Fracture Lower Extremity Part II
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Surgical Repair of Transverse Patella Fractures
A vertical patella fracture James Heilman, MD The Surgical Repair of Transverse Patella Fractures Angela Miller, cst Patella fractures constitute about 1% of all fractures, and are mostly caused by direct trauma to the front of the knee.1 There are many types of patella fractures: comminuted, open, nondisplaced and displaced. This article will focus on the about 50% to 80% of patellar fractures that are transverse,3 and requires the surgical treatment using Kirschner wires, also known as K-wires and tension-band wiring. ANATOMY AND PHYSIOLOGY LEARNING OBJECTIVES The patella is the largest sesamoid bone in the human body. Sesamoid ▲ Learn about the use of K-wires for bones are not connected to other bones; instead, they are connected treatment of this fracture by tendons or are embedded in muscle tissue. The patella bone can ▲ Review the anatomy related to this be found in the quadriceps tendons. The function of sesamoid bones is to provide a smooth surface over which the tendon can slide, and procedure increases the ability of the tendons to transmit muscle forces.2 The ▲ Recall the patient preparation patella bone is located anterior to the knee joint, and the posterior sur- specific to this operation face articulates with the femur. It is attached proximally to the femoral ▲ Examine the role of the surgical condyles, and attached distally to the condyles of the tibia and upper technologist during a transverse ends of the fibula.5 patella fracture ▲ Read about studies comparing the POSITIONING use of metallic versus nonmetallic During transverse patella fractures a patient will be placed in the implants supine position, with their arms are placed at each of their sides and A vertical patella fracture James Heilman, MD AUGUST 2016 | The Surgical Technologist | 349 tucked by the draw sheet. -

Vertical Open Patella Fracture, Treatment, Rehabilitation and the Moment to Fixation
Elmer ress Case Report J Clin Med Res. 2015;7(2):129-133 Vertical Open Patella Fracture, Treatment, Rehabilitation and the Moment to Fixation Joao Alberto Larangeiraa, Liliane Bellenziera, Vanessa da Silva Rigoa, Elias Josue Ramos Netoa, Francisco Fritsch Machry Kruma, Tiango Aguiar Ribeiroa, b, c Abstract Introduction Patella fracture is relatively uncommon and the vertical trace frac- Patella fracture is relatively uncommon and represents approx- ture represents almost 12-17%. The open patella fracture expresses imately 0.5-1.5% of all bone injuries [1, 2], and men are more 6-30%. The association of these two uncommon conditions was the affected than women [3, 4]. The classification can be done by aim of this case report even as the treatment and the moment of fixa- characterizing the fracture pattern in osteochondral, multifrag- tion (definitive surgical treatment). A 27-year-old man after a motor- mented, stellate, transversal, vertical and polar fracture (Fig. cycle accident showed an open patella fracture classified as a Gustilo 1). Other classifications may take into account the presence of and Anderson type IIIA lesion. The patient was immediately treated deviation between the fragments, deviated and not deviated, with precocious surgery fixation with a modified tension band which and the mechanism of injury. The transversal type is more fre- consists of two parallel K-wires positioned orthogonal to the fracture quent corresponding to 50-80%, comminuted 30-35% and ver- line and a cerclage wire shaped anteriorly at patella as an eight. The tical fractures 12-17% [2, 3] and these are rarely displaced [5]. -

Is There Any Difference Between the Biomechanical Strengths of The
550 Acta Orthop. Belg.O. KOCADAL, 2017, ,83 M,. 550-557PEPE, Z. GUNES, E. AKSAHIN, S. DURAN, C. N. AKTEKIN ORIGINAL STUDY Is there any difference between the biomechanical strengths of the current fixation techniques for comminuted distal patellar fractures? (Comparison of distal patella fracture fixation techniques) Onur KOCADAL, Murad PEPE, Zafer GUNES, Ertugrul AKSAHIN, Semra DURAN, Cem Nuri AKTEKIN From the Ankara Training and Research Hospital, Ulucanlar, Ankara, Turkey In this biomechanical study, the strength of five surgical treatment for the patella inferior pole different fixation techniques -anterior tension band fractures (15). Internal fixation of the distal part, if wiring with K-wires, separate vertical wiring, headless possible, or excision of the small bone fragments compression screws with anterior tension band with repair of the patellar tendon by transosseous wiring, cannulated screws with tension band wiring pull-out sutures, in the extremely comminuted and memory shape patellar fixator- for distal patellar cases, should be performed (17). However in the fractures were compared. Forty calf knees were used for the biomechanical testing. Each specimen latter, non-absorbable synthetic sutures and partial was pre-loaded with 10 N at 1 N/s. The distraction patellectomy necessitate immobilization of the forces were applied consistently with the velocity of 5 knee, which causes weakness in the quadriceps mm/s. The ultimate load (N) and displacement (mm) muscle (7,14,17,30). Therefore, fixation of the distal values were recorded. The headless compression patellar fractures has gained popularity over partial screw with anterior tension band wiring (656.9±167.9 patellectomy. N) and the cannulated screws with anterior tension There are various previously defined surgical band wiring (642.6±166.0 N) obtained significantly fixation options for patella inferior pole fractures: higher ultimate loading values compared to the other anterior tension band wiring, combining screw fixation methods (p<0.05). -

Pseudogout at the Knee Joint Will Frequently Occur After Hip Fracture
Harato and Yoshida Journal of Orthopaedic Surgery and Research (2015) 10:4 DOI 10.1186/s13018-014-0145-9 RESEARCH ARTICLE Open Access Pseudogout at the knee joint will frequently occur after hip fracture and lead to the knee pain in the early postoperative period Kengo Harato1,3*† and Hiroki Yoshida2† Abstract Background: Symptomatic knee joint effusion is frequently observed after hip fracture, which may lead to postoperative knee pain during rehabilitation after hip fracture surgery. However, unfortunately, very little has been reported on this phenomenon in the literature. The purpose of the current study was to investigate the relationship between symptomatic knee effusion and postoperative knee pain and to clarify the reason of the effusion accompanied by hip fracture. Methods: A total of 100 patients over 65 years of age with an acute hip fracture after fall were prospectively followed up. Knee effusion was assessed on admission and at the operating room before the surgery. If knee effusion was observed at thetimeofthesurgery,synovialfluidwascollectedintosyringes to investigate the cause of the effusion using a compensated polarized light microscope. Furthermore, for each patient, we evaluated age, sex, radiographic knee osteoarthritis (OA), type of the fracture, laterality, severity of the fracture, and postoperative knee pain during rehabilitation. These factors were compared between patients with and without knee effusion at the time of the surgery. As a statistical analysis, we used Mann–Whitney U-test for patients’ age and categorical variables were analyzed by chi-square test or Fisher’sexacttest. Results: A total of 30 patients presented symptomatic knee effusion at the time of the surgery. -

Treatment of Common Hip Fractures: Evidence Report/Technology
This report is based on research conducted by the Minnesota Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290 2007 10064 1). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This report may be used, in whole or in part, as the basis for the development of clinical practice guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage policies. AHRQ or U.S. Department of Health and Human Services endorsement of such derivative products may not be stated or implied. Evidence Report/Technology Assessment Number 184 Treatment of Common Hip Fractures Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290 2007 10064 1 Prepared by: Minnesota Evidence-based Practice Center, Minneapolis, Minnesota Investigators Mary Butler, Ph.D., M.B.A. Mary Forte, D.C. Robert L. Kane, M.D. Siddharth Joglekar, M.D. Susan J. Duval, Ph.D. Marc Swiontkowski, M.D. -
Management of Knee Injuries Protocol in Mius and Wics
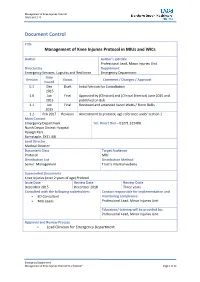
Management of Knee Injuries Protocol FINAL 04.12.15 Document Control Title Management of Knee Injuries Protocol in MIUs and WICs Author Author’s job title Professional Lead, Minor Injuries Unit Directorate Department Emergency Services, Logistics and Resilience Emergency Department Date Version Status Comment / Changes / Approval Issued 0.1 Dec Draft Initial Version for Consultation 2015 1.0 Jun Final Approved by (Clinician) and (Clinical Director) June 2015 and 2015 published on Bob. 1.1 Jun Final Reviewed and amended Karen Watts / Fionn Bellis 2015 1.2 Feb 2017 Revision Amendment to protocol, age reference under section 1 Main Contact Emergency Department Tel: Direct Dial – 01271 322480 North Devon District Hospital Raleigh Park Barnstaple, EX31 4JB Lead Director Medical Director Document Class Target Audience Protocol MIU Distribution List Distribution Method Senior Management Trust’s internal website Superseded Documents Knee Injuries (over 2 years of age) Protocol Issue Date Review Date Review Cycle December 2015 December 2018 Three years Consulted with the following stakeholders Contact responsible for implementation and ED Consultant monitoring compliance: MIU Leads Professional Lead, Minor Injuries Unit Education/ training will be provided by: Professional Lead, Minor Injuries Unit Approval and Review Process Lead Clinician for Emergency Department Emergency Department Management of Knee Injuries Protocol V1.2 Feb2017 Page 1 of 12 Management of Knee Injuries Protocol FINAL 04.12.15 Local Archive Reference G:\Policies and Protocols Local Path MIU Filename Knee Injuries (over 2 years of age) Protocol V1.2 Policy categories for Trust’s internal website Tags for Trust’s internal website (Bob) (Bob) MIU MIU Emergency Department Management of Knee Injuries Protocol V1.2 Feb2017 Page 2 of 12 Management of Knee Injuries Protocol FINAL 04.12.15 2. -

Suture Repair of Patellar Inferior Pole Fracture: Transosseous Tunnel Suture Compared with Anchor Suture
EXPERIMENTAL AND THERAPEUTIC MEDICINE 22: 998, 2021 Suture repair of patellar inferior pole fracture: Transosseous tunnel suture compared with anchor suture WENZHOU HUANG1‑3, TIANLONG WU1‑3, QIANGQIANG WEI1‑3, LONGHAI PENG1‑3, XIGAO CHENG1‑3 and GUICHENG GAO1‑3 1Department of Orthopaedic Surgery, The Second Affiliated Hospital of Nanchang University; 2Institute of Orthopedics of Jiangxi Province; 3Institute of Minimally Invasive Orthopedics of Nanchang University, Nanchang, Jiangxi 330006, P.R. China Received May 18, 2020; Accepted March 10, 2021 DOI: 10.3892/etm.2021.10430 Abstract. Patellar inferior pole fracture is difficult to treat due Introduction to the inherent weakness of small comminuted distal fragments. However, suture fixation was recently introduced and reported. Inferior pole fracture of the patella is an extra‑articular injury The aim of the present study was to evaluate and compare that accounts for 5% of all patellar fractures and usually requires the clinical outcomes of two suture techniques, transosseous operative treatment if displaced or associated with complete tunnel suture (TTS) and anchor suture (AS), for the fixation disruption of the extensor mechanism (1). However, displaced of patellar inferior pole fracture. A total of 35 patients with fracture fragments are typically small and comminuted and it patellar inferior pole fracture treated at the Second Affiliated is difficult to fix and maintain anatomical reduction (2). The Hospital of Nanchang University (Nanchang, China) between inferior patellar pole is continuous with the patellar tendon and June 2014 and April 2018 were retrospectively reviewed. Of the key to reconstructing the fracture fragment surgically is these, 14 were treated with the TTS technique and 21 using AS to reestablish the extensor mechanism while simultaneously fixation. -

Distal Tibial Fracture
Distal Tibial Fracture Sally Choi Date: 7/15/2020 RAD 4014 Dr. Manickam Kumaravel History 7/8/2020 • 20s F • MVC at highway speeds • Only reports R forearm pain, also presents with forehead hematoma, confused, and GCS 11 • Could not get reliable exam so pan-scanned • XR R ankle, elbow, foot, forearm, tibia fibula, and chest • CT chest/ab/pelvis, head/neck, and cervical spine • R Ankle Imaging: XR 7/8/20, CT 7/9/20 McGovern Medical School Differential Diagnosis for Ankle Injury • Fracture • Hemarthrosis • Ligament Injury • Soft Tissue Edema • Complex Regional Pain Syndrome McGovern Medical School XR R Ankle McGovern Medical School XR R Ankle Fibula Fibula Tibia Fibular notch Medial Malleolus Lateral Talus Lateral Malleolus Malleolus Navicular Calcaneus Calcaneus Cuneiforms Cuboid McGovern Medical School XR R Ankle McGovern Medical School XR R Ankle • Comminuted, impacted pilon fracture of distal right tibia • Definition: Pilon fracture is a type of distal tibial fracture involving the tibial plafond. McGovern Medical School XR R Ankle McGovern Medical School XR R Ankle • 3 mm cortical offset at the posterior 3rd of the articular surface of the tibial plafond McGovern Medical School XR R Ankle • Convex soft tissue swelling at the anterior medial aspect of right ankle McGovern Medical School CT R Ankle w/o Contrast (s/p ex fix) – Coronal Anterior → → → Posterior McGovern Medical School CT R Ankle w/o Contrast (s/p ex fix) – Coronal Anterior → → → Posterior McGovern Medical School CT R Ankle w/o Contrast (s/p ex fix) – Sagittal Lateral → → → Medial McGovern Medical School CT R Ankle w/o Contrast (s/p ex fix) – Sagittal Lateral → → → Medial McGovern Medical School Key imaging findings • Comminuted distal tibial fracture with coronally oriented fracture component, extending into the medial malleolus, with focal zone of depression comprising 30% of the tibial plafond with maximal depression of 1 cm. -

Patella Fracture
Patella Fracture A fracture is a broken bone. A patellar fracture is a break in the patella, or kneecap, the small bone that sits at the front of your knee. Because the patella acts as a shield for your knee joint, it is vulnerable to fracture if you fall directly onto your knee or hit it against the dashboard in a vehicle collision. Some patellar fractures can be treated by wearing a cast or splint until the bone heals. In some patellar fractures, however, the pieces of bone move out of place when the injury occurs. For these more complicated fractures, surgery is needed to restore and stabilize the kneecap and allow for the return of function. Depending upon your specific fracture, you may be allowed to bear weight on your leg while wearing a cast or brace. With some fractures, however, weight bearing is not allowed for 6 to 8 weeks. Your Consultant will talk with you about restrictions on weight bearing. Physiotherapy Exercises- Stage 1 These exercises can be carried out to maintain lower limb strength even if you are non-weight bearing or wearing a brace. Use ice and elevate your leg to control swelling. Ensure you have adequate pain relief. 1. Quads set QUAD SET - TOWEL UNDER KNEE Tighten your top thigh muscle as you attempt to press the back of your knee downward towards the table. 2. Short arc Place two rolled towels under the quads knee to lift it about 5 inches off the mat. Bring your toes towards your head (dorsiflexion) then straighten the knee for a hold of 3-5 seconds. -

Tennessee X-Ray Jul-Dec 2021
Volume 27 Issue 3 Tennessee X-Ray Jul-Dec 2021 Radiology Events to Remember • October—National Breast Cancer Awareness Month Visit http:// www.nationalbreastcancer.org/breast-cancer-awareness-month • TSRT Annual Meeting: Fall 2021 Visit http://www.tsrt.org/ • National Mammography Day: October 15, 2021 • World Osteoporosis Day: October 20, 2021 • Remembering Wilhelm Conrad Roentgen 126th Anniversary of the discovery of x-rays November 8, 1895 • National Radiologic Technology Week: November 7-13, 2021 Theme: Essential Together https://www.asrt.org/events-and- conferences/nrtw • Radiological Society of North America: November 28–December 2, 2021 RSNA Scientific Assembly and Annual meeting to be held in Chicago Visit www.rsna.org Limited Scope Exam Fee Increase Limited Scope Testing (LST) provides application processing services for eligible students wishing to sit for the American Registry of Radiologic Technologists (ARRT) Limited Scope of Practice in Radiology examination and the Bone Densitometry Equipment Operator examination for the state of Tennessee. The cost of both these exams will increase to $275 on January 1, 2022 due to an ARRT exam fee increase. Renewing in 2022? If you renew your license next year in 2022, you need to complete your 20 CE credits by December 31, 2021 to be compliant with current state rules. Even though you must complete your CE credits within the 2 preceding calendar years, the due date for proof of that completion is not until your biennium renewal due date. INSIDE THIS ISSUE Puzzle Challenge 3 X-Ray Quiz 3 Amazing Facts 3 Online Access Instructions 4 Answer Sheet Instructions 4 Direct Reading DR-105 Article 5 DR-105 DR-105 Post-Test 32 Extremity Fractures Link to XRN Order Form 35 Link to RES Enrollment 35 Link to CE Enrollment 35 Change of Address Form 36 Important Facts to Remember About Your TN Medical X-Ray License 1. -

Medical Consultation for the Elderly Patient with Hip Fracture
J Am Board Fam Pract: first published as 10.3122/15572625-11-5-366 on 1 September 1998. Downloaded from CLINICAL REVIEW Medical Consultation for the Elderly Patient With Hip Fracture RichardJ Ackermann, MD Background: This article describes a family physician geriatrician's perspective on the comprehensive management of hip fracture in frail elderly patients. Primary care physicians might be called upon to pro vide medical consultation for these patients. Methods: Guidelines were developed by a combination of personal experience in consulting for several hun dred elderly patients with hip fracture at a large community hospital, literature review using the key words "hip fractures," "aged," and "aged, 80 and over," and educational presentations for family practice residents. Results and Conclusions: Elderly patients with hip fracture offer a prime opportunity for comprehensive geriatric assessment. Intertrochanteric fractures are almost always treated with internal fixation, whereas femoral neck fractures can be treated by either fixation or by hemiarthroplasty. Hip fracture should be re garded as a surgical urgency, and generally operation should not be delayed, even if patients have serious comorbidity. The family physician can be instrumental in preparing the patient for surgery, preventing and treating complications, and assisting in the placement and rehabilitation of patients after hospital dis charge. 0 Am Board Fam Pract 1998; 11:366-77.) As the result of an aging population, family physi Some hip fractures and the falls that precede cians are increasingly likely to participate in the them are probably preventable. Strategies to de care of elderly patients suffering hip fracture. This tect and treat osteoporosis, especially in high-risk copyright. -

What You Should Know About Hip Fractures
Information O from Your Family Doctor What You Should Know About Hip Fractures What is a hip fracture? surgery. It may involve putting pins, rods, and A hip fracture is a break in the top of your plates into the hip joint. Some hip fractures are upper leg bone near the hip joint, just below treated with a hip replacement. The orthopedic the waist. The type of hip fracture depends surgeon will help decide which surgery is best on which part of the bone breaks. Most hip for you. fractures are caused by a fall in people 65 years or older. People with weak bones, known as What happens next? osteoporosis (OSS-tee-oh-puh-RO-sis), are You will need to work with a physical therapist more likely to break a hip. at home, in the therapist’s office, or in a skilled nursing facility to regain use of your hip. You will What are the symptoms? practice bending, walking, and climbing stairs. The most common symptom is pain in the hip For most patients, your doctor will or groin area. The pain is usually worse when recommend a medicine called a bisphosphonate you try to move the hip. There is a lot of pain (bis-FOSS-fuh-nate). This is taken by mouth. when you walk. Most people cannot walk with It can help lower your chance of another hip a hip fracture. fracture. How is it found? How can hip fractures be prevented? An x-ray can show if the hip is broken and You can prevent falls by talking to your doctor which part of the bone is fractured.