Sleep, Exercise, and Insulin Sensitivity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Petition Signatories 12 November 2020 First Name Surname Country Capacity
Petition Signatories 12 November 2020 First name Surname Country Capacity 1 Ulisses Abade Brasil Vice Presidente Sindicato 2 Sandrine Abayou France salariée 3 HAYANI ABDEL BELGIUM trade union 4 Ariadna Abeltina Latvia Trade Union Officer General Secretary FSC 5 Roberto Abenia España CCOO Aragón 6 Pascal Abenza France Délégué Syndical Groupe 7 Jacques ADAM Luxembourg membre du syndicat 8 Lenka Adamcikova Slowakei Member of works 9 Ole Einar Adamsrød Norway Trade Union 10 Paula Adao Luxembourg Déléguée 11 Nicolae Adrian România Union member 12 Costache Adrian Alin Romania Trade union 13 Pana Adriana Laura România Member of works council 14 Bert Aerts Belgium member of works council 15 Annick Aerts Belgium trade union 16 Sascha Aerts België 200 Secrétaire Générale UL 17 Odile AGRAFEIL FRANCE CGT 18 Oscar Aguado España Miembro comité empresa 19 Fátima Aguado Queipo Spain Trade union 20 Agustin Aguila Mellado España Miembro del Sindicato SECRETARIO UGT ADIF 21 HERNANDEZ AGUILAR OSWALD BARCELONA 22 Antonio Angel Aguilar Fernández España Trade Union 23 Jaan Aiaots Estonia Trade union SYNDICAT SYNPTAC-CGT 24 Nora AINECHE FRANCE PARIS FRANCE 25 Raul Aira España miembro comité empresa 26 Alessandra Airaldi Italy TRADE union 27 Juan Miguel Aisa Spain Member of works council 28 Juan-Miguel AISA Spain EWC Membre élu du comité européen Driver Services 29 Sylvestre AISSI France Norauto 30 Sara Akervall Sweden EWC 31 Michiel Al Netherlands trade union official 32 Nickels Alain Luxemburg Trade Union 33 MAURO ALBANESE FRANCE SYNDICAT 34 Michela Albarello -

Nursing, Council on Peripheral Vascular Disease, and Council on Clinical Cardiology
Guidelines for the Early Management of Patients With Acute Ischemic Stroke : A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association Edward C. Jauch, Jeffrey L. Saver, Harold P. Adams, Jr, Askiel Bruno, J.J. (Buddy) Connors, Bart M. Demaerschalk, Pooja Khatri, Paul W. McMullan, Jr, Adnan I. Qureshi, Kenneth Rosenfield, Phillip A. Scott, Debbie R. Summers, David Z. Wang, Max Wintermark and Howard Yonas on behalf of the American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Peripheral Vascular Disease, and Council on Clinical Cardiology Stroke. 2013;44:870-947; originally published online January 31, 2013; doi: 10.1161/STR.0b013e318284056a Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2013 American Heart Association, Inc. All rights reserved. Print ISSN: 0039-2499. Online ISSN: 1524-4628 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://stroke.ahajournals.org/content/44/3/870 Data Supplement (unedited) at: http://stroke.ahajournals.org/content/suppl/2013/01/29/STR.0b013e318284056a.DC1.html Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. -

Are Also Chapters on Education for the Culturally Disadvantaged, Crime
DOCUMEN T RESUME ED 024 703 UD 006 450 By- Tumin, Melvin M., Ed. Research Annual on Intergroup Relations, 1965: A Research Study of the Anti-DefamationLeague of B'ned B'rith. B'nai B'rith, New York, N.Y. Anti-Defamation League. Pub Date 66 Note- 185p. Available from-Frederick A. Praeger, Inc.,I I 1 Fourth Avenue, New York, N.Y. 10003 ($1.95). EDRS Price MF-0.75 HC-$9.35 Descriptors- Action Programs (Community), *Annotated Bibliographies, Attitudes, Civil Rights, Crime, Culturally Disadvantaged, Delinquency, Educational Opportunities, Ethnic Groups. *Intergroup Relations, International Education, Race, Religious Cultural Groups, *Research Reviews (Publications), Social Discrimination This annual bulletin offers digests of research in intergroup relations during the period of September. 1964 to April, 1965. The reported studiesare grouped under the rubrics of. (1) researchin attitudes. (2) studies in the characteristics, structure, and position ofethnic,racial,religious, and national groups;(3) patterns of discrimination. segregation, desegregation. and "integration; and (4) civil rights. There arealso chapters on educationforthe culturallydisadvantaged,crime and delinquency, the radical right, and miscellaneous studies. One section is devoted to various action programs relevant to intergroup relations. (NH) 113:-DIPARTMENT OF HEALTH, EDUCATION & WELFARE OFFICE OF EDUCATION THIS DOCUMENT HAS BEEN REPRODUCED EXACTLY AS RECEIVED FROM THE I PERSON OR ORGANIZATIONORICIIIATIIICIvIED. Ilm ITII.DrIIIITC ilE uittli aro rvInt., InIFI:.0 V. 1.11%-"I'MONS STATED DO NOT NECESSARILY REPRESENT OFFICIAL OFFICE OF EDUCATION 1POSITION OR POLICY. ResearchAnnual on Intergroup Relations1965 "A RESEARCH STUDYOF THE ANTI-DEFAMATION LEAGUEOF B'NAI B'RITH A clothbound editionof the Research Annualis being published simultaneouslyby Frederick A. -

UPDATED: 12 June 2008
UPDATED: 3 December 2009 CASE-LAW REFERENCES OF JUDGMENTS AND PUBLISHED DECISIONS - A - A. and E. Riis v. Norway (no. 2), no. 16468/05, § …, 17 January 2008 A. and E. Riis v. Norway, no. 9042/04, § …, 31 May 2007 A. and Others v. Denmark, 8 February 1996, § …, Reports of Judgments and Decisions 1996-I A. and Others v. the United Kingdom [GC], no. 3455/05, § …, ECHR 2009-… A. and Others v. Turkey, no. 30015/96, § …, 27 July 2004 A. E. v. Poland, no. 14480/04, § …, 31 March 2009 A. v. France, 23 November 1993, § …, Series A no. 277-B A. v. Italy (friendly settlement), no. 40453/98, § …, 9 October 2003 A. v. Norway, no. 28070/06, § …, 9 April 2009 A. v. the United Kingdom, 23 September 1998, § …, Reports of Judgments and Decisions 1998-VI A. v. the United Kingdom, no. 35373/97, § …, ECHR 2002-X A. Yılmaz v. Turkey, no. 10512/02, § …, 22 July 2008 A.A.U. v. France, no. 44451/98, § …, 19 June 2001 A.B. v. Italy, no. 41809/98, § …, 8 February 2000 A.B. v. Poland, no. 33878/96, § …, 20 November 2007 2 A.B. v. Slovakia, no. 41784/98, § …, 4 March 2003 A.B. v. the Netherlands, no. 37328/97, § …, 29 January 2002 A.C. v. Italy, no. 44481/98, § …, 1 March 2001 A.D. v. Turkey, no. 29986/96, § …, 22 December 2005 A.D.T. v. the United Kingdom, no. 35765/97, § …, ECHR 2000-IX A.G. v. Italy, no. 66441/01, § …, 9 October 2003 A.H. v. Finland, no. 46602/99, § …, 10 May 2007 A.J. -

Second Jacket Mailing First Name Last Name Pauline Aamodt
Second Jacket Mailing First Name Last Name Pauline Aamodt Amanda Aarsvold Allison Abe Bill Aberg Tanya Abernethy Mark Abrahamson Dominic Abram Melissa Achten Romy Ackerberg Brett Adams Eric Adams Ian Adams Mallory Adams Michele Adams Nikk Adams Parker Adams Trish Adamson Danielle Adank Matt Adasm Hailey Aderman Mary Adkins Bethany Aeling Jeffery Agaton Howes Payton Agen Gaurav Aggarwal Valerie Aggerbeck Eliana Agudelo Juan Aguilar Paul Ahearn Brianna Ahern Kristy Ahlbrecht Monica Ahlman Amy Aho Jon Aho Marko Ahokas Jennifer Ahonen Jonathan Aikman Kate Aikman Henrietta Aitken Amanda Akason Kimberly Alaspa Paul Albares Tony Albeck Francine Albers Siegfried Alicia Albrecht Catie Albrecht Mark Albrecht Mary Albrecht Michael Albrecht Phil Albu Juan Carlos Alcayaga Ben Alcorn Teresa Aldach Rachel Alderman Robert Alderson Paul Aldrich Tim Aldrich Brian Alementi Cheryl Alementi Elizabeth Alesch Michelle Allard Ann Allen Julie Allen Lynn Allen Molly Allen Terri Allen Kelly Allgaier Brian Allison Esther Almeidas Caron Alten Edgar Alvarez Emma Alvarez Lily Alvarez Sergio Alvarez Angela Amazi Linda Amendola Mary Ames Jon Ameter Hector Amezcua Karen Amidon Patricia Amidon Susan Amidon Lindsey Amistadi Nana Amoako Rob Amott Elliot Amundson Jill Amundson Jacob Anason Erik Anderberg David Anderholm Julie Anderholm Emily Andersen Nick Andersen Alan Anderson Alexa Anderson Anna Anderson Becca Anderson Brad Anderson Brent Anderson Brian Anderson Caleb Anderson Carla Anderson Chad Anderson Chelsea Anderson Chris Anderson Chris Anderson Chris Anderson Danielle -
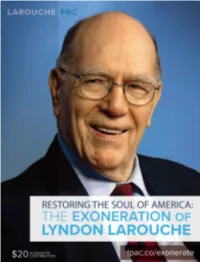
Lyndon Larouche Political Action Committee LAROUCHE PAC Larouchepac.Com Facebook.Com/Larouchepac @Larouchepac
Lyndon LaRouche Political Action Committee LAROUCHE PAC larouchepac.com facebook.com/larouchepac @larouchepac Restoring the Soul of America THE EXONERATION OF LYNDON LAROUCHE Table of Contents Helga Zepp-LaRouche: For the Exoneration of 2 the Most Beautiful Soul in American History Obituary: Lyndon H. LaRouche, Jr. (1922–2019) 9 Selected Condolences and Tributes 16 Background: The Fraudulent 25 Prosecution of LaRouche Letter from Ramsey Clark to Janet Reno 27 Petition: Exonerate LaRouche! 30 Prominent Petition Signers 32 Prominent Signers of 1990s Statement in 36 Support of Lyndon LaRouche’s Exoneration LLPPA-2019-1-0-0-STD | COPYRIGHT © MAY 2019 LYNDON LAROUCHE PAC, ALL RIGHTS RESERVED. Cover photo credits: EIRNS/Stuart Lewis and Philip Ulanowsky INTRODUCTION For the Exoneration of the Most Beautiful Soul in American History by Helga Zepp-LaRouche There is no one in the history of the United States to my knowledge, for whom there is a greater discrep- ancy between the image crafted by the neo-liberal establishment and the so-called mainstream media, through decades of slanders and co- vert operations of all kinds, and the actual reality of the person himself, than Lyndon LaRouche. And that is saying a lot in the wake of the more than two-year witch hunt against President Trump. The reason why the complete exoneration of Lyn- don LaRouche is synonymous with the fate of the United States, lies both in the threat which his oppo- nents pose to the very existence of the U.S.A. as a republic, and thus for the entire world, it system, the International Development Bank, which and also in the implications of his ideas for America’s fu- he elaborated over the years into a New Bretton Woods ture survival. -

Nobilitashungariae: List of Historical Surnames of The
nobilitashungariae: List of Historical Surnames of the Hungarian Nobility / A magyar történelmi nemesség családneveinek listája <http://docs.lib.purdue.edu/clcweblibrary/nobilitashungariae> Steven TÖTÖSY de ZEPETNEK Comp. & Ed. West Lafayette: Purdue University Press, 2010-. ISSN 1923-9580 ©Steven Tötösy de Zepetnek & Purdue University Press version 2021.03.03. verzió corrections: / helyesbítések: <[email protected]> Contents / Tartalom 1) Introduction / Bevezető 2) Bibliotheca selecta familiarium nobilium et armae Hungariae Selected Sources of Genealogies and Heraldry of Historical Hungarian Nobility / Szemelt forrásai a magyar történelmi nemesség genealógiájának és címertanának 3) nobilitashungariae: List of Historical Surnames of the Hungarian Nobility / A magyar történelmi nemesség családneveinek listája 2 nobilitashungariae: List of Historical Surnames of the Hungarian Nobility / A magyar történelmi nemesség családneveinek listája Comp. & Ed. Tötösy de Zepetnek, Steven <http://docs.lib.purdue.edu/clcweblibrAry/nobilitAshungariAe> Main Title: Tötösy de Zepetnek, Steven. nobilitashungariae: List of Historical Surnames of the Hungarian Nobility / A magyar történelmi nemesség családneveinek listája Published/Created 2010- ISSN 1923-9580 Tötösy de Zepetnek, Steven (1950) ©Tötösy de Zepetnek, Steven & Purdue University Press Description: 120 pages; bibliography ISSN digital (pdf): ISSN 1923-9580 nobilitashungariae: List of Historical Surnames of the Hungarian Nobility / A magyar történelmi nemesség családneveinek listája 3 Comp. & Ed. Tötösy de Zepetnek, Steven <http://docs.lib.purdue.edu/clcweblibrAry/nobilitAshungariAe> 1) Introduction / Bevezető Hungarian (Magyar) nobility is documented since the Magyar con- A magyar nemesség a honfoglalás korától (9. század) dokumentált. A quest of Pannonia in the 9th century. In the 14th-20th centuries nobi- 14.-20. századokban magyar nemesség egy uralkodó által adományozott lity is based on a patent of nobility (armales) with a coat-of-arms címeres nemeslevél (armales) következménye és 1848-ig jogi osztály. -

Written Comments Submitted To
Submitted Electronically to [email protected] Ms. Maria Ellis Executive Secretary for MEDCAC Centers for Medicare & Medicaid Services Office of Clinical Standards and Quality Coverage and Analysis Group, S3–02–01, 7500 Security Boulevard, Baltimore, MD 21244 Ms. Ellis: The undersigned groups have co-sponsored and or endorsed the 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS Guideline on the Management of PatientsWith Extracranial Carotid and Vertebral Artery Disease. We recommend our analysis and recommendations be the primary basis for determining Medicare’s Coverage of treatments for carotid atherosclerosis. The development of this guideline involved an extensive review of all available literature and writing committee members had great expertise in the various treatments for carotid atherosclerosis. The recommendations are based on a comprehensive review of the literature relevant to carotid and vertebral artery interventions through May 2010. The document was reviewed by 55 external reviewers, including individuals nominated by each of the ASA, ACCF, AHA, AANN, AANS, ACEP, American College of Physicians, ACR, ASNR, CNS, SAIP, SCAI, SCCT, SIR, SNIS, SVM, and SVS, and by individual content reviewers, including members from the ACCF Catheterization Committee, ACCF Interventional Scientific Council, ACCF Peripheral Vascular Disease Committee, ACCF Surgeons’ Scientific Council, ACCF/SCAI/SVMB/SIR/ASITN Expert Consensus Document on Carotid Stenting, ACCF/AHA Peripheral Arterial Disease Guideline Writing Committee, AHA Peripheral Vascular Disease Steering Committee, AHA Stroke Leadership Committee, and individual nominees. All information on reviewers’ relationships with industry and other entities was distributed to the writing committee and is published in this document (Appendix 2). -

City of Newton Cy 2008 Earnings Report
CITY OF NEWTON CY 2008 EARNINGS REPORT Employee Name Department Job Title Regular Overtime Detail Longevity Other Total Earnings ANDREWS, GREGORY ASSESSING DEPUTY DIR-ASSESSING 90,007.34 0.00 0.00 775.00 796.15 91,578.49 ANDREWS, LOUISE A ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 BERESON, LOUISE Z ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 CARUSO, MARIE ASSESSING DATA CONTROL SPECIALIST 44,778.56 0.00 0.00 650.00 602.25 46,030.81 COHEN, ALLAN S ASSESSING ASST RESID ASSESSOR 72,936.98 0.00 0.00 575.00 13,152.86 86,664.84 COTOIA, ALICE E ASSESSING EXCISE PROCESSOR 45,726.67 0.00 0.00 950.00 -247.86 46,428.81 CRUMMETT, RUANE ASSESSING ASSESSOR SEASONAL 18,857.03 0.00 0.00 0.00 0.00 18,857.03 DEPASQUALE, LORRAINE M ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 DESMOND, ELEANOR P ASSESSING SR CITIZEN TAX WORK 736.00 0.00 0.00 0.00 0.00 736.00 DEZOTELL, ESTELLE L ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 DOBIES, STANLEY ASSESSING EXEMPTION COORDINATOR 53,206.78 0.00 0.00 850.00 494.05 54,550.83 DRAPKIN, SYLVIA G ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 DROMEY, ELIZABETH ASSESSING CHAIRMAN - ASSESSORS 110,657.83 0.00 0.00 775.00 930.14 112,362.97 ETHIER, LILY N ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 FALLON, PHYLLIS A ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 FANELLI, MARY E ASSESSING SR CITIZEN TAX WORK 750.00 0.00 0.00 0.00 0.00 750.00 FLYNN, JOSEPH A ASSESSING APPRAISAL TECH 53,206.78 0.00 -

Ucm 451284.Pdf
Guidelines for the Early Management of Patients With Acute Ischemic Stroke : A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association Edward C. Jauch, Jeffrey L. Saver, Harold P. Adams, Jr, Askiel Bruno, J.J. (Buddy) Connors, Bart M. Demaerschalk, Pooja Khatri, Paul W. McMullan, Jr, Adnan I. Qureshi, Kenneth Rosenfield, Phillip A. Scott, Debbie R. Summers, David Z. Wang, Max Wintermark and Howard Yonas on behalf of the American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Peripheral Vascular Disease, and Council on Clinical Cardiology Stroke. 2013;44:870-947; originally published online January 31, 2013; doi: 10.1161/STR.0b013e318284056a Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2013 American Heart Association, Inc. All rights reserved. Print ISSN: 0039-2499. Online ISSN: 1524-4628 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://stroke.ahajournals.org/content/44/3/870 Data Supplement (unedited) at: http://stroke.ahajournals.org/content/suppl/2013/01/29/STR.0b013e318284056a.DC1.html Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. -

International Congress Engineering of Advanced Materials ICEAM2017
International Congress Engineering of Advanced ICEAM2017 Materials ICEAM2017 10 – 12 October 2017 · Erlangen · Germany International Congress Engineering of Advanced Materials www.iceam2017.fau.de www.iceam2017.fau.de Content 1 – Welcome 1 2 – Information on EAM and FAU 2 3 – Confirmed Speakers (Plenary, EAM Talk, Keynote) 3 4 – Scientific Organizing Committee and Congress Office 4 5 – ICEAM2017 Program 5 6 – Plenary Talk Abstracts 10 7 – EAM Talk Abstracts 17 8 – Keynote Talk Abstracts 25 9 – Session Talk Abstracts 42 10 – Poster Presentation Abstracts 129 11 – List of Participants 230 Welcome to the International Congress Engineering of Advanced Materials ICEAM2017 10 – 12 October 2017 Erlangen, Germany It is our pleasure to welcome you to Erlangen for the International Congress Engineering of Advanced Materials ICEAM2017, organized by the Cluster of Excellence – Engineering of Advanced Materials (EAM) at the Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU). ICEAM2017 provides a showcase for 10 years of interdisciplinary research at EAM and places it in an international context for state-of-the-art science and engineering research. The congress addresses local, national and international researchers working in the fields where EAM is active. The program themes will focus on EAM’s four application fields: Nanoelectronic Materials, Photonic and Optical Materials, Catalytic Materials and Lightweight Materials. Furthermore, the key role played by our cross-sectional topics, namely Functional Particle Systems, Nanoanalysis and Microscopy, and Multiscale Modeling and Simulation will be emphasized throughout the congress. With a mix of high profile external invited plenary, keynote and session talks, combined with excellent internal contributions and a high-quality poster session, we hope for a wide range of inspiring interactions and fruitful discussions. -

Bone Morphogenetic Proteins in Vascular Homeostasis and Disease
Downloaded from http://cshperspectives.cshlp.org/ on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Bone Morphogenetic Proteins in Vascular Homeostasis and Disease Marie-Jose´Goumans,1 An Zwijsen,2,3 Peter ten Dijke,1,4 and Sabine Bailly5,6,7 1Department of Molecular Cell Biology, Leiden University Medical Center, 2300 RC Leiden, The Netherlands 2VIB Center for the Biology of Disease, 3000 Leuven, Belgium 3KU Leuven Department of Human Genetics, 3000 Leuven, Belgium 4Cancer Genomics Centre Netherlands, Leiden University Medical Center, 2300 RC Leiden, The Netherlands 5Institut National de la Sante´ et de la Recherche Me´cale (INSERM), U1036, 38000 Grenoble, France 6Laboratoire Biologie du Cancer et de l’Infection, Commissariat a` l’E´nergie Atomique et aux Energies Alternatives, Biosciences and Biotechnology Institute of Grenoble, 38000 Grenoble, France 7University of Grenoble Alpes, 38000 Grenoble, France Correspondence: [email protected]; [email protected] It is well established that control of vascular morphogenesis and homeostasis is regulated by vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), Delta-like 4 (Dll4), angiopoietin, and ephrin signaling. It has become clear that signaling by bone morphogenetic proteins (BMPs), which have a long history of studies in bone and early heart development, are also essential for regulating vascular function. Indeed, mutations that cause deregulated BMP signaling are linked to two human vascular diseases, hereditary hemorrhagic telangiectasia and pulmonary arterial hypertension. These observations are corroborated by data obtained with vascular cells in cell culture and in mouse models. BMPs are required for normal endothelial cell differentiation and for venous/arterial and lymphatic specification.