Managment of Fractures of Patella Olecranon, Malleoli by Tension Band Wiring Method” Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Surgical Repair of Transverse Patella Fractures
A vertical patella fracture James Heilman, MD The Surgical Repair of Transverse Patella Fractures Angela Miller, cst Patella fractures constitute about 1% of all fractures, and are mostly caused by direct trauma to the front of the knee.1 There are many types of patella fractures: comminuted, open, nondisplaced and displaced. This article will focus on the about 50% to 80% of patellar fractures that are transverse,3 and requires the surgical treatment using Kirschner wires, also known as K-wires and tension-band wiring. ANATOMY AND PHYSIOLOGY LEARNING OBJECTIVES The patella is the largest sesamoid bone in the human body. Sesamoid ▲ Learn about the use of K-wires for bones are not connected to other bones; instead, they are connected treatment of this fracture by tendons or are embedded in muscle tissue. The patella bone can ▲ Review the anatomy related to this be found in the quadriceps tendons. The function of sesamoid bones is to provide a smooth surface over which the tendon can slide, and procedure increases the ability of the tendons to transmit muscle forces.2 The ▲ Recall the patient preparation patella bone is located anterior to the knee joint, and the posterior sur- specific to this operation face articulates with the femur. It is attached proximally to the femoral ▲ Examine the role of the surgical condyles, and attached distally to the condyles of the tibia and upper technologist during a transverse ends of the fibula.5 patella fracture ▲ Read about studies comparing the POSITIONING use of metallic versus nonmetallic During transverse patella fractures a patient will be placed in the implants supine position, with their arms are placed at each of their sides and A vertical patella fracture James Heilman, MD AUGUST 2016 | The Surgical Technologist | 349 tucked by the draw sheet. -

Ideal Medial Malleolar Screw Length Based on the Tibial Epiphyseal Scar Location in Weight Bearing CT’S Collin G
Ideal Medial Malleolar Screw Length Based on the Tibial Epiphyseal Scar Location in Weight Bearing CT’s Collin G. Messerly DPM, Keegan A. Duelfer DPM, Troy J. Boffeli DPM, FACFAS, Tyler K. Sorensen, DPM Regions Hospital / HealthPartners Institute for Education and Research - Saint Paul, MN Figure 1. Zone of Dense Bone in Medial Malleolar ORIF Figure 4. Measuring Distal – Most 5% to Medial Malleolus Table 2. Distance Between Epiphyseal Scar & Distal – Most 5% of RESULTS STATEMENT OF PURPOSE The epiphyseal scar is located in the distal The medial malleolus to distal – most 5% mark Tibia 97 WB ankle CT scans evaluated in uninjured ankles Medial malleolar fractures are one of the most common fracture types metaphysis of the tibia, and can oftentimes be was measured on the coronal WB CT slice with Measurement of interest Male: Mean ± SD Female: Mean ± SD (mm) In males < 60 years old there was a 12.75 mm zone of increased bone the widest medial malleolus. Screw threads observed in the ankle joint and have been long fixated with two screws; easily visualized on X-ray and CT scan (red line). (mm) density, as compared to 13.66 mm in those ≥ 60 which was not statistically The distal – most 5% of the tibia (distal to the beyond this point will purchase less dense bone however, the bone density of the distal tibia has potential for poor screw significant. purchase due to compromised bone density. This is especially true in elderly black line) contains dense bone with marked in the medullary canal with potential to not have Epiphyseal Scar to Medial Malleolus 12.75 ± 2.91 9.39 ± 2.38 In females < 60 years old there was 9.39 mm zone of increased bone populations with osteoporotic bone. -

Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT
Patellofemoral Syndrome: Evaluation & Management Scott Sevinsky MSPT What is Patellofemoral Syndrome? Patellofemoral syndrome (PFS) is a term commonly used to describe a condition where the patella ‘tracks’ or glides improperly between the femoral condyles. This improper tracking causes pain in the anterior knee and may lead to degenerative changes or dislocation of the knee cap. To be more precise the term ‘anterior knee pain’ is suggested to encompass all pain-related problems of the anterior part of the knee. By excluding anterior knee pain due to intra-articular pathology, peripatellar tendinitis or bursitis, plica syndromes, Sinding Larsen’s disease, Osgood Schlatter’s disease, neuromas and other rarely occurring pathologies it is suggested that remaining patients with a clinical presentation of anterior knee pain could be diagnosed with PFPS. The term ‘patellofemoral’ is used as no distinction can be made as to which specific structure of the patella or femur is affected. The term ‘chondromalacia patellae’, defined at the beginning of the 20th century to describe pathological changes of the retropatellar cartilage,7,8 was for half a century, used as a synonym for the syndrome of patellofemoral pain. However, several studies during the last 2 decades have shown a poor correlation between articular cartilage damage and the still not well-defined pain mechanism of retropatellar pain. Review of Knee Anatomy 1. Femur – thigh bone; longest bone in the body. · Lateral femoral condyle larger than medial condyle & projects farther anteriorly. · Medial femoral condyle longer anterior to posterior · Distal surfaces are convex · Intercondylar (trochlear) notch: groove in which the patella glides or ‘tracks’ 2. -

Vertical Open Patella Fracture, Treatment, Rehabilitation and the Moment to Fixation
Elmer ress Case Report J Clin Med Res. 2015;7(2):129-133 Vertical Open Patella Fracture, Treatment, Rehabilitation and the Moment to Fixation Joao Alberto Larangeiraa, Liliane Bellenziera, Vanessa da Silva Rigoa, Elias Josue Ramos Netoa, Francisco Fritsch Machry Kruma, Tiango Aguiar Ribeiroa, b, c Abstract Introduction Patella fracture is relatively uncommon and the vertical trace frac- Patella fracture is relatively uncommon and represents approx- ture represents almost 12-17%. The open patella fracture expresses imately 0.5-1.5% of all bone injuries [1, 2], and men are more 6-30%. The association of these two uncommon conditions was the affected than women [3, 4]. The classification can be done by aim of this case report even as the treatment and the moment of fixa- characterizing the fracture pattern in osteochondral, multifrag- tion (definitive surgical treatment). A 27-year-old man after a motor- mented, stellate, transversal, vertical and polar fracture (Fig. cycle accident showed an open patella fracture classified as a Gustilo 1). Other classifications may take into account the presence of and Anderson type IIIA lesion. The patient was immediately treated deviation between the fragments, deviated and not deviated, with precocious surgery fixation with a modified tension band which and the mechanism of injury. The transversal type is more fre- consists of two parallel K-wires positioned orthogonal to the fracture quent corresponding to 50-80%, comminuted 30-35% and ver- line and a cerclage wire shaped anteriorly at patella as an eight. The tical fractures 12-17% [2, 3] and these are rarely displaced [5]. -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -

Patella Problems
Patella Problems Introduction The patella, or kneecap, can be the reason your knee hurts if it fails to function properly. Over time, wear and tear underneath the patella can also lead to degeneration of the cartilage behind the patella and cause pain, weakness and swelling of the knee joint. There are several different problems that affect the patella and the groove that it runs through as the knee is bent. These problems can affect people of all ages. Anatomy The patella, or kneecap, is the moveable bone on the front of the knee. The patella is wrapped inside a large tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. This large tendon when combined with the patella, is called the quadriceps mechanism. The quadriceps mechanism is usually referred to as two separate tendons the quadriceps tendon on top of the patella and the patellar tendon below the patella. The quadriceps mechanism allows you to straighten out the knee. The patella acts like a fulcrum to increase the force of the quadriceps muscle. The underside of the patella is covered with articular cartilage, the smooth covering of joint surfaces. This slippery surface helps the patella glide in a special groove of the thigh bone, or femur. Together the patella and the groove in the femur are called the patellofemoral mechanism. Causes Problems commonly develop when the patella suffers wear and tear. The underlying cartilage begins to degenerate, a condition sometimes referred to as chondromalacia patellae. Wear and tear can develop for several reasons. -

Is There Any Difference Between the Biomechanical Strengths of The
550 Acta Orthop. Belg.O. KOCADAL, 2017, ,83 M,. 550-557PEPE, Z. GUNES, E. AKSAHIN, S. DURAN, C. N. AKTEKIN ORIGINAL STUDY Is there any difference between the biomechanical strengths of the current fixation techniques for comminuted distal patellar fractures? (Comparison of distal patella fracture fixation techniques) Onur KOCADAL, Murad PEPE, Zafer GUNES, Ertugrul AKSAHIN, Semra DURAN, Cem Nuri AKTEKIN From the Ankara Training and Research Hospital, Ulucanlar, Ankara, Turkey In this biomechanical study, the strength of five surgical treatment for the patella inferior pole different fixation techniques -anterior tension band fractures (15). Internal fixation of the distal part, if wiring with K-wires, separate vertical wiring, headless possible, or excision of the small bone fragments compression screws with anterior tension band with repair of the patellar tendon by transosseous wiring, cannulated screws with tension band wiring pull-out sutures, in the extremely comminuted and memory shape patellar fixator- for distal patellar cases, should be performed (17). However in the fractures were compared. Forty calf knees were used for the biomechanical testing. Each specimen latter, non-absorbable synthetic sutures and partial was pre-loaded with 10 N at 1 N/s. The distraction patellectomy necessitate immobilization of the forces were applied consistently with the velocity of 5 knee, which causes weakness in the quadriceps mm/s. The ultimate load (N) and displacement (mm) muscle (7,14,17,30). Therefore, fixation of the distal values were recorded. The headless compression patellar fractures has gained popularity over partial screw with anterior tension band wiring (656.9±167.9 patellectomy. N) and the cannulated screws with anterior tension There are various previously defined surgical band wiring (642.6±166.0 N) obtained significantly fixation options for patella inferior pole fractures: higher ultimate loading values compared to the other anterior tension band wiring, combining screw fixation methods (p<0.05). -

About Your Knee
OrthoInfo Basics About Your Knee What are the parts of the knee? Your knee is Your knee is made up of four main things: bones, cartilage, ligaments, the largest joint and tendons. in your body Bones. Three bones meet to form your knee joint: your thighbone and one of the (femur), shinbone (tibia), and kneecap (patella). Your patella sits in most complex. front of the joint and provides some protection. It is also vital Articular cartilage. The ends of your thighbone and shinbone are covered with articular cartilage. This slippery substance to movement. helps your knee bones glide smoothly across each other as you bend or straighten your leg. Because you use it so Two wedge-shaped pieces of meniscal cartilage act as much, it is vulnerable to Meniscus. “shock absorbers” between your thighbone and shinbone. Different injury. Because it is made from articular cartilage, the meniscus is tough and rubbery to help up of so many parts, cushion and stabilize the joint. When people talk about torn cartilage many different things in the knee, they are usually referring to torn meniscus. can go wrong. Knee pain or injury Femur is one of the most (thighbone) common reasons people Patella (kneecap) see their doctors. Most knee problems can be prevented or treated with simple measures, such as exercise or Articular cartilage training programs. Other problems require surgery Meniscus to correct. Tibia (shinbone) 1 OrthoInfo Basics — About Your Knee What are ligaments and tendons? Ligaments and tendons connect your thighbone Collateral ligaments. These are found on to the bones in your lower leg. -
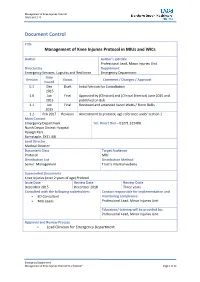
Management of Knee Injuries Protocol in Mius and Wics
Management of Knee Injuries Protocol FINAL 04.12.15 Document Control Title Management of Knee Injuries Protocol in MIUs and WICs Author Author’s job title Professional Lead, Minor Injuries Unit Directorate Department Emergency Services, Logistics and Resilience Emergency Department Date Version Status Comment / Changes / Approval Issued 0.1 Dec Draft Initial Version for Consultation 2015 1.0 Jun Final Approved by (Clinician) and (Clinical Director) June 2015 and 2015 published on Bob. 1.1 Jun Final Reviewed and amended Karen Watts / Fionn Bellis 2015 1.2 Feb 2017 Revision Amendment to protocol, age reference under section 1 Main Contact Emergency Department Tel: Direct Dial – 01271 322480 North Devon District Hospital Raleigh Park Barnstaple, EX31 4JB Lead Director Medical Director Document Class Target Audience Protocol MIU Distribution List Distribution Method Senior Management Trust’s internal website Superseded Documents Knee Injuries (over 2 years of age) Protocol Issue Date Review Date Review Cycle December 2015 December 2018 Three years Consulted with the following stakeholders Contact responsible for implementation and ED Consultant monitoring compliance: MIU Leads Professional Lead, Minor Injuries Unit Education/ training will be provided by: Professional Lead, Minor Injuries Unit Approval and Review Process Lead Clinician for Emergency Department Emergency Department Management of Knee Injuries Protocol V1.2 Feb2017 Page 1 of 12 Management of Knee Injuries Protocol FINAL 04.12.15 Local Archive Reference G:\Policies and Protocols Local Path MIU Filename Knee Injuries (over 2 years of age) Protocol V1.2 Policy categories for Trust’s internal website Tags for Trust’s internal website (Bob) (Bob) MIU MIU Emergency Department Management of Knee Injuries Protocol V1.2 Feb2017 Page 2 of 12 Management of Knee Injuries Protocol FINAL 04.12.15 2. -

Fracture Lower Extremity Part II
CONTENTS FEMUR SHAFT BOTH BONE SUBTROCHANTERIC TIBIAL PLAFON FRACTURE LOWER FRACTURE ANKLE EXTREMITIES: PART 2 FRACTURE FEMUR FOOT SUPRACONDYLAR FRACTURE FEMUR CALCANEUS PATELLA TALUS WORAWAT LIMTHONGKUL, M.D. 14 JAN 2013 TIBIA LISFRANC’S TIBIAL PLATEAU METATARSAL 1 2 SUBTROCHANTERIC FRACTURE FEMUR A PART OF FRACTURE OCCUR BETWEEN TIP OF LESSER TROCHANTER AND A POINT 5 SUBTROCHANTERIC CM DISTALLY CALCAR FEMORALE FRACTURE LARGE FORCES ARE NEEDED TO CAUSE FRACTURES IN 5 CM YOUNG & ADULT INJURY IS RELATIVELY TRIVIAL IN ELDERLY 2° CAUSE: OSTEOPOROSIS, OSTEOMALACIA, PAGET’S 3 4 SUBTROCHANTERIC FRACTURE FEMUR TREATMENT INITIAL FEMUR SHAFT TRACTION DEFINITE FRACTURE ORIF WITH INTRAMEDULLARY NAIL OR 95 DEGREE HIP- SCREW-PLATE 5 6 FEMUR FRACTURE FILM HIPS SEVERE PAIN, UNABLE TO BEAR WEIGHT 10% ASSOCIATE FEMORAL SUPRACONDYLAR NECK FRACTURE FEMUR FRACTURE TREATMENT: ORIF WITH IM NAIL OR P&S COMPLICATION: HEMORRHAGE, NEUROVASCULAR INJURY, FAT EMBOLI 7 8 SUPRACONDYLAR FEMUR FRACTURE SUPRACONDYLAR ZONE DIRECT VIOLENCE IS THE USUAL CAUSE PATELLA FRACTURE LOOK FOR INTRA- ARTICULAR INVOLVEMENT CHECK TIBIAL PULSE TREATMENT: ORIF WITH P&S 9 10 PATELLA FRACTURE PATELLA FRACTURE FUNCTION: LENGTHENING THE ANTERIOR LEVER ARM DDX: BIPATITE PATELLA AND INCREASING THE (SUPEROLATERAL) EFFICIENCY OF THE QUADRICEPS. TREATMENT: DIRECT VS INDIRECT NON-DISPLACE, INJURY INTACT EXTENSOR : CYLINDRICAL CAST TEST EXTENSOR MECHANISM DISPLACE, DISRUPT EXTENSOR: ORIF WITH VERTICAL FRACTURE: TBW MERCHANT VIEW 11 12 PATELLAR DISLOCATION ADOLESCENT FEMALE DISLOCATION AROUND USUALLY -

Physio Med Self Help for Anterior Knee Pain
Physio Med Self Help 0113 229 1300 for Anterior Knee Pain There can be many causes of knee pain. Anterior knee pain or patella-femoral pain is pain that is felt under the knee cap (patella) at the front of the knee. The patella, or kneecap, can be a source of knee pain when it fails to function properly. Alignment or overuse problems of the patella can lead to wear and tear of the cartilage behind the patella. Patella-femoral pain syndrome (anterior knee pain) is a common knee problem that affects the patella and the groove that the patella slides in over the femur (thigh bone). The kneecap together with the lower end of the femur is considered to be the patella-femoral joint. Anatomy of the Area What is the patella, and what does it do? The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. The large quadriceps tendon together with the patella and patellar ligament is called the extensor mechanism. Though we think of it as a single device, the extensor mechanism has two separate tendons, the quadriceps tendon on top of the patella, which connects the quadriceps muscle to the top of the patella, and the patellar tendon below the patella, which connects the lower portion of the patella to the shinbone (tibia). The tendon above the patella is called the suprapatella tendon and the tendon below the patella is called the infrapatella tendon. -

Back of Leg I
Back of Leg I Dr. Garima Sehgal Associate Professor “Only those who risk going too far, can possibly find King George’s Medical University out how far one can go.” UP, Lucknow — T.S. Elliot DISCLAIMER Presentation has been made only for educational purpose Images and data used in the presentation have been taken from various textbooks and other online resources Author of the presentation claims no ownership for this material Learning Objectives By the end of this teaching session on Back of leg – I all the MBBS 1st year students must be able to: • Enumerate the contents of superficial fascia of back of leg • Write a short note on small saphenous vein • Describe cutaneous innervation in the back of leg • Write a short note on sural nerve • Enumerate the boundaries of posterior compartment of leg • Enumerate the fascial compartments in back of leg & their contents • Write a short note on flexor retinaculum of leg- its attachments & structures passing underneath • Describe the origin, insertion nerve supply and actions of superficial muscles of the posterior compartment of leg Introduction- Back of Leg / Calf • Powerful superficial antigravity muscles • (gastrocnemius, soleus) • Muscles are large in size • Inserted into the heel • Raise the heel during walking Superficial fascia of Back of leg • Contains superficial veins- • small saphenous vein with its tributaries • part of course of great saphenous vein • Cutaneous nerves in the back of leg- 1. Saphenous nerve 2. Posterior division of medial cutaneous nerve of thigh 3. Posterior cutaneous