COPD and Asthma: Differential Diagnosis Is Available At
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -

Legionnaires' Disease
epi TRENDS A Monthly Bulletin on Epidemiology and Public Health Practice in Washington Legionnaires’ disease Vol. 22 No. 11 Legionellosis is a bacterial respiratory infection which can result in severe pneumonia and death. Most cases are sporadic but legionellosis is an important public health issue because outbreaks can occur in hotels, communities, healthcare facilities, and other settings. Legionellosis Legionellosis was first recognized in 1976 when an outbreak affected 11.17 more than 200 people and caused more than 30 deaths, mainly among attendees of a Legionnaires’ convention being held at a Philadelphia hotel. Legionellosis is caused by numerous different Legionella species and serogroups but most epiTRENDS P.O. Box 47812 recognized infections are due to Olympia, WA 98504-7812 L. pneumophila serogroup 1. The extent to which this is due to John Wiesman, DrPH, MPH testing bias is unclear since only Secretary of Health L. pneumophila serogroup 1 is Kathy Lofy, MD identified via commonly used State Health Officer urine antigen tests; other species Scott Lindquist, MD, MPH Legionella pneumophila multiplying and serogroups must be identified in a human lung cell State Epidemiologist, through PCR or culture, tests Communicable Disease www.cdc.gov which are less commonly ordered. Jerrod Davis, P.E. Assistant Secretary The disease involves two clinically distinct syndromes: Pontiac fever, Disease Control and Health Statistics a self-limited flu-like illness without pneumonia; and Legionnaires’ disease, a potentially fatal pneumonia with initial symptoms of fever, Sherryl Terletter Managing Editor cough, myalgias, malaise, and sometimes diarrhea progressing to symptoms of pneumonia which can be severe. Health conditions that Marcia J. -
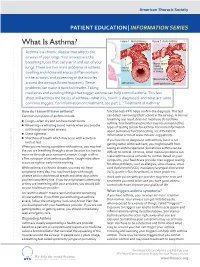
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Pneumonia: Prevention and Care at Home
FACT SHEET FOR PATIENTS AND FAMILIES Pneumonia: Prevention and Care at Home What is it? On an x-ray, pneumonia usually shows up as Pneumonia is an infection of the lungs. The infection white areas in the affected part of your lung(s). causes the small air sacs in your lungs (called alveoli) to swell and fill up with fluid or pus. This makes it harder for you to breathe, and usually causes coughing and other symptoms that sap your energy and appetite. How common and serious is it? Pneumonia is fairly common in the United States, affecting about 4 million people a year. Although for many people infection can be mild, about 1 out of every 5 people with pneumonia needs to be in the heart hospital. Pneumonia is most serious in these people: • Young children (ages 2 years and younger) • Older adults (ages 65 and older) • People with chronic illnesses such as diabetes What are the symptoms? and heart disease Pneumonia symptoms range in severity, and often • People with lung diseases such as asthma, mimic the symptoms of a bad cold or the flu: cystic fibrosis, or emphysema • Fatigue (feeling tired and weak) • People with weakened immune systems • Cough, without or without mucus • Smokers and heavy drinkers • Fever over 100ºF or 37.8ºC If you’ve been diagnosed with pneumonia, you should • Chills, sweats, or body aches take it seriously and follow your doctor’s advice. If your • Shortness of breath doctor decides you need to be in the hospital, you will receive more information on what to expect with • Chest pain or pain with breathing hospital care. -

Chest Pain and Non-Respiratory Symptoms in Acute Asthma
Postgrad Med J 2000;76:413–414 413 Chest pain and non-respiratory symptoms in Postgrad Med J: first published as 10.1136/pmj.76.897.413 on 1 July 2000. Downloaded from acute asthma W M Edmondstone Abstract textbooks. Occasionally the combination of The frequency and characteristics of chest dyspnoea and chest pain results in diagnostic pain and non-respiratory symptoms were confusion. This study was prompted by the investigated in patients admitted with observation that a number of patients admitted acute asthma. One hundred patients with with asthmatic chest pain had been suspected a mean admission peak flow rate of 38% of having cardiac ischaemia, pleurisy, pericardi- normal or predicted were interviewed tis, or pulmonary embolism. It had also been using a questionnaire. Chest pain oc- observed that many patients admitted with curred in 76% and was characteristically a asthma complained of a range of non- dull ache or sharp, stabbing pain in the respiratory symptoms, something which has sternal/parasternal or subcostal areas, been noted previously in children1 and in adult worsened by coughing, deep inspiration, asthmatics in outpatients.2 The aim of this or movement and improved by sitting study was to examine the frequency and char- upright. It was rated at or greater than acteristics of chest pain and other symptoms in 5/10 in severity by 67% of the patients. A patients admitted with acute asthma. wide variety of upper respiratory and sys- temic symptoms were described both Patients and methods before and during the attack. One hundred patients (66 females, mean (SD) Non-respiratory symptoms occur com- age 45.0 (19.7) years) admitted with acute monly in the prodrome before asthma asthma were studied. -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Obliterative Bronchiolitis, Cryptogenic Organising Pneumonitis and Bronchiolitis Obliterans Organizing Pneumonia: Three Names for Two Different Conditions
Eur Reaplr J EDITORIAL 1991, 4, 774-775 Obliterative bronchiolitis, cryptogenic organising pneumonitis and bronchiolitis obliterans organizing pneumonia: three names for two different conditions R.M. du Bois, O.M. Geddes Over the last five years, increasing confusion has has been applied to conditions in which airflow obstruc developed over the use of the terms "bronchiolitis tion is prominent and in which response to treatment is obliterans" and "bronchiolitis obliterans organizing poor. pneumonia". The confusion stems largely from the common use of the term "bronchiolitis obliterans" or "obliterative bronchiolitis" in the diagnostic labels applied "Cryptogenic organizing pneumonitis" or "bronchi· to two entities which are quite distinct clinically but which otitis obliterans organizing pneumonia" (BOOP) bear certain resemblances histologically. Cryptogenic organizing pneumonitis was first described by DAVISON et al. [7] in 1983. The clinical syndrome ObUterative bronchiolitis consisted of breathlessness, malaise, fever, high erythrocyte sedimentation rate (ESR), pneumonic In 1977, GEODES et al. [1] reported the case histories shadowing on chest radiograph with a restrictive of six patients whose clinical condition was characterized pulmonary function defect and low gas transfer coeffi by airways obliteration in association with rheumatoid cient. On histological examination of lung biopsy mate· arthritis. The striking clinical features were of rapidly rial, the typical and distinguishing feature was the progressive breathlessness and the fmding on examination presence of connective tissue within the alveoli, alveolar of a high-pitched mid-inspiratory squeak heard over the ducts and, occasionally, in respiratory bronchioles. This lung fields. Chest radiographs showed hyperinflated lungs connective tissue consisted of "loosely woven fibres of but were otherwise normal. -

Diseases of the Respiratory System (J00-J99) ICD-10-CM
Diseases of the Respiratory System (J00-J99) ICD-10-CM Coverage provided by Amerigroup Inc. This publication contains proprietary information. This material is for informational purposes only. Reference the Centers for Medicare and Medicaid Services (CMS) for more information on Risk Adjustment and the CMS-HCC Model. Redistribution or other use is strictly forbidden This publication is for informational purposes only and is not guaranteed to be without defect. Please reference the current version(s) of the ICD-10-CM codebook, CMS-HCC Risk Adjustment Model, and AHA Coding Clinic for complete code sets and official coding guidance. AGPCARE-0080-19 63321MUPENABS 10/05/16 Diseases of the respiratory system are located in chapter Intermittent asthma which is defined as less 10 of the ICD-10-CM code book; this chapter includes than or equal to two occurrences per week. conditions such as asthma, pneumonia, and chronic Persistent asthma which includes three levels obstructive pulmonary disease (COPD). of severity: Mild: more than two times per week Reporting respiratory conditions Moderate: daily and may restrict Codes for reporting diseases of the respiratory physical activity system in ICD-10-CM feature relatively minor Severe: throughout the day with changes from ICD-9-CM. Most of the changes recurrent severe attacks limiting the involve understanding the medical terminology that ability to breathe the more specific codes include, as well as, the new The fourth character indicates severity, and the general coding structure and rules. fifth identifies whether status asthmaticus or At the beginning of chapter 10 for “Diseases of exacerbation is present. the Respiratory System (J00-J99),” an instructional note states, “When a respiratory condition is Asthma ICD-10-CM description described as occurring in more than one site and Category J45 Asthma is not specifically indexed, it should be classified Includes: to the lower anatomic site.” For example, Allergic: tracheobronchitis is classified to bronchitis with Asthma code J40. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS. -
Right Heart Pressures in Bronchial Asthma
Thorax: first published as 10.1136/thx.26.1.39 on 1 January 1971. Downloaded from Thorax (1971), 26, 39. Right heart pressures in bronchial asthma R. F. GUNSTONE St. George's Hospital, London S.W.1 Right heart pressures, electrocardiograms, blood gases, and peak expiratory flow rates were measured in nine patients admitted to hospital with severe bronchial asthma. Low or normal right heart pressures were found despite electrocardiographic changes in five patients consisting of right atrial P waves, abnormal right axis deviation, and in one patient T-wave changes in pre- cordial leads. These electrocardiographic changes reverted towards normal on recovery of the patient from the asthmatic attack. Electrocardiographic changes suggestive of right The procedure was carried out in the general ward heart embarrassment have been noted in acute with the patient in the sitting position supported at 60 bronchial asthma, particularly right atrial P waves to 90 degrees to the horizontal because orthopnoea (P and abnormal right axis deviation was always present. Immediately after catheterization pulmonale) the peak expiratory flow rate was measured with a (Harkavy and Romanoff, 1942; Miyamato, Wright peak flow meter (Wright and McKerrow, Bastaroli, and Hoffman, 1961; Ambiavagar, 1959) and blood (capillary or arterial) was taken for Jones and Roberts, 1967). These observations measurement of pH, Pco2, and standard bicarbonate raise the possibility that death in bronchial asthma by the Astrup method (Astrup, J0rgensen, Andersen, may be due to acute cor pulmonale although and Engel, 1960). The peak flow rate and electro- copyright. necropsy evidence is against this suggestion (Earle, cardiogram were repeated after recovery. -

Management of Wheeze and Cough in Infants and Pre-Schoo L Children In
nPersonal opinio lManagement of wheeze and cough in infants and pre-schoo echildren in primary car Pauln Stephenso nIntroductio is, well established in adults 2thoughs there remain somer controversy about its diagnosis in children eve Managementa of wheeze and cough in children is sinceh Spelman's uncontrolled study of children wit commonm problem in primary care. In this paper I ai nchronic cough successfully treated according to a tod provide a few useful management tools with regar .asthma protocol 3gWithout the ability to perform lun toe diagnosis, the role of a trial of treatment, and th functione tests in pre-school children, care must b rationalee for referral. For an in-depth review see th takent to exclude other diagnoses. A persisten article. in this journal two years ago by Bush 1 eproductiv coughc may be due solely to chroni catarrhe with postnasal drip, but early referral may b sPresentation of Symptom needed. A persistent dry cough,n worse at night and o exercise,s and without evidence of other diagnose Ity is always worth asking parents what they mean b warrants. a trial of asthma treatment thed term 'wheeze' or 'cough'. The high-pitche musicaln noise of a wheeze usually on expiratio Thef younger the child, the longer the list o shouldy not be confused with the sound of inspirator differentialo diagnoses and the more one has t sstridor. The sound of airflow through secretions i econsider possibilities other than 'asthma'. Thes ddifferent again, and parents may describe their chil linclude upper airways disease, congenital structura 'vomiting'g when, in fact, the child has been coughin diseasel of the bronchi, bronchial or trachea severely and bringing up phlegm or mucus.