Vertical Open Patella Fracture, Treatment, Rehabilitation and the Moment to Fixation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Surgical Repair of Transverse Patella Fractures
A vertical patella fracture James Heilman, MD The Surgical Repair of Transverse Patella Fractures Angela Miller, cst Patella fractures constitute about 1% of all fractures, and are mostly caused by direct trauma to the front of the knee.1 There are many types of patella fractures: comminuted, open, nondisplaced and displaced. This article will focus on the about 50% to 80% of patellar fractures that are transverse,3 and requires the surgical treatment using Kirschner wires, also known as K-wires and tension-band wiring. ANATOMY AND PHYSIOLOGY LEARNING OBJECTIVES The patella is the largest sesamoid bone in the human body. Sesamoid ▲ Learn about the use of K-wires for bones are not connected to other bones; instead, they are connected treatment of this fracture by tendons or are embedded in muscle tissue. The patella bone can ▲ Review the anatomy related to this be found in the quadriceps tendons. The function of sesamoid bones is to provide a smooth surface over which the tendon can slide, and procedure increases the ability of the tendons to transmit muscle forces.2 The ▲ Recall the patient preparation patella bone is located anterior to the knee joint, and the posterior sur- specific to this operation face articulates with the femur. It is attached proximally to the femoral ▲ Examine the role of the surgical condyles, and attached distally to the condyles of the tibia and upper technologist during a transverse ends of the fibula.5 patella fracture ▲ Read about studies comparing the POSITIONING use of metallic versus nonmetallic During transverse patella fractures a patient will be placed in the implants supine position, with their arms are placed at each of their sides and A vertical patella fracture James Heilman, MD AUGUST 2016 | The Surgical Technologist | 349 tucked by the draw sheet. -

Is There Any Difference Between the Biomechanical Strengths of The
550 Acta Orthop. Belg.O. KOCADAL, 2017, ,83 M,. 550-557PEPE, Z. GUNES, E. AKSAHIN, S. DURAN, C. N. AKTEKIN ORIGINAL STUDY Is there any difference between the biomechanical strengths of the current fixation techniques for comminuted distal patellar fractures? (Comparison of distal patella fracture fixation techniques) Onur KOCADAL, Murad PEPE, Zafer GUNES, Ertugrul AKSAHIN, Semra DURAN, Cem Nuri AKTEKIN From the Ankara Training and Research Hospital, Ulucanlar, Ankara, Turkey In this biomechanical study, the strength of five surgical treatment for the patella inferior pole different fixation techniques -anterior tension band fractures (15). Internal fixation of the distal part, if wiring with K-wires, separate vertical wiring, headless possible, or excision of the small bone fragments compression screws with anterior tension band with repair of the patellar tendon by transosseous wiring, cannulated screws with tension band wiring pull-out sutures, in the extremely comminuted and memory shape patellar fixator- for distal patellar cases, should be performed (17). However in the fractures were compared. Forty calf knees were used for the biomechanical testing. Each specimen latter, non-absorbable synthetic sutures and partial was pre-loaded with 10 N at 1 N/s. The distraction patellectomy necessitate immobilization of the forces were applied consistently with the velocity of 5 knee, which causes weakness in the quadriceps mm/s. The ultimate load (N) and displacement (mm) muscle (7,14,17,30). Therefore, fixation of the distal values were recorded. The headless compression patellar fractures has gained popularity over partial screw with anterior tension band wiring (656.9±167.9 patellectomy. N) and the cannulated screws with anterior tension There are various previously defined surgical band wiring (642.6±166.0 N) obtained significantly fixation options for patella inferior pole fractures: higher ultimate loading values compared to the other anterior tension band wiring, combining screw fixation methods (p<0.05). -
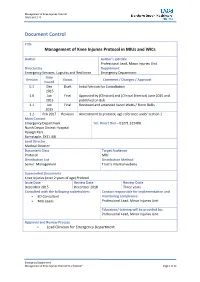
Management of Knee Injuries Protocol in Mius and Wics
Management of Knee Injuries Protocol FINAL 04.12.15 Document Control Title Management of Knee Injuries Protocol in MIUs and WICs Author Author’s job title Professional Lead, Minor Injuries Unit Directorate Department Emergency Services, Logistics and Resilience Emergency Department Date Version Status Comment / Changes / Approval Issued 0.1 Dec Draft Initial Version for Consultation 2015 1.0 Jun Final Approved by (Clinician) and (Clinical Director) June 2015 and 2015 published on Bob. 1.1 Jun Final Reviewed and amended Karen Watts / Fionn Bellis 2015 1.2 Feb 2017 Revision Amendment to protocol, age reference under section 1 Main Contact Emergency Department Tel: Direct Dial – 01271 322480 North Devon District Hospital Raleigh Park Barnstaple, EX31 4JB Lead Director Medical Director Document Class Target Audience Protocol MIU Distribution List Distribution Method Senior Management Trust’s internal website Superseded Documents Knee Injuries (over 2 years of age) Protocol Issue Date Review Date Review Cycle December 2015 December 2018 Three years Consulted with the following stakeholders Contact responsible for implementation and ED Consultant monitoring compliance: MIU Leads Professional Lead, Minor Injuries Unit Education/ training will be provided by: Professional Lead, Minor Injuries Unit Approval and Review Process Lead Clinician for Emergency Department Emergency Department Management of Knee Injuries Protocol V1.2 Feb2017 Page 1 of 12 Management of Knee Injuries Protocol FINAL 04.12.15 Local Archive Reference G:\Policies and Protocols Local Path MIU Filename Knee Injuries (over 2 years of age) Protocol V1.2 Policy categories for Trust’s internal website Tags for Trust’s internal website (Bob) (Bob) MIU MIU Emergency Department Management of Knee Injuries Protocol V1.2 Feb2017 Page 2 of 12 Management of Knee Injuries Protocol FINAL 04.12.15 2. -

Fracture Lower Extremity Part II
CONTENTS FEMUR SHAFT BOTH BONE SUBTROCHANTERIC TIBIAL PLAFON FRACTURE LOWER FRACTURE ANKLE EXTREMITIES: PART 2 FRACTURE FEMUR FOOT SUPRACONDYLAR FRACTURE FEMUR CALCANEUS PATELLA TALUS WORAWAT LIMTHONGKUL, M.D. 14 JAN 2013 TIBIA LISFRANC’S TIBIAL PLATEAU METATARSAL 1 2 SUBTROCHANTERIC FRACTURE FEMUR A PART OF FRACTURE OCCUR BETWEEN TIP OF LESSER TROCHANTER AND A POINT 5 SUBTROCHANTERIC CM DISTALLY CALCAR FEMORALE FRACTURE LARGE FORCES ARE NEEDED TO CAUSE FRACTURES IN 5 CM YOUNG & ADULT INJURY IS RELATIVELY TRIVIAL IN ELDERLY 2° CAUSE: OSTEOPOROSIS, OSTEOMALACIA, PAGET’S 3 4 SUBTROCHANTERIC FRACTURE FEMUR TREATMENT INITIAL FEMUR SHAFT TRACTION DEFINITE FRACTURE ORIF WITH INTRAMEDULLARY NAIL OR 95 DEGREE HIP- SCREW-PLATE 5 6 FEMUR FRACTURE FILM HIPS SEVERE PAIN, UNABLE TO BEAR WEIGHT 10% ASSOCIATE FEMORAL SUPRACONDYLAR NECK FRACTURE FEMUR FRACTURE TREATMENT: ORIF WITH IM NAIL OR P&S COMPLICATION: HEMORRHAGE, NEUROVASCULAR INJURY, FAT EMBOLI 7 8 SUPRACONDYLAR FEMUR FRACTURE SUPRACONDYLAR ZONE DIRECT VIOLENCE IS THE USUAL CAUSE PATELLA FRACTURE LOOK FOR INTRA- ARTICULAR INVOLVEMENT CHECK TIBIAL PULSE TREATMENT: ORIF WITH P&S 9 10 PATELLA FRACTURE PATELLA FRACTURE FUNCTION: LENGTHENING THE ANTERIOR LEVER ARM DDX: BIPATITE PATELLA AND INCREASING THE (SUPEROLATERAL) EFFICIENCY OF THE QUADRICEPS. TREATMENT: DIRECT VS INDIRECT NON-DISPLACE, INJURY INTACT EXTENSOR : CYLINDRICAL CAST TEST EXTENSOR MECHANISM DISPLACE, DISRUPT EXTENSOR: ORIF WITH VERTICAL FRACTURE: TBW MERCHANT VIEW 11 12 PATELLAR DISLOCATION ADOLESCENT FEMALE DISLOCATION AROUND USUALLY -

Suture Repair of Patellar Inferior Pole Fracture: Transosseous Tunnel Suture Compared with Anchor Suture
EXPERIMENTAL AND THERAPEUTIC MEDICINE 22: 998, 2021 Suture repair of patellar inferior pole fracture: Transosseous tunnel suture compared with anchor suture WENZHOU HUANG1‑3, TIANLONG WU1‑3, QIANGQIANG WEI1‑3, LONGHAI PENG1‑3, XIGAO CHENG1‑3 and GUICHENG GAO1‑3 1Department of Orthopaedic Surgery, The Second Affiliated Hospital of Nanchang University; 2Institute of Orthopedics of Jiangxi Province; 3Institute of Minimally Invasive Orthopedics of Nanchang University, Nanchang, Jiangxi 330006, P.R. China Received May 18, 2020; Accepted March 10, 2021 DOI: 10.3892/etm.2021.10430 Abstract. Patellar inferior pole fracture is difficult to treat due Introduction to the inherent weakness of small comminuted distal fragments. However, suture fixation was recently introduced and reported. Inferior pole fracture of the patella is an extra‑articular injury The aim of the present study was to evaluate and compare that accounts for 5% of all patellar fractures and usually requires the clinical outcomes of two suture techniques, transosseous operative treatment if displaced or associated with complete tunnel suture (TTS) and anchor suture (AS), for the fixation disruption of the extensor mechanism (1). However, displaced of patellar inferior pole fracture. A total of 35 patients with fracture fragments are typically small and comminuted and it patellar inferior pole fracture treated at the Second Affiliated is difficult to fix and maintain anatomical reduction (2). The Hospital of Nanchang University (Nanchang, China) between inferior patellar pole is continuous with the patellar tendon and June 2014 and April 2018 were retrospectively reviewed. Of the key to reconstructing the fracture fragment surgically is these, 14 were treated with the TTS technique and 21 using AS to reestablish the extensor mechanism while simultaneously fixation. -

Patella Fracture
Patella Fracture A fracture is a broken bone. A patellar fracture is a break in the patella, or kneecap, the small bone that sits at the front of your knee. Because the patella acts as a shield for your knee joint, it is vulnerable to fracture if you fall directly onto your knee or hit it against the dashboard in a vehicle collision. Some patellar fractures can be treated by wearing a cast or splint until the bone heals. In some patellar fractures, however, the pieces of bone move out of place when the injury occurs. For these more complicated fractures, surgery is needed to restore and stabilize the kneecap and allow for the return of function. Depending upon your specific fracture, you may be allowed to bear weight on your leg while wearing a cast or brace. With some fractures, however, weight bearing is not allowed for 6 to 8 weeks. Your Consultant will talk with you about restrictions on weight bearing. Physiotherapy Exercises- Stage 1 These exercises can be carried out to maintain lower limb strength even if you are non-weight bearing or wearing a brace. Use ice and elevate your leg to control swelling. Ensure you have adequate pain relief. 1. Quads set QUAD SET - TOWEL UNDER KNEE Tighten your top thigh muscle as you attempt to press the back of your knee downward towards the table. 2. Short arc Place two rolled towels under the quads knee to lift it about 5 inches off the mat. Bring your toes towards your head (dorsiflexion) then straighten the knee for a hold of 3-5 seconds. -

Tennessee X-Ray Jul-Dec 2021
Volume 27 Issue 3 Tennessee X-Ray Jul-Dec 2021 Radiology Events to Remember • October—National Breast Cancer Awareness Month Visit http:// www.nationalbreastcancer.org/breast-cancer-awareness-month • TSRT Annual Meeting: Fall 2021 Visit http://www.tsrt.org/ • National Mammography Day: October 15, 2021 • World Osteoporosis Day: October 20, 2021 • Remembering Wilhelm Conrad Roentgen 126th Anniversary of the discovery of x-rays November 8, 1895 • National Radiologic Technology Week: November 7-13, 2021 Theme: Essential Together https://www.asrt.org/events-and- conferences/nrtw • Radiological Society of North America: November 28–December 2, 2021 RSNA Scientific Assembly and Annual meeting to be held in Chicago Visit www.rsna.org Limited Scope Exam Fee Increase Limited Scope Testing (LST) provides application processing services for eligible students wishing to sit for the American Registry of Radiologic Technologists (ARRT) Limited Scope of Practice in Radiology examination and the Bone Densitometry Equipment Operator examination for the state of Tennessee. The cost of both these exams will increase to $275 on January 1, 2022 due to an ARRT exam fee increase. Renewing in 2022? If you renew your license next year in 2022, you need to complete your 20 CE credits by December 31, 2021 to be compliant with current state rules. Even though you must complete your CE credits within the 2 preceding calendar years, the due date for proof of that completion is not until your biennium renewal due date. INSIDE THIS ISSUE Puzzle Challenge 3 X-Ray Quiz 3 Amazing Facts 3 Online Access Instructions 4 Answer Sheet Instructions 4 Direct Reading DR-105 Article 5 DR-105 DR-105 Post-Test 32 Extremity Fractures Link to XRN Order Form 35 Link to RES Enrollment 35 Link to CE Enrollment 35 Change of Address Form 36 Important Facts to Remember About Your TN Medical X-Ray License 1. -

Postoperative Instructions Following Open Repair of Patella Fracture-- Dr
Postoperative Instructions Following Open Repair of Patella Fracture-- Dr. Kerns You are going home after surgical repair of your broken knee-cap. This does not mean that you are on your own. Please read the instructions below carefully and if you have any other questions or concerns, there is always someone available to talk you through your troubles. If it is between the hours of 8AM and 4PM, please call Covenant Medical Group Orthopedic Surgery mainnumber (989) 583-7450. After office hours, you can reach the orthopedic surgeon on-call through our answering service at (989) 583-7450. Protecting Your Repair • Wear your knee immobilizer. Do not take it off…ever. • You may walk on the injured leg only so long as you are wearing your knee immobilizer. • Keep your dressing clean and dry. Stay in cool, temperature controlled spaces to avoid excessive sweating and moisture around your incision. This will also help to prevent itching skin within your splint. Sponge bathing is the safest technique for personal hygiene, but a trash bag that has been secured over the splint or cast with Saran-wrap and tape can allow careful use of a shower. Be sure to meticulously dry the bag before attempting to remove it. Water may collect in pockets and creases, then drain down the top of your splint before you have a chance to prevent it, otherwise. Minimize Pain and Swelling Even though your incisions are quite small, you have had a significant surgical procedure at your knee. It is normal to have pain throughout your wrist and forearm but rest assured that this will pass. -

Patellar (Kneecap) Fractures-Orthoinfo
Patellar (Kneecap) Fractures Because your kneecap (patella) acts like a shield for your knee joint, it can easily be broken. Falling directly onto your knee, for example, is a common cause of patellar fractures. These fractures are serious injuries and often require surgery to heal. Over the long term, they may cause arthritis in the knee. Anatomy The patella is a small bone located in front of your knee joint — where the thighbone (femur) and shinbone (tibia) meet. It protects your knee and connects the muscles in the front of your thigh to your tibia. The ends of the femur and the undersides of the patella are covered with a slippery substance called articular cartilage. This helps the bones glide smoothly along each other as you move your leg. Statistics Patellar fractures account for about 1% of all fractures. They are most common in people who are 20 to 50 years old. Men are twice as likely as women to fracture the kneecap. Types of Patellar Fractures Patellar fractures vary. The kneecap can crack just slightly, or can be broken into many pieces. A break in the kneecap can happen at the top, center, or lower part of the bone. Sometimes, fractures occur in more than one area of the kneecap. This x-ray of the knee taken from the side shows a patella that has been fractured in three places. Stable fracture. This type of fracture is nondisplaced. The broken ends of the bones meet up correctly and are aligned. In a stable fracture, the bones usually stay in place during healing. -

2019 Trauma Practice Profiled ABOS Blueprint
2019 Trauma Practice Profiled ABOS Blueprint ABOS BLUEPRINT ABOS% Max % Questions TOPICS COVERED ON ORTHOBULLETS Pelvis/Acetabulum 8-12% IN STUDY PLAN Pelvis (initial) 1-3% 3% 45 Pelvic Ring Fractures Pelvis (definitive) 1-3% 3% 45 Pelvis Fractures - Pediatric Acetabulum 1-4% 4% 6 Stoppa Approach to Acetabulum Sacral FX SI Dislocation & Crescent FX Posterior Approach to the Acetabulum (Kocher-Langenbeck) Acetabular FX Ilium FX Ilioinguinal Approach to the Acetabulum Upper Extremity 18-22% Shoulder-scapula 0.5-1% 1% 1.5 Scapula FX Shoulder-clavicle 1-2% 2% 30 Flail Chest Shoulder-proximal humerus 1-4% 4% 6 Sternoclavicular Dislocation Humerus shaft 1-2% 2% 30 Brachial Plexus Injuries Elbow-distal humerus 1-3% 3% 45 Clavicle Shaft FX Elbow-proximal/radius/ulna/dislocations 1-3% 3% 45 Distal Third Clavicle FX Elbow-pediatric supracondylar humerus 0.5-1% 1% 1.5 Proximal Humerus FX Forearm-radius/ulna 0.5-1% 1% 1.5 Proximal Humerus Fracture Malunion Distal radius 1-3% 3% 45 Humeral Shaft FX Humeral Shaft Nonunion Distal Humerus FX Capitellum FX Coronoid FX Olecranon FX Monteggia FX Monteggia Fracture - Pediatric Radial Head FX Radial Head and Neck FX - Pediatric Elbow Dislocation Terrible Triad Injury of Elbow Supracondylar Fracture - Pediatric Medial Epicondylar FX - Pediatric Lateral Condyle Fracture - Pediatric Radius and Ulnar Shaft FX Radioulnar Synostosis Both Bone Forearm Fracture - Pediatric Distal Radius FX Distal Radius FX - Pediatric Distal Radial Ulnar Joint (DRUJ) Injuries Galeazzi FX Galeazzi Fracture - Pediatric Lower Extremity -

Transverse Patella Fracture in a Ten Year Old Boy: Case Report
Case Report East African Orthopaedic Journal TRANSVERSE PATELLA FRACTURE IN A TEN YEAR OLD BOY: CASE REPORT B.M. Ndeleva, MMed Ortho (Mak), FCS (Ortho) ECSA, Orthopaedic Surgeon & Lecturer, Egerton University, Njoro, Kenya. C.K. Lakati, FCS (Ortho) ECSA, Orthopaedic Surgeon & Lecturer, Egerton University, Njoro, Kenya, M.L. Lutomia, FCS (Ortho), ECSA, Orthopaedic Surgeon & Lecturer, Egerton University, Njoro, Kenya and S.O. Mak’Anyengo , MBChB (Pret), COSECSA, Resident, Rift Valley Provincial General Hospital, Nakuru, Kenya Correspondence to: Dr. B. M. Ndeleva, P.O. Box 1562 - 90100, Machakos, Kenya. Email: [email protected] ABSTRACT Patella fractures are rare in children. Transverse fractures in particular are an uncommon pattern. We report a case of a transverse patella fracture in a ten year old boy. He presented with inability to actively extend his left knee, two months after a fall. On evaluation he was found to have a transverse fracture of his left patella. This was treated by tension band wiring. INTRODUCTION Figure 1 AP and lateral view radiographs of the patient’s left The function of the patella is to increase the mechanical knee advantage of the quadriceps by increasing the angle at which the quadriceps acts. In children a larger part of the patella is cartilaginous compared to adults. It is also a lot more mobile and therefore less predisposed to fracturing (1,2). As more and more of the patella ossifies, the incidence of fractures of the patella increases. The pattern too changes. While the sleeve fracture is the commonest pattern seen in young children, adolescents will have other patterns including transverse and comminuted fractures just as in the adults (1, 2). -

Discharge Instructions for Patella Fracture Fixation
Discharge Instructions for Patella Fracture Fixation Wound Care: • Your post-operative dressing has three layers. Your incisions were closed with staples. These will be removed 10-14 days after surgery • The second layer is gauze pads to help absorb some water that will leak from your knee for the first couple hours after surgery. Occasionally, there will also be a small amount of blood mixed with this water - this is normal. • The outer layer is a long ace wrap that was wrapped around your leg from the foot up to your thigh. We wrap the whole leg, not just the knee, so that the ace wrap does not act like a tourniquet causing the lower leg to swell. • Keep dressing on for 3-5 days. After removing the dressing, keep wounds covered with clean dry gauze. • Keep dry for 2 weeks, sponge baths only • Do not submerge in water until incisions are fully healed, this may take up to 4 weeks. Activity: • A brace is used to protect your knee after surgery. The only time you can remove the brace is for physical therapy and hygiene for the first 4-6 weeks following surgery. • The brace's hinges are locked in full extension - do not change the hinges on the brace. • You may put your weight bearing as tolerated/full weight on the operative knee. Remember that the brace must be on and locked in extension at all times while walking. You will probably need to continue use of the crutches up to six weeks after surgery. • Crutch Adjustment: The crutch length will be set at your height so that there are about two to three fingers between the top of the crutch and the armpit.