTION 52 JURONG GATEWAY ROAD, JEM OFFICE TOWER, #09-01 SINGAPORE 608550 HS CODE PRODUCT CODE PRODUCT DESCRIPTION QTY UNIT A) LIVE ANIMALS & BIRDS AND VETERINARY BIOLOGICS AMPHIBIANS (LIVE FROGS) 01069000 VAP0FF LIVE FROGS FOR FISH FEEDING NMB 01069000 VAP0ZZ LIVE FROGS (NON-CITES) NMB 01069000 VAP1ZZ LIVE FROGS (CITES LISTED) NMB BIRDS (CAPTIVE BIRDS) 01063100 VBD1BP BIRDS OF PREY 01063200 VBD1ZZ LIVE BIRDS (CITES LISTED) NMB 01063900 VBD0ZZ LIVE BIRDS (NON-CITES) NMB BREEDING ANIMALS (FOR BREEDING PURPOSE ONLY) 01011000 VBA0HO LIVE HORSES FOR BREEDING NMB LABORATORY ANIMALS (MICE/RATS/GUINEA PIGS/HAMSTERS/RABBITS) 01061900 VLA0GP LIVE GUINEA PIGS NMB 01061900 VLA0HA LIVE HAMSTERS NMB 01061900 VLA0MC LIVE MICE NMB 01061900 VLA0RA LIVE RABBITS NMB 01061900 VLA0RT LIVE RATS NMB 01061900 VLA0ZZ OTHER LABORATORY ANIMALS NMB PET ANIMALS (DOGS/CATS/HORSES/RABBITS/GUINEA PIGS) 01019030 VPA0HO LIVE HORSE FOR RACING NMB 01019030 VPA0PO LIVE PONIES NMB 01061900 VPA0CA LIVE CATS (COMMERCIAL) NMB 01061900 VPA0CP LIVE CATS (PERSONAL) NMB 01061900 VPA0CL LIVE CHINCHILLAS NMB 01061900 VPA0DG LIVE DOGS (COMMERCIAL) NMB 01061900 VPA0DP LIVE DOGS (PERSONAL) NMB 01061900 VPA0GP LIVE GUINEA PIGS NMB 01061900 VPA0HA LIVE HAMSTERS NMB 01061900 VPA0RA LIVE RABBITS NMB 01061900 VPA0ZZ OTHER PET ANIMALS NMB WILD ANIMALS (ZOO ANIMALS) 01061900 VWA0ZZ ZOO ANIMALS (NON-CITES) NMB 01061900 VWA1ZZ ZOO ANIMALS (CITES LISTED) NMB 01061100 VWA1PM PRIMATES NMB 01061200 VWA1DG MANATEES/DUGONGS NMB 01061200 VWA1WD WHALES/DOLPHINS NMB VETERINARY VACCINES 30023000 VVC0ZZ VETERINARY VACCINE - VETERINARY BIOLOGICS 30029000 VVP0B0COWRUMB COWDRIA RUMINANTIUM - 30029000 VVP0B2AERHYDB AEROMONAS HYDROPHILA - 30029000 VVP0B2ANAMARB ANAPLASMA MARGINALE - 30029000 VVP0B2BORBURB BORRELIA BURGDORFERI - 30029000 VVP0B2CAMFETV CAMPYLOBACTER FETUS SUBSP. -

(12) Patent Application Publication (10) Pub. No.: US 2012/0009150 A1 WEBER Et Al
US 2012O009 150A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0009150 A1 WEBER et al. (43) Pub. Date: Jan. 12, 2012 (54) DIARYLUREAS FORTREATINGVIRUS Publication Classification INFECTIONS (51) Int. Cl. (76) Inventors: Olaf WEBER, Wulfrath (DE); st 2. CR Bernd Riedl, Wuppertal (DE) ( .01) A63/675 (2006.01) (21) Appl. No.: 13/236,865 A6II 3/522 (2006.01) A6IP 29/00 (2006.01) (22) Filed: Sep. 20, 2011 A6II 3/662 (2006.01) A638/14 (2006.01) Related U.S. Application Data A63L/7056 (2006.01) A6IP3L/2 (2006.01) (63) Continuation of application No. 12/097.350. filed on A6II 3/44 (2006.01) Nov. 3, 2008, filed as application No. PCTAEPO6/ A6II 3/52 (2006.01) 11693 on Dec. 6, 2006. O O (52) U.S. Cl. .......... 424/85.6; 514/350; 514/171; 514/81; (30) Foreign Application Priority Data 514/263.38: 514/263.4: 514/120: 514/4.3: Dec. 15, 2005 (EP) .................................. 05O274513 424/85.7; 514/43 Dec. 15, 2005 (EP). ... O5O27452.1 Dec. 15, 2005 (EP). ... O5O27456.2 Dec. 15, 2005 (EP). ... O5O27458.8 The present invention relates to pharmaceutical compositions Dec. 15, 2005 (EP) O5O27.460.4 for treating virus infections and/or diseases caused by virus Dec. 15, 2005 (EP) O5O27462.O infections comprising at least a diary1 urea compound option Dec. 15, 2005 (EP). ... O5O27465.3 ally combined with at least one additional therapeutic agent. Dec. 15, 2005 (EP). ... O5O274.67.9 Useful combinations include e.g. BAY 43-9006 as a diaryl Dec. -

"Fischgesundheit Und Fischerei Im Wandel Der Zeit"
Fischgesundheit und Fischerei im Wandel der Zeit Tagungsband XV. Gemeinschaftstagung der Deutschen, Österreichischen und Schweizer Sektionen der European Association of Fish Pathologists (EAFP) Starnberg, 8. – 10. Oktober 2014 Die Tagung wurde in wesentlichen Teilen finanziert vom Bayerischen Staatsministerium für Ernährung, Landwirtschaft und Forsten (StMELF) aus der Fischereiabgabe Bayerns Weitere Unterstützung erfolgte durch: ― Niedersächsisches Landesamt für Verbraucherschutz und Lebensmittelsicherheit ― Bayerische Landesanstalt für Landwirtschaft, Institut für Fischerei ― MSD Tiergesundheit, Intervet Deutschland GmbH ― Zentralverband Zoologischer Fachbetriebe (ZZF) und Wirtschaftsgemeinschaft Zoolo- gischer Fachbetriebe GmbH (WZF) ― Familie Gerda und Hartmut Stachowitz ― Oswald Fürneisen ― Tetra GmbH, Melle ― BioMar Group Für die Erstellung des Tagungsbandes wurden die von den Autoren eingesandten Manu- skripte bzw. Zusammenfassungen verwendet. Für die Inhalte und Abbildungen sind die Autoren verantwortlich. Einige Beiträge wurden oder werden an anderer Stelle veröffent- licht. Im vorliegenden Tagungsband sind Zusammenfassungen dieser Beiträge veröffent- licht. Zitiervorschlag KLEINGELD, D. W., und WEDEKIND, H. (Hrsg.) (2015): Fischgesundheit und Fische- rei im Wandel der Zeit. XV. Gemeinschaftstagung der Deutschen, Österreichischen und Schweizer Sektion der European Association of Fish Pathologists (EAFP), 8. – 10. Okto- ber 2014 an der LfL in Starnberg. Impressum Herausgeber: Bayerische Landesanstalt für Landwirtschaft, Vöttinger -

Shedding of the Salmonid Herpesvirus-3 by Infected Lake Trout (Salvelinus Namaycush)
viruses Communication Shedding of the Salmonid Herpesvirus-3 by Infected Lake Trout (Salvelinus namaycush) Mohamed Faisal 1,2,3, Mochamad Purbayu 3, Megan A. Shavalier 2,3, Terence L. Marsh 4 and Thomas P. Loch 1,2,* 1 Department of Pathobiology and Diagnostic Investigation, College of Veterinary Medicine, Michigan State University, East Lansing, MI 48824, USA 2 Department of Fisheries and Wildlife, College of Agriculture and Natural Resources, Michigan State University, East Lansing, MI 48824, USA 3 Comparative Medicine and Integrative Biology, College of Veterinary Medicine, Michigan State University, East Lansing, MI 48824, USA 4 Department of Microbiology and Molecular Genetics, College of Natural Science, Michigan State University, East Lansing, MI 48824, USA * Correspondence: [email protected]; Tel.: +517-884-2019; Fax: +517-432-2310 Received: 9 May 2019; Accepted: 20 June 2019; Published: 26 June 2019 Abstract: Salmonid Herpesvirus-3, commonly known as the Epizootic Epitheliotropic Disease virus (EEDV), causes a disease of lake trout (Salvelinus namaycush) that has killed millions of fish over the past several decades. Currently, most aspects of EEDV disease ecology remain unknown. In this study, we investigated EEDV shedding in experimentally challenged (intracoelomic injection) lake trout that were individually microchipped. In order to assess viral shedding, each infected fish was placed in individual static, aerated aquaria for a period of 8 h, after which the water was assessed for the presence of EEDV DNA using quantitative PCR. Water sampling was conducted every seven days for 93 days post-infection (pi), followed by additional sampling after one year. Results demonstrated that lake trout began shedding EEDV into the water as early as 9 days pi. -

Herpes Virus Infection Associated with Interstitial Nephritis in a Beaked
Arbelo et al. BMC Veterinary Research 2012, 8:243 http://www.biomedcentral.com/1746-6148/8/243 RESEARCH ARTICLE Open Access Herpes virus infection associated with interstitial nephritis in a beaked whale (Mesoplodon densirostris) Manuel Arbelo1, Edwige N Bellière2, Eva Sierra1, Simona Sacchinni1, Fernando Esperón2, Marisa Andrada1, Miguel Rivero1, Josue Diaz-Delgado1 and Antonio Fernández1* Abstract Background: The capacity for herpesvirus to cause disease in cetaceans is unclear and may be varied depending on the different conditions of individuals and between different species. Kidney pathology and intralesional virus-associated infection have been rarely reported in cetaceans. Result: On April 2004, an old adult male Blainville’s beaked whale (Mesoplodon densirostris) 420 cm long with a poor body condition was stranded on Tenerife Island. During necropsy, no gross lesions were observed in the kidneys. However, membranous glomerulonephritis, multifocal interstitial lymphoplasmacytic nephritis and acute multifocal necrotizing tubulointerstitial nephritis with intranuclear inclusion bodies was diagnosed by histological analysis. Tissue samples were submitted for bacteriological analysis and molecular viral screening. Conclusion: A novel alpha herpesvirus associated with interstitial nephritis was identified in an old adult male Blainville's beaked whale (M. densirostris) with a poor body condition stranded in the Canary Islands. This report suggests that identification of herpesvirus infection could be used as a differential diagnosis for interstitial nephritis in cetaceans. Keywords: Beaked whale, Interstitial nephritis, Alpha herpes virus, Diagnosis Background [8]. Gamma-HV have been identified in mucosal lesions in The presence of herpesviruses (HV) in cetaceans was bottlenose dolphins, Risso’sdolphins(Grampus griseus), shown in the late 1980s by electron microscopy (EM) ana- dwarf sperm whales (Kogia sima) and Blainville’s beaked lysis demonstrating HV-like particles in skin biopsies from whales (Mesoplodon densirostris) [8-10]. -

Cyprinid Herpesvirus 3
1 © 2015. This manuscript version is made available under the CC-BY-NC-ND 4.0 license 2 http://creativecommons.org/licenses/by-nc-nd/4.0/ 3 doi:10.1016/bs.aivir.2015.03.001 4 Running title: Cyprinid herpesvirus 3 5 Title: Cyprinid herpesvirus 3, an archetype of fish alloherpesviruses 6 Authors and Affiliations 7 Maxime Boutier 1, Maygane Ronsmans 1, Krzysztof Rakus 1, Joanna Jazowiecka-Rakus 1, 8 Catherine Vancsok 1, Léa Morvan 1, Ma. Michelle D. Peñaranda 1, David M. Stone 2, Keith 9 Way 2, Steven J. van Beurden 3, Andrew J. Davison 4 and Alain Vanderplasschen 1* 10 11 1 Immunology-Vaccinology (B43b), Department of Infectious and Parasitic Diseases, 12 Fundamental and Applied Research for Animals & Health (FARAH), Faculty of Veterinary 13 Medicine, University of Liège, B-4000 Liège, Belgium. 14 2 The Centre for Environment, Fisheries and Aquaculture Science, Weymouth Laboratory, 15 Barrack Road, The Nothe, Weymouth, Dorset DT4 8UB, United Kingdom. 16 3 Department of Pathobiology, Faculty of Veterinary Medicine, Utrecht University, Yalelaan 17 1, 3584CL Utrecht, The Netherlands. 18 4 MRC - University of Glasgow Centre for Virus Research, 8 Church Street, Glasgow G11 19 5JR, United Kingdom. 20 21 22 * Corresponding author. Mailing address: Immunology-Vaccinology (B43b), Department of 23 Infectious and Parasitic Diseases, Faculty of Veterinary Medicine, University of Liège, 24 B-4000 Liège, Belgium. Phone: 32-4-366 42 64 - Fax: 32-4-366 42 61 25 E-mail: [email protected] 26 Author’s contacts (see affiliations above) 27 28 Maxime Boutier: [email protected] ; +32 4 366 42 66 29 Maygane Ronsmans: [email protected] ; +32 4 366 42 66 30 Krzysztof Rakus: [email protected] ; +32 4 366 42 66 31 Joanna Jazowiecka-Rakus: [email protected] ; +32 4 366 42 66 32 Catherine Vancsok: [email protected] ; +32 4 366 42 66 33 Léa Morvan: [email protected] ; +32 4 366 42 66 34 Ma. -

Fish Herpesvirus Diseases
ACTA VET. BRNO 2012, 81: 383–389; doi:10.2754/avb201281040383 Fish herpesvirus diseases: a short review of current knowledge Agnieszka Lepa, Andrzej Krzysztof Siwicki Inland Fisheries Institute, Department of Fish Pathology and Immunology, Olsztyn, Poland Received March 19, 2012 Accepted July 16, 2012 Abstract Fish herpesviruses can cause significant economic losses in aquaculture, and some of these viruses are oncogenic. The virion morphology and genome organization of fish herpesviruses are generally similar to those of higher vertebrates, but the phylogenetic connections between herpesvirus families are tenuous. In accordance with new taxonomy, fish herpesviruses belong to the family Alloherpesviridae in the order Herpesvirales. Fish herpesviruses can induce diseases ranging from mild, inapparent infections to serious ones that cause mass mortality. The aim of this work was to summarize the present knowledge about fish herpesvirus diseases. Alloherpesviridae, CyHV-3, CyHV-2, CyHV-1, IcHV-1, AngHV-1 Herpesviruses comprise a numerous group of large DNA viruses with common virion structure and biological properties (McGeoch et al. 2008; Mattenleiter et al. 2008). They are host-specific pathogens. Apart from three herpesviruses found recently in invertebrate species, all known herpesviruses infect vertebrates, from fish to mammals (Davison et al. 2005a; Savin et al. 2010). According to a new classification accepted by the International Committee on Taxonomy of Viruses (http:/ictvonline.org), all herpesviruses have been incorporated into a new order named Herpesvirales, which has been split into three families. The revised family Herpesviridae contains mammalian, avian, and reptilian viruses; the newly-created family Alloherpesviridae contains herpesviruses of fish and amphibians, and the new family Malacoherpesviridae comprises single invertebrate herpesvirus (Ostreid herpesvirus). -

The Role of Viral Glycoproteins and Tegument Proteins in Herpes
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School 2014 The Role of Viral Glycoproteins and Tegument Proteins in Herpes Simplex Virus Type 1 Cytoplasmic Virion Envelopment Dmitry Vladimirovich Chouljenko Louisiana State University and Agricultural and Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the Veterinary Pathology and Pathobiology Commons Recommended Citation Chouljenko, Dmitry Vladimirovich, "The Role of Viral Glycoproteins and Tegument Proteins in Herpes Simplex Virus Type 1 Cytoplasmic Virion Envelopment" (2014). LSU Doctoral Dissertations. 4076. https://digitalcommons.lsu.edu/gradschool_dissertations/4076 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. THE ROLE OF VIRAL GLYCOPROTEINS AND TEGUMENT PROTEINS IN HERPES SIMPLEX VIRUS TYPE 1 CYTOPLASMIC VIRION ENVELOPMENT A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The Interdepartmental Program in Veterinary Medical Sciences through the Department of Pathobiological Sciences by Dmitry V. Chouljenko B.Sc., Louisiana State University, 2006 August 2014 ACKNOWLEDGMENTS First and foremost, I would like to thank my parents for their unwavering support and for helping to cultivate in me from an early age a curiosity about the natural world that would directly lead to my interest in science. I would like to express my gratitude to all of the current and former members of the Kousoulas laboratory who provided valuable advice and insights during my tenure here, as well as the members of GeneLab for their assistance in DNA sequencing. -

Viruses Status January 2013 FOEN/FOPH 2013 1
Classification of Organisms. Part 2: Viruses Status January 2013 FOEN/FOPH 2013 1 Authors: Prof. Dr. Riccardo Wittek, Dr. Karoline Dorsch-Häsler, Julia Link > Classification of Organisms Part 2: Viruses The classification of viruses was first published in 2005 and revised in 2010. Classification of Organisms. Part 2: Viruses Status January 2013 FOEN/FOPH 2013 2 Name Group Remarks Adenoviridae Aviadenovirus (Avian adenoviruses) Duck adenovirus 2 TEN Duck adenovirus 2 2 PM Fowl adenovirus A 2 Fowl adenovirus 1 (CELO, 112, Phelps) 2 PM Fowl adenovirus B 2 Fowl adenovirus 5 (340, TR22) 2 PM Fowl adenovirus C 2 Fowl adenovirus 10 (C-2B, M11, CFA20) 2 PM Fowl adenovirus 4 (KR-5, J-2) 2 PM Fowl adenovirus D 2 Fowl adenovirus 11 (380) 2 PM Fowl adenovirus 2 (GAL-1, 685, SR48) 2 PM Fowl adenovirus 3 (SR49, 75) 2 PM Fowl adenovirus 9 (A2, 90) 2 PM Fowl adenovirus E 2 Fowl adenovirus 6 (CR119, 168) 2 PM Fowl adenovirus 7 (YR36, X-11) 2 PM Fowl adenovirus 8a (TR59, T-8, CFA40) 2 PM Fowl adenovirus 8b (764, B3) 2 PM Goose adenovirus 2 Goose adenovirus 1-3 2 PM Pigeon adenovirus 2 PM TEN Turkey adenovirus 2 TEN Turkey adenovirus 1, 2 2 PM Mastadenovirus (Mammalian adenoviruses) Bovine adenovirus A 2 Bovine adenovirus 1 2 PM Bovine adenovirus B 2 Bovine adenovirus 3 2 PM Bovine adenovirus C 2 Bovine adenovirus 10 2 PM Canine adenovirus 2 Canine adenovirus 1,2 2 PM Caprine adenovirus 2 TEN Goat adenovirus 1, 2 2 PM Equine adenovirus A 2 Equine adenovirus 1 2 PM Equine adenovirus B 2 Equine adenovirus 2 2 PM Classification of Organisms. -

Supporting Information
Supporting Information Wu et al. 10.1073/pnas.0905115106 20 15 10 5 0 10 15 20 25 30 35 40 Fig. S1. HGT cutoff and tree topology. Robinson-Foulds (RF) distance [Robinson DF, Foulds LR (1981) Math Biosci 53:131–147] between viral proteome trees with different horizontal gene transfer (HGT) cutoffs h at feature length 8. Tree distances are between h and h-1. The tree topology remains stable for h in the range 13–31. We use h ϭ 20 in this work. Wu et al. www.pnas.org/cgi/content/short/0905115106 1of6 20 18 16 14 12 10 8 6 0.0/0.5 0.5/0.7 0.7/0.9 0.9/1.1 1.1/1.3 1.3/1.5 Fig. S2. Low complexity features and tree topology. Robinson-Foulds (RF) distance between viral proteome trees with different low-complexity cutoffs K2 for feature length 8 and HGT cutoff 20. The tree topology changes least for K2 ϭ 0.9, 1.1 and 1.3. We choose K2 ϭ 1.1 for this study. Wu et al. www.pnas.org/cgi/content/short/0905115106 2of6 Table S1. Distribution of the 164 inter-viral-family HGT instances bro hr RR2 RR1 IL-10 Ubi TS Photol. Total Baculo 45 1 10 9 11 1 77 Asco 11 7 1 19 Nudi 1 1 1 3 SGHV 1 1 2 Nima 1 1 2 Herpes 48 12 Pox 18 8 2 3 1 3 35 Irido 1 1 2 4 Phyco 2 3 2 1 8 Allo 1 1 2 Total 56 8 35 24 6 17 14 4 164 The HGT cutoff is 20 8-mers. -

Taxonomy Bovine Ephemeral Fever Virus Kotonkan Virus Murrumbidgee
Taxonomy Bovine ephemeral fever virus Kotonkan virus Murrumbidgee virus Murrumbidgee virus Murrumbidgee virus Ngaingan virus Tibrogargan virus Circovirus-like genome BBC-A Circovirus-like genome CB-A Circovirus-like genome CB-B Circovirus-like genome RW-A Circovirus-like genome RW-B Circovirus-like genome RW-C Circovirus-like genome RW-D Circovirus-like genome RW-E Circovirus-like genome SAR-A Circovirus-like genome SAR-B Dragonfly larvae associated circular virus-1 Dragonfly larvae associated circular virus-10 Dragonfly larvae associated circular virus-2 Dragonfly larvae associated circular virus-3 Dragonfly larvae associated circular virus-4 Dragonfly larvae associated circular virus-5 Dragonfly larvae associated circular virus-6 Dragonfly larvae associated circular virus-7 Dragonfly larvae associated circular virus-8 Dragonfly larvae associated circular virus-9 Marine RNA virus JP-A Marine RNA virus JP-B Marine RNA virus SOG Ostreid herpesvirus 1 Pig stool associated circular ssDNA virus Pig stool associated circular ssDNA virus GER2011 Pithovirus sibericum Porcine associated stool circular virus Porcine stool-associated circular virus 2 Porcine stool-associated circular virus 3 Sclerotinia sclerotiorum hypovirulence associated DNA virus 1 Wallerfield virus AKR (endogenous) murine leukemia virus ARV-138 ARV-176 Abelson murine leukemia virus Acartia tonsa copepod circovirus Adeno-associated virus - 1 Adeno-associated virus - 4 Adeno-associated virus - 6 Adeno-associated virus - 7 Adeno-associated virus - 8 African elephant polyomavirus -

Herpesvirus Systematics§ Andrew J
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Veterinary Microbiology 143 (2010) 52–69 Contents lists available at ScienceDirect Veterinary Microbiology journal homepage: www.elsevier.com/locate/vetmic Herpesvirus systematics§ Andrew J. Davison * MRC Virology Unit, Institute of Virology, University of Glasgow, Church Street, Glasgow G11 5JR, UK ARTICLE INFO ABSTRACT Keywords: This paper is about the taxonomy and genomics of herpesviruses. Each theme is presented Herpesvirus as a digest of current information flanked by commentaries on past activities and future Classification directions. Genomics The International Committee on Taxonomy of Viruses recently instituted a major Herpes simplex virus update of herpesvirus classification. The former family Herpesviridae was elevated to a new Human cytomegalovirus order, the Herpesvirales, which now accommodates 3 families, 3 subfamilies, 17 genera and 90 species. Future developments will include revisiting the herpesvirus species definition and the criteria used for taxonomic assignment, particularly in regard to the possibilities of classifying the large number of herpesviruses detected only as DNA sequences by polymerase chain reaction. Nucleotide sequence accessions in primary databases, such as GenBank, consist of the sequences plus annotations of the genetic features. The quality of these accessions is important because they provide a knowledge base that is used widely by the research community. However, updating the accessions to take account of improved knowledge is essentially reserved to the original depositors, and this activity is rarely undertaken. Thus, the primary databases are likely to become antiquated. In contrast, secondary databases are open to curation by experts other than the original depositors, thus increasing the likelihood that they will remain up to date.