Cervical Spine Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Seat-Belt Injuries in Children Involved in Motor Vehicle Crashes
Original Article Article original Seat-belt injuries in children involved in motor vehicle crashes Miriam Santschi, MD;* Vincent Echavé, MD;† Sophie Laflamme, MD;* Nathalie McFadden, MD;† Claude Cyr, MD* Background: The efficacy of seat belts in reducing deaths from motor vehicle crashes is well docu- mented. A unique association of injuries has emerged in adults and children with the use of seat belts. The “seat-belt syndrome” refers to the spectrum of injuries associated with lap-belt restraints, particu- larly flexion-distraction injuries to the spine (Chance fractures). Methods: We describe the injuries sus- tained by 8 children, including 2 sets of twins, in 3 different motor vehicle crashes. Results: All children were rear seat passengers wearing lap or 3-point restraints. All had abdominal lap-belt ecchymosis and multiple abdominal injuries due to the common mechanism of seat-belt compression with hyperflexion and distraction during deceleration. Five of the children had lumbar spine fractures and 4 remained permanently paraplegic. Conclusions: These incidents illustrate the need for acute awareness of the complete spectrum of intra-abdominal and spinal injuries in restrained pediatric passengers in motor vehicle crashes and for rear seat restraints that include shoulder belts with the ability to adjust them to fit smaller passengers, including older children. Contexte : L’efficacité des ceintures de sécurité pour réduire le nombre des décès causés par les colli- sions de véhicules à moteur est bien documentée. On a toutefois relevé une association particulière entre certains traumatismes et le port de la ceinture de sécurité chez les adultes et les enfants. Le «syndrome de la ceinture de la sécurité» désigne l’éventail des traumatismes associés aux ceintures ventrales, et en particulier les traumatismes de flexion-distraction de la colonne (fractures de Chance). -

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

Treatment of Comminuted Fractures of the Base of the Thumb Metacarpal Using a Cemented Bone-K-Wire Frame
Hand Surgery and Rehabilitation 38 (2019) 44–51 Available online at ScienceDirect www.sciencedirect.com Original article Treatment of comminuted fractures of the base of the thumb metacarpal using a cemented bone-K-wire frame Traitement des fractures comminutives de la base du premier me´tacarpien graˆce a` un cadre os-broches-ciment W. Duan, X. Zhang, Y. Yu, Z. Zhang *, X. Shao, W. Du Department of Hand Surgery, Third Hospital of Hebei Medical University, Shijiazhuang, Hebei 050051, PR China ARTICLE INFO ABSTRACT Article history: We aimed to describe the treatment of comminuted fractures of the base of the thumb metacarpal using a Received 13 June 2018 cemented bone-K-wire frame. Between March 2010 and January 2016, 41 fractures of the base of the thumb Received in revised form 8 August 2018 were treated using a cemented bone-K-wire frame. The mean age of the patients was 34 years. The patients’ Accepted 7 September 2018 history included a fall onto the hand in 7 cases, direct trauma in 31 cases, and polytrauma with an unclear Available online 11 October 2018 mechanism of injury in 3 cases. At the final follow-up, hand grip and pinch strength were measured using a dynamometer. All measurements were compared with those of the opposite hand. The patients were assessed Keywords: functionally using the Smith and Cooney score.All K-wires were left in place until the bone healed. Bone healing Cemented K-wire frame was achieved in all thumbs in an average of 5.2 weeks. Follow-up averaged 27 months. The mean hand pinch External fixator Rolando fracture andgripstrengthwas8.7 kg Æ 2.4 kgand38.4 kg Æ 5.9 kg,respectively.Themeanmeasurementsontheopposite Thumb side were 9.2 kg Æ 2.5 kg and 40.2 kg Æ 6.6 kg, respectively. -

Pseudogout at the Knee Joint Will Frequently Occur After Hip Fracture
Harato and Yoshida Journal of Orthopaedic Surgery and Research (2015) 10:4 DOI 10.1186/s13018-014-0145-9 RESEARCH ARTICLE Open Access Pseudogout at the knee joint will frequently occur after hip fracture and lead to the knee pain in the early postoperative period Kengo Harato1,3*† and Hiroki Yoshida2† Abstract Background: Symptomatic knee joint effusion is frequently observed after hip fracture, which may lead to postoperative knee pain during rehabilitation after hip fracture surgery. However, unfortunately, very little has been reported on this phenomenon in the literature. The purpose of the current study was to investigate the relationship between symptomatic knee effusion and postoperative knee pain and to clarify the reason of the effusion accompanied by hip fracture. Methods: A total of 100 patients over 65 years of age with an acute hip fracture after fall were prospectively followed up. Knee effusion was assessed on admission and at the operating room before the surgery. If knee effusion was observed at thetimeofthesurgery,synovialfluidwascollectedintosyringes to investigate the cause of the effusion using a compensated polarized light microscope. Furthermore, for each patient, we evaluated age, sex, radiographic knee osteoarthritis (OA), type of the fracture, laterality, severity of the fracture, and postoperative knee pain during rehabilitation. These factors were compared between patients with and without knee effusion at the time of the surgery. As a statistical analysis, we used Mann–Whitney U-test for patients’ age and categorical variables were analyzed by chi-square test or Fisher’sexacttest. Results: A total of 30 patients presented symptomatic knee effusion at the time of the surgery. -
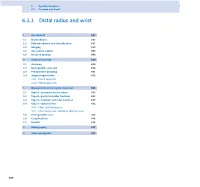
6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -

8. T. Wood the Pediatric Trauma Patient
9/9/2019 History ● Halifax 1917 ● French cargo ship with explosives collided with Norwegian ship ○ Dr. William Ladd distressed by pediatric patients ■ Treated similarly to adults ● Different anatomic, physiologic, surgical conditions ● 1970s The Pediatric Trauma Patient ○ First pediatric shock trauma unit at Johns Hopkins ● 2010 ○ Pediatric trauma centers: 43 ■ 2015: 136 1 Tessa Woods, DO, FACOS ○ Adult trauma centers (Level 1/2): 474 1. Pediatric Trauma Centers, A Report to Congressional Requesters. 2017 History ● One million children killed per year ○ 10,000,000 to 30,000,000 nonfatal injuries per year ○ US: 12,000 die, 1,000,000 nonfatal ● Injuries are leading cause of death age 1-19 ● C. Everett Koop, former pediatric surgeon and US Surgeon General: ○ “If a disease were killing our children at the rate unintentional injuries are, the public would be outraged and demand that this killer be stopped.” Injury Patterns Location Matters ● Infants ● 30% of children lack access to a pediatric trauma facility ○ inflicted trauma, abusive ○ Many go to those who have SOME training in pediatrics ● Age 1-4 ○ Fall ● Age 5-9 “Children are not just little adults” ○ Pedestrian injuries ● Age 10-14 ○ Motor vehicle 1 9/9/2019 Initial Evaluation Initial Evaluation ● Initial workup the same: ABC ● Less than 40 kg ○ MCC Preventable prehospital cause of death: ● Broselow Emergency Tape ■ Airway Obstruction ○ Fluids ○ Prehospital cpr: poor prognosis ○ Drugs 1 ■ 25 children reviewed, blunt injury with prehospital cpr: no survival ○ Vital Signs ● Majority from lethal CNS injury ○ Equipment sizes ○ Beware: ■ May underestimate weight ● By 2.6kg on average 1. Calkins CM, Bensard DD, Patrick DA, Karrer FM. -

Approach to Hand Conditions
Approach to Hand Conditions Alphonsus Chong Associate Professor, Department of Orthopaedic Surgery, Singapore Senior Consultant, Department of Hand and Reconstructive Microsurgery, Singapore http://bit.ly/39fuCIK [email protected] Scope • Introduction – Slides at http://bit.ly/39fuCIK • And other material at: https://nus.edu/2Mh4e4s • Physical examination http://bit.ly/39fuCIK : these slides • Traumatic injuries – open and closed • Peripheral nerve problems • Masses in the hand and wrist • Tendinopathy and tendinitis • Deformity https://nus.edu/2Mh4e4s: hand wiki 3 History Taking • Pain – different aspects • Handedness • Deformity • Job v – Congenital • Hobbies – Acquired - ? Traumatic • Previous injury/ surgery • Decreased rangev of motion • Weakness • For acute trauma/conditions: • Numbness – Last meal v • Others e.g. triggering, instability – Mechanism of injury – Time/date of injury Expose both sides: subcutaneous border Scars, wasting, deformity of ulna and elbow- rheumatoid nodules Completeness and fluidity of motion Scars, wasting, deformity Quick Nerve Screen Median Nerve Radial Nerve Ulnar nerve Traumatic Injuries – Open Injuries Open traumatic injuries are a staple work of hand surgeons. Assessment of Hand – Work through the tissues (see Apley) • Skin – note size and types of wounds • Vessels - circulation • Nerves – sensation and motor • Muscle and Tendons – individual flexor and extensor tendon testing • Bones & Joints – appropriate x-rays to assess fractures/ dislocation What do you see? • LOOK • LOOK – Loss of cascade • -

Ortho Trauma
Pediatric Orthopedic/ Trauma Nursing, pg 1 of 11 Developmental Differences • Immature Immune System • have less ability to wall off an infection and keep it in one place in the body, less ability to fight off infection • Bone Structure/Function • More flexible/porous: more incomplete fractures in kids than adults • Periosteum stronger/tougher: incomplete fx • Epiphyseal growth plates: fx to a growth plate is a big deal in a kid, leads to growth probs • Faster healing: d/t rich blood supply to bones • Remodeling ability: bones grow until about age 20 • Cartilage is soft, lots of cartilage on ends of long bones b/c still growing Epiphyseal Growth Plate • Layer of cartilage between epiphysis and metaphysis • Controls long bone growth • New cartilage converted to bone • Disruption affects growth • This area is more vulnerable than injury; even muscles and tendons can be stronger than bones; under pressure, the growth plate can “slip”. Infections • Osteomyelitis • Rich vascular supply • Hematogenous origin 80-90% • 1/3 have history of minor trauma • Metaphysis long bone most common • Risk joint involvement • More common in kids ?? years of age (not in slides, and I didn’t catch what she said) • More common in males > females • Often follows URI and minor trauma to the bone (fell down and bruised) • More common in the long bones...big concern if it gets into the joint • Patho: Infection goes into bone, causes inflammation and swelling, then you get decrease in blood flow to the cells and this leads to necrosis in the bone. • Osteomyelitis: -

Bimalleolar Ankle Fracture Fixation of a 13-Year-Old Patient with Two Activascrew™ LAG Bioabsorbable Screws
Bimalleolar ankle fracture fixation of a 13-year-old patient with two ActivaScrew™ LAG bioabsorbable screws. Pierre Lascombes Professor, M.D., Ph.D. For medical professional use, not public. © 2020 Bioretec Ltd. and Prof. Lascombes. All rights reserved. Table of Contents Summary Table ........................................................................................................... 3 1 Case Description .................................................................................................. 4 2 Implants and operative technique ......................................................................... 5 3 Outcome ............................................................................................................... 7 4 Contact Information Concerning the Case ............................................................ 8 For medical professional use, not public Page 2 / 8 © 2020 Bioretec Ltd., Prof. Lascombes. All rights reserved. Summary Table Demographics Patient number: P01 Patient Initials: NX Smoking: No Sex: Female Use of alcohol: No Age: 13 Years Systemic disease: No Height: 158 cm Cont. Medication: No Weight: 40 kg Case description Diagnosis: Dislocation right ankle - bimalleolar fracture Cause of injury: Gymnastic injury Operation Operator: Lascombes Operation year: 2016 Note: Immediate reduction of the Operation description: Open reduction of medial malleolus and fixation with TWO resorbable screws dislocation at emergenry room - ketamine. Surgical treatment 5 hours Operation time:h57 min Immobilisation -

Treatment of Common Hip Fractures: Evidence Report/Technology
This report is based on research conducted by the Minnesota Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290 2007 10064 1). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This report may be used, in whole or in part, as the basis for the development of clinical practice guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage policies. AHRQ or U.S. Department of Health and Human Services endorsement of such derivative products may not be stated or implied. Evidence Report/Technology Assessment Number 184 Treatment of Common Hip Fractures Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290 2007 10064 1 Prepared by: Minnesota Evidence-based Practice Center, Minneapolis, Minnesota Investigators Mary Butler, Ph.D., M.B.A. Mary Forte, D.C. Robert L. Kane, M.D. Siddharth Joglekar, M.D. Susan J. Duval, Ph.D. Marc Swiontkowski, M.D. -

Effect of Manual Reduction and Indirect Decompression on Thoracolumbar Burst Fracture: a Comparison Study
Effect of manual reduction and indirect decompression on thoracolumbar burst fracture: a comparison study Jian Huang ( [email protected] ) Haikou Hospital of Traditional Chinese Medicine https://orcid.org/0000-0002-5434-1148 Limin Zhou Haikou Hospital of Traditional Chinese Medicine Zhaodong Yan Shaoxing Hospital of Traditional Chinese Medicine Zongbo Zhou Haikou Hospital of Traditional Chinese Medicine Xuejian Gou Haikou Hospital of Traditional Chinese Medcine Research article Keywords: Manipulative reduction, Indirect decompression, Thoracolumbar burst fractures Posted Date: October 14th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-90414/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on November 13th, 2020. See the published version at https://doi.org/10.1186/s13018-020-02075-w. Page 1/16 Abstract Study design Retrospective cohort study. Objective To evaluate the effect of manual reduction and indirect decompression on thoracolumbar burst fracture. Methods 60 patients with thoracolumbar burst fracture who were hospitalized from January 2018 to October 2019 were selected and divided into experimental group (33 cases) and control group (27 cases) according to different treatment methods. The experimental group was treated with manual reduction and indirect decompression, while the control group was not treated with manual reduction. The operation time and intraoperative blood loss were recorded. VAS score was used to evaluate the improvement of pain. The anterior height of injured vertebra, wedge angle of injured vertebral body, encroachment ratio of injured vertebral canal were used to evaluate spinal canal decompression and fracture reduction. -

Listen to the Associated Podcast Episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, Available at Theradiologyreview.Com O
MSK: Fractures for Radiology Board Study, Matt Covington, MD Listen to the associated podcast episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, available Listen to associated Podcast episodes: ABR Core Exam, Multisystemic Diseases Parts 1-3, available at at theradiologyreview.com or on your favorite podcast directory. Copyrighted. theradiologyreview.com or on your favorite podcast direcry. Fracture resulting From abnormal stress on normal bone = stress Fracture Fracture From normal stress on abnormal bone = insuFFiciency Fracture Scaphoid Fracture site with highest risk for avascular necrosis (proximal or distal)? Proximal pole scaphoid Fractures are at highest risk For AVN Comminuted Fracture at the base oF the First metacarpal = Rolando Fracture Non-comminuted Fracture at base oF the First metacarpal = Bennett Fracture The pull oF which tendon causes the dorsolateral dislocation in a Bennett fracture? The abductor pollicus longus tendon. Avulsion Fracture at the base oF the proximal phalanx with ulnar collateral ligament disruption = Gamekeeper’s thumb. Same Fracture but adductor tendon becomes caught in torn edge oF the ulnar collateral ligament? Stener’s lesion. IF Stener’s lesion is present this won’t heal on its own so you need surgery. You shouldn’t image a Gamekeeper’s thumb with stress views because you can convert it to a Stener’s lesion. Image with MRI instead. Distal radial Fracture with dorsal angulation = Colle’s Fracture (C to D= Colle’s is Dorsal) Distal radial Fracture with volar angulation = Smith’s Fracture (S