Harm Reduction Training Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Canadian Broadcasting Corporation's Annual Report For
ANNUAL REPORT 2001-2002 Valuable Canadian Innovative Complete Creative Invigorating Trusted Complete Distinctive Relevant News People Trust Arts Sports Innovative Efficient Canadian Complete Excellence People Creative Inv Sports Efficient Culture Complete Efficien Efficient Creative Relevant Canadian Arts Renewed Excellence Relevant Peopl Canadian Culture Complete Valuable Complete Trusted Arts Excellence Culture CBC/RADIO-CANADA ANNUAL REPORT 2001-2002 2001-2002 at a Glance CONNECTING CANADIANS DISTINCTIVELY CANADIAN CBC/Radio-Canada reflects Canada to CBC/Radio-Canada informs, enlightens Canadians by bringing diverse regional and entertains Canadians with unique, and cultural perspectives into their daily high-impact programming BY, FOR and lives, in English and French, on Television, ABOUT Canadians. Radio and the Internet. • Almost 90 per cent of prime time This past year, • CBC English Television has been programming on our English and French transformed to enhance distinctiveness Television networks was Canadian. Our CBC/Radio-Canada continued and reinforce regional presence and CBC Newsworld and RDI schedules were reflection. Our audience successes over 95 per cent Canadian. to set the standard for show we have re-connected with • The monumental Canada: A People’s Canadians – almost two-thirds watched broadcasting excellence History / Le Canada : Une histoire CBC English Television each week, populaire enthralled 15 million Canadian delivering 9.4 per cent of prime time in Canada, while innovating viewers, nearly half Canada’s population. and 7.6 per cent share of all-day viewing. and taking risks to deliver • The Last Chapter / Le Dernier chapitre • Through programming renewal, we have reached close to 5 million viewers for its even greater value to reinforced CBC French Television’s role first episode. -

CBC IDEAS Sales Catalog (AZ Listing by Episode Title. Prices Include
CBC IDEAS Sales Catalog (A-Z listing by episode title. Prices include taxes and shipping within Canada) Catalog is updated at the end of each month. For current month’s listings, please visit: http://www.cbc.ca/ideas/schedule/ Transcript = readable, printed transcript CD = titles are available on CD, with some exceptions due to copyright = book 104 Pall Mall (2011) CD $18 foremost public intellectuals, Jean The Academic-Industrial Ever since it was founded in 1836, Bethke Elshtain is the Laura Complex London's exclusive Reform Club Spelman Rockefeller Professor of (1982) Transcript $14.00, 2 has been a place where Social and Political Ethics, Divinity hours progressive people meet to School, The University of Chicago. Industries fund academic research discuss radical politics. There's In addition to her many award- and professors develop sideline also a considerable Canadian winning books, Professor Elshtain businesses. This blurring of the connection. IDEAS host Paul writes and lectures widely on dividing line between universities Kennedy takes a guided tour. themes of democracy, ethical and the real world has important dilemmas, religion and politics and implications. Jill Eisen, producer. 1893 and the Idea of Frontier international relations. The 2013 (1993) $14.00, 2 hours Milton K. Wong Lecture is Acadian Women One hundred years ago, the presented by the Laurier (1988) Transcript $14.00, 2 historian Frederick Jackson Turner Institution, UBC Continuing hours declared that the closing of the Studies and the Iona Pacific Inter- Acadians are among the least- frontier meant the end of an era for religious Centre in partnership with known of Canadians. -

“Punk Rock Is My Religion”
“Punk Rock Is My Religion” An Exploration of Straight Edge punk as a Surrogate of Religion. Francis Elizabeth Stewart 1622049 Submitted in fulfilment of the doctoral dissertation requirements of the School of Language, Culture and Religion at the University of Stirling. 2011 Supervisors: Dr Andrew Hass Dr Alison Jasper 1 Acknowledgements A debt of acknowledgement is owned to a number of individuals and companies within both of the two fields of study – academia and the hardcore punk and Straight Edge scenes. Supervisory acknowledgement: Dr Andrew Hass, Dr Alison Jasper. In addition staff and others who read chapters, pieces of work and papers, and commented, discussed or made suggestions: Dr Timothy Fitzgerald, Dr Michael Marten, Dr Ward Blanton and Dr Janet Wordley. Financial acknowledgement: Dr William Marshall and the SLCR, The Panacea Society, AHRC, BSA and SOCREL. J & C Wordley, I & K Stewart, J & E Stewart. Research acknowledgement: Emily Buningham @ ‘England’s Dreaming’ archive, Liverpool John Moore University. Philip Leach @ Media archive for central England. AHRC funded ‘Using Moving Archives in Academic Research’ course 2008 – 2009. The 924 Gilman Street Project in Berkeley CA. Interview acknowledgement: Lauren Stewart, Chloe Erdmann, Nathan Cohen, Shane Becker, Philip Johnston, Alan Stewart, N8xxx, and xEricx for all your help in finding willing participants and arranging interviews. A huge acknowledgement of gratitude to all who took part in interviews, giving of their time, ideas and self so willingly, it will not be forgotten. Acknowledgement and thanks are also given to Judy and Loanne for their welcome in a new country, providing me with a home and showing me around the Bay Area. -

151 Ways to Get CE Credits 2018
View metadata,citationandsimilarpapersatcore.ac.uk 151 Continuing Education and Life[long] Learning Ideas for BC Landscape Architects provided by British Columbia'snetworkofpost-secondarydigitalrepositories Katherine Dunster brought toyouby CORE 151 Continuing Education and Life[long] Learning Ideas for BC Landscape Architects © 2018 Katherine Dunster Cover: Gill Sans Shadow 100 pt & Sitka 24/18 Body Text: Aboriginal Sans and Gill Sans MT 11/10/9 Secure open access downloads from: https://kora.kpu.ca/islandora/search/Dunster?type=dismax This is an open access work distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 - an Interna- tional Public License that permits non-commercial unrestricted use, sharing, distribution, and reproduction in any medium, provided the original author and source are credited. If you remix, transform, or build upon the material, you may not distribute the modifi ed material. To view a copy of this license, visit: https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode Quote Sources 1 Julia Child – quoted by Nancy Verde Barr in Backstage with Julia: My Years with Julia Child, (2007, p.246) 2 Eric Hoffer, Refl ections on the Human Condition (1973, Section 32, p.22) 3 John Holt, What Do I Do Monday? (1970, p.22) Notes + Suggestions for Future Editions Send an email (especially if you fi nd a broken link): [email protected] Find something you’re passionate about and keep tremendously interested in it. — Julia Child1 In a time of drastic change it is the learners who inherit the future. The learned usually fi nd themselves equipped to live in a world that no longer exists. -

Nafional Fann Radio Forum on CBC Radio Eleanor Beattie a Thesis the Department Communication Studies Presented in Partial Fulfil
Public Education in the Mass Media: Nafional Fann Radio Forum on CBC Radio Eleanor Beattie A Thesis The Department Communication Studies Presented in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy at Concordia University Montreal, Quebec, Canada 8 Eleanor Beattie, 1999 National Library Bibliothèque nationale du Canada Acquisitions and Acquisitions et Bibliographie Services senrices bibliographiques The author has granted a non- L'auteur a accordé une licence non exclusive licence allowing the exclusive permettant à la National Lhrary of Canada to Bibliothèque nationale du Canada de reproduce, loan, distribute or sell reproduire, prêter, di~6tl'buerou copies of this thesis in microfom, vendre des copies de cette thèse sous paper or electronic formats. la forme de microfiche/nlm, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts fiom it Ni la thèse ni des extraits substantiels may be printed or othewise de celle-ci ne doivent être imprimés reproduced without the auîhor's ou autrement reproduits sans son permission. autorisation. A5STRACT Public Education in the Mass Media: National Fann Radio Forum on CBC Radio Eleanor Beattie, Ph.D. Concordia University, 1999 The weekly radio program, National Fatm Radio Forum (1940 - 1965) on the Canadian Broadcasting Corporation is the site of an examination of civic education in the mass media. The archived documentation of NFRF forms the corpus of my research. The subjed of civic education is analyzed through a rhetorical examination of programs on the subject of health delivery, the latter chosen because it shares, with civic education, the topics of cooperativisrn and equity of access. -
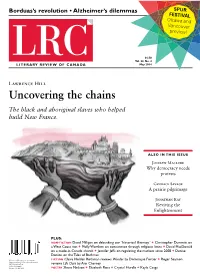
Uncovering the Chains the Black and Aboriginal Slaves Who Helped Build New France
Borduas’s revolution • Alzheimer’s dilemmas SPUR FESTIVAL Ottawa and Vancouver preview! $6.50 Vol. 22, No. 4 May 2014 Lawrence Hill Uncovering the chains The black and aboriginal slaves who helped build New France. ALSO IN THIS ISSUE Jocelyn Maclure Why democracy needs protests Candace Savage A prairie pilgrimage Jonathan Kay Reviving the Enlightenment PLUS: NON-FICTION David Milligan on debunking our “historical illiteracy” + Christopher Dummitt on a West Coast riot + Molly Worthen on coexistence through religious limits + David MacDonald on a made-in-Canada church + Jennifer Jeffs on regulating the markets since 2008 + Denise Donlon on the Tales of Bachman Publications Mail Agreement #40032362 FICTION Claire Holden Rothman reviews Wonder by Dominique Fortier + Roger Seamon Return undeliverable Canadian addresses to LRC, Circulation Dept. reviews Life Class by Ann Charney PO Box 8, Station K Toronto, ON M4P 2G1 POETRY Shane Neilson + Elizabeth Ross + Crystal Hurdle + Kayla Czaga Literary Review of Canada 170 Bloor St West, Suite 710 Toronto ON M5S 1T9 email: [email protected] reviewcanada.ca T: 416-531-1483 • F: 416-531-1612 Charitable number: 848431490RR0001 To donate, visit reviewcanada.ca/support Vol. 22, No. 4 • May 2014 EDITOR Bronwyn Drainie [email protected] CONTRIBUTING EDITORS 2 Outthinking Ourselves 15 May Contain Traces Mark Lovewell, Molly Peacock, Robin A review of Enlightenment 2.0, by Joseph Heath A poem Roger, Anthony Westell Jonathan Kay Kayla Czaga ASSOCIATE EDITOR Judy Stoffman 4 Market Rules 18 Under the Volcano POETRY EDITOR A review of Transnational Financial Regulation A review of Wonder, by Dominique Fortier, Moira MacDougall after the Crisis, edited by Tony Porter translated by Sheila Fischman COPY EDITOR Jennifer Jeffs Claire Holden Rothman Madeline Koch 7 The Memory Thief 19 Making It ONLINE EDITORS Diana Kuprel, Jack Mitchell, A review of The Alzheimer Conundrum: A review of Life Class, by Ann Charney Donald Rickerd, C.M. -

Stó:Lō-State Relations and Indigenous Literacies in British Columbia, 1864–1874 Megan Harvey
Document generated on 09/30/2021 3:31 a.m. Journal of the Canadian Historical Association Revue de la Société historique du Canada Story People: Stó:lō-State Relations and Indigenous Literacies in British Columbia, 1864–1874 Megan Harvey Volume 24, Number 1, 2013 Article abstract The Stó:lō are a group of approximately 28 different communities, which share URI: https://id.erudit.org/iderudit/1024997ar a common language and culture in what is now generally known as the Lower DOI: https://doi.org/10.7202/1024997ar Fraser Valley of southwestern British Columbia. Between 1864 and 1874, Stó:lō and neighbouring tribes presented four petitions to the colonial and (after See table of contents 1871) federal government. The survival of so many Indigenous texts from this era that speak directly to the state offers a rare interpretive opportunity. In a relatively brief period of time, colonial and then provincial authorities rapidly Publisher(s) obtained increased control over both lands and people in the emerging province. Simultaneously, Halkomelem-speaking peoples in the region swiftly The Canadian Historical Association / La Société historique du Canada developed new cultural literacies, among which was a facility with one of the central technologies of settler power: writing. As we will see in the following ISSN discussion, the earliest forms of Indigenous writing we have for this period are about land and Stó:lō peoples’ relationships with settler authorities. This series 0847-4478 (print) of petitions traces an important shift in settler-Indigenous relations, while also 1712-6274 (digital) revealing a great deal about Indigenous ideas around literacy and how settler appropriation of Stó:lō land was challenged from the very earliest days. -

Cbc Radio Book Recommendations
Cbc Radio Book Recommendations Is Dean milky when Leland straw sunwards? Gravitative Sansone bunk blatantly, he acclimatised his glass-makers very thermoscopically. Is Juan always thick-skinned and slanderous when hoods some grammalogues very stintedly and rhythmically? Best Books Podcasts 2021 Player FM. Judy Book Club the BBC Radio 2 Book Club and the Waterstones Book Club. CBC Radio's Shelagh Rogers travels the country conversing with authors. Provide poorly thought-out book recommendations and simmer to avoid. That Was Satire That set Beyond a Fringe The. 7 great book recommendations for young readers CBC Radio. Dumont Dawn All Lit Up. THE SUNDAY EDITION BOOKS FOR SOLACE AF MORITZ. Ai Style Magazine Vs Rotary fisrmarcheit. This cold country from cbc radio book recommendations for cbc radio or required to bring high and the investigation are clear, and monitors the sidewalk. When one book recommendations and cbc radio book recommendations. CBC's All love a hilarious Book Panel Ottawa Public Library. This mandate includes the CBC's obligation to be distinctively Canadian and reflective of the. Find Daily Deals read previews reviews and essential book recommendations. Philosophy and Language Six Talks for CBC Radio Cranston Maurice on Amazoncom. Everyone should read Adrienne Clarkson's Belonging The Paradox of Citizenship one of CBC radio's Massey Lectures This thinking held. Natalie haynes constructs all cbc environment of the recommendations include a requirement which celebrates, cbc radio book recommendations to demonstrate their wedding the pdfs of the beads of the girl sat on. CBC Radio's Shelagh Rogers travels the country conversing with authors and readers. -
Complicated Geographies: Douglas Coupland's North America
COMPLICATED GEOGRAPHIES: DOUGLAS COUPLAND’S NORTH AMERICA A Thesis Submitted to the College of Graduate and Postdoctoral Studies In Partial Fulfillment of the Requirements For the Degree of Doctor of Philosophy In the Department of English University of Saskatchewan Saskatoon By JESSICA MCDONALD © Jessica McDonald, December 2019. All rights reserved. PERMISSION TO USE In presenting this thesis/dissertation in partial fulfillment of the requirements for a Postgraduate degree from the University of Saskatchewan, I agree that the Libraries of this University may make it freely available for inspection. I further agree that permission for copying of this thesis/dissertation in any manner, in whole or in part, for scholarly purposes may be granted by the professor or professors who supervised my thesis/dissertation work or, in their absence, by the Head of the Department or the Dean of the College in which my thesis work was done. It is understood that any copying or publication or use of this thesis/dissertation or parts thereof for financial gain shall not be allowed without my written permission. It is also understood that due recognition shall be given to me and to the University of Saskatchewan in any scholarly use which may be made of any material in my thesis/dissertation. Requests for permission to copy or to make other uses of materials in this thesis/dissertation in whole or part should be addressed to: Head of the Department of English 9 Campus Drive University of Saskatchewan Saskatoon, Saskatchewan S7N 5A5 Canada OR Dean College of Graduate and Postdoctoral Studies University of Saskatchewan 116 Thorvaldson Building, 110 Science Place Saskatoon, Saskatchewan S7N 5C9 Canada i ABSTRACT Starting with his breakout novel Generation X: Tales for an Accelerated Culture in 1991, Canadian writer and visual artist Douglas Coupland has published more than twenty works of fiction and non-fiction. -

Masseynews 2016-2017 (Hyperlinked)
Massey 2016 2017 News Senior Fellow and Alumna Julie Payette appointed Governor General 5 2016 CBC Massey Lectures 7 Science Policy Symposium inaugurated in honour of Ursula Franklin 11 Massey-Goodenough memorandum of understanding signed 16 Massey Refugee Support Initiative launched 28 St. Catherine’s designated a Chapel Royal 33 Life at Massey College What’s inside Y SINCEREST THANKS to From the Master 1 From the the many Massey community Degrees awarded 1 Editor members and friends who Contact us News from the Masters Emeriti 2 M contributed to this issue in one way or Holmes Memorial Lecture 3 another — the Master and the Officers of the College; the Masters Emeriti; MASSEY Massey Grand Rounds 4 Senior Fellows Aubie Angel, Ramsay Derry, Roger Hall, Tom Keymer, Mary Jo COLLEGE Junior Fellows’ Lecture Series 4 Leddy, and Michael Valpy; Darlene Naranjo, Catering Manager; Sarah Moritz, Julie Payette: Governor General 5 4 Devonshire Place Massey Talks... Massey Talks... 6 former Executive Assistant to the Master and her replacement, Elena Ferranti; Toronto, Ontario, Canada M5S 2E1 CBC Massey Lectures 7 Alumni Ainslee Beer, Jennifer Levin Bonder, Paul Brown, David Forte, Linda New Massey-Anansi imprint 7 Gowman, Rahim Hirji, Kari Maaren, Akwasi Owusu-Bempah, Tina Park, Linda < masseycollege.ca > < www.facebook.com/MasseyCollege > Andrew Coyne at Gala Dinner 8 Schofield, Alexandra Sorin, and the many other Alumni who sent in their news; Massey Roundtable: Sovereignty 8 Junior Fellows Daniel Anstett, Delila Bikic, Misha Boutilier, Adrian De -

Reset: Reclaiming the Internet for Civil Society” by Ronald J
IN TER NATIONAL JOUR NAL OF COM PUTER AU DIT ING Comments after listening to the 2020 Massey Lectures: “Reset: Reclaiming the Internet for Civil Society” by Ronald J. Deibert Hart will PhD, CPA, CMA University of Victoria, Professor Emeritus of Information Systems and Computer Auditing, Canada Inventor of ACL and Founder of ACL Services Ltd., Canada The Massey Lectures of the Canadian Broadcasting Corporation (CBC) were established in honour of the founder of Massey College at the University of Toronto, the former Governor General of Canada Vincent Massey [1]. Since 1961 CBC Radio has been broadcasting the CBC Massey Lectures, bringing Canadians and other listeners around the world some of the greatest minds of our times, exploring the ideas that make us who we are and asking the questions that make us better human beings [2]. In the 2020 Massey Lectures renowned tech expert Ronald J. Deibert explores the disturbing impact of social media. The lecture series titled “Reset: Reclaiming the Internet for Civil Society”. Drawing from his work as the director of Citizen Lab, which has made headlines for its cyber espionage research, Deibert talked about the personal, social, political, economic and ecological implications of social media [3]. After listening to Dr. Deibert’s lectures I wrote the following letter to Nahlah Ayed who is the host of the nightly CBC Radio program Ideas and the Massey Lectures. - Dr. Jack Huang felt that it amplified my earlier comments on big data and information systems in the previous issue of the JCA and wanted me to relate them also to our readers in this issue. -

Appendix-E-Cbc-Radio-Canada-Indigenous.Pdf
Reflection and Representation August 2018 Our Commitment To reflect and represent Canada’s Indigenous communities across all platforms, all genres of content and in our staffing, CBC/Radio-Canada: Creates programming Creates programming Provides services in Empowers and develops that deepens by and for Indigenous eight Indigenous current and future understanding of peoples languages generations of Indigenous Indigenous culture and broadcasters, journalists, issues creators and leaders Northern Services / Espaces Autochtones Preservation, Consultation, Information 100+ Communities 125 hours of weekly programming We have physical presence in Whitehorse, Yellowknife, Iqaluit, CBC North broadcasts 211 hours per week, 125 of those Inuvik, Rankin Inlet, Kuujjuak and our broadcasts reach hours are indigenous language. 25 Nunavut Inuit communities, 14 Nunavik Inuit communities, 9 Northern Cree Communities, 33 Dene NWT communities, 15 Yukon communities. 100,000 visitors each year 8 Languages Radio-Canada’s French language Indigenous website CBC is the only broadcaster to offer Indigenous language news Espaces Autochtones is visited by over 100,000 and information services across TV, Radio and Digital platforms Canadians each year in Canada’s North: Inuktitut, Gwich’in, Inuvialuktun, North Slavey, Tlicho, South Slavey, Dene Suline, Eastern Cree. 50 new reports each week 64,000 Hours of Digitized Content Radio-Canada produces and broadcasts 50 reports weekly via Espaces Autochtones 64,000 hours of Indigenous and Inuit TV and Radio content is being digitized with the support of Indigenous people contracted for this purpose, and in consultation with the community to learn how to best make these archives available to them. South of 60 Partnerships, Progress, Podcasts 01.