Right Heart Pressures in Bronchial Asthma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -
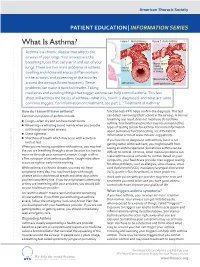
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Diseases of the Respiratory System (J00-J99) ICD-10-CM
Diseases of the Respiratory System (J00-J99) ICD-10-CM Coverage provided by Amerigroup Inc. This publication contains proprietary information. This material is for informational purposes only. Reference the Centers for Medicare and Medicaid Services (CMS) for more information on Risk Adjustment and the CMS-HCC Model. Redistribution or other use is strictly forbidden This publication is for informational purposes only and is not guaranteed to be without defect. Please reference the current version(s) of the ICD-10-CM codebook, CMS-HCC Risk Adjustment Model, and AHA Coding Clinic for complete code sets and official coding guidance. AGPCARE-0080-19 63321MUPENABS 10/05/16 Diseases of the respiratory system are located in chapter Intermittent asthma which is defined as less 10 of the ICD-10-CM code book; this chapter includes than or equal to two occurrences per week. conditions such as asthma, pneumonia, and chronic Persistent asthma which includes three levels obstructive pulmonary disease (COPD). of severity: Mild: more than two times per week Reporting respiratory conditions Moderate: daily and may restrict Codes for reporting diseases of the respiratory physical activity system in ICD-10-CM feature relatively minor Severe: throughout the day with changes from ICD-9-CM. Most of the changes recurrent severe attacks limiting the involve understanding the medical terminology that ability to breathe the more specific codes include, as well as, the new The fourth character indicates severity, and the general coding structure and rules. fifth identifies whether status asthmaticus or At the beginning of chapter 10 for “Diseases of exacerbation is present. the Respiratory System (J00-J99),” an instructional note states, “When a respiratory condition is Asthma ICD-10-CM description described as occurring in more than one site and Category J45 Asthma is not specifically indexed, it should be classified Includes: to the lower anatomic site.” For example, Allergic: tracheobronchitis is classified to bronchitis with Asthma code J40. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS. -

Severe Asthma Is Associated with a Remodeling of the Pulmonary Arteries in Horses
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.15.042903; this version posted April 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Severe asthma is associated with a remodeling of the pulmonary arteries in horses Remodeling of pulmonary arteries in severe equine asthma Serena Ceriotti1,2, Michela Bullone1, Mathilde Leclere1, Francesco Ferrucci2, Jean-Pierre Lavoie1* 1 Department of Clinical Sciences, Faculty of Veterinary Medicine, University of Montreal, Saint- Hyacinthe, Quebec, Canada 2 Department of Health, Animal Science and Food Safety, Università degli Studi di Milano, Milano, Italy Dr. Ceriotti current address is Department of Clinical Sciences, College of Veterinary Medicine, Auburn University, Auburn, Alabama, USA Dr. Bullone current address is Department of Veterinary Science, Università degli Studi di Torino, Grugliasco, Italy *Corresponding author: [email protected] Serena Ceriotti and Jean-Pierre Lavoie conceived and designed the work. Serena Ceriotti, Michela Bullone and Mathilde Leclere acquired clinical data, collected, processed and prepared histological and immunostained samples. Serena Ceriotti performed histomorphometric studies and statistical analysis. Serena Ceriotti, Jean-Pierre Lavoie and Francesco Ferrucci prepared and edited the manuscript prior to submission. Michela Bullone and Mathilde Leclere edited the manuscript prior to submission. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.04.15.042903; this version posted April 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Allergic Bronchopulmonary Aspergillosis: Diagnostic and Treatment Challenges
y & Re ar sp Leonardi et al., J Pulm Respir Med 2016, 6:4 on ir m a l to u r P y DOI: 10.4172/2161-105X.1000361 f M o e Journal of l d a i n c r i n u e o J ISSN: 2161-105X Pulmonary & Respiratory Medicine Review Article Open Access Allergic Bronchopulmonary Aspergillosis: Diagnostic and Treatment Challenges Lucia Leonardi*, Bianca Laura Cinicola, Rossella Laitano and Marzia Duse Department of Pediatrics and Child Neuropsychiatry, Division of Allergy and Clinical Immunology, Sapienza University of Rome, Policlinico Umberto I, Rome, Italy Abstract Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disorder, occurring mostly in asthmatic and cystic fibrosis patients, caused by an abnormal T-helper 2 lymphocyte response of the host to Aspergillus fumigatus antigens. ABPA diagnosis is defined by clinical, laboratory and radiological criteria including active asthma, immediate skin reactivity to A. fumigatus antigens, total serum IgE levels>1000 IU/mL, fleeting pulmonary parenchymal opacities and central bronchiectases that represent an irreversible complication of ABPA. Despite advances in our understanding of the role of the allergic response in the pathophysiology of ABPA, pathogenesis of the disease is still not completely clear. In addition, the absence of consensus regarding its prevalence, diagnostic criteria and staging limits the possibility of diagnosing the disease at early stages. This may delay the administration of a therapy that can potentially prevent permanent lung damage. Long-term management is still poorly studied. Present primary therapies, based on clinical experience, are not yet standardized. These consist in oral corticosteroids, which control acute symptoms by mitigating the allergic inflammatory response, azoles and, more recently, anti-IgE antibodies. -
So You Have Asthma
So You Have Asthma A GUIDE FOR PATIENTS AND THEIR FAMILIES So You Have Asthma A GUIDE FOR PATIENTS AND THEIR FAMILIES NIH Publication No. 13-5248 Originally Printed 2007 Revised March 2013 Contents Overview ...........................................................................................................................................................1 Introduction ....................................................................................................................................................3 Asthma—Some Basics ................................................................................................................................4 Why You? .........................................................................................................................................................6 How Does Asthma Make You Feel? ......................................................................................................8 How Do You Know if You Have Asthma? ...........................................................................................9 How To Control Your Asthma ................................................................................................................ 11 Your Asthma Management Partnership ................................................................................... 11 Your Written Asthma Action Plan ............................................................................................. 12 Your Asthma Medicines: How They Work and How To Take Them .......................... -

Pulmonary Hypertension ______
Pulmonary Hypertension _________________________________________ What is it? High blood pressure in the arteries that supply the lungs is called pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH). The blood pressure measured by a cuff on your arm isn’t directly related to the pressure in your lungs. The blood vessels that supply the lungs constrict and their walls thicken, so they can’t carry as much blood. As in a kinked garden hose, pressure builds up and backs up. The heart works harder, trying to force the blood through. If the pressure is high enough, eventually the heart can’t keep up, and less blood can circulate through the lungs to pick up oxygen. Patients then become tired, dizzy and short of breath. If a pre-existing disease triggered the PH, doctors call it secondary pulmonary hypertension. That’s because it’s secondary to another problem, such as a left heart or lung disorder. However, congenital heart disease can cause PH that’s similar to PH when the cause isn’t known, i.e., idiopathic or unexplained pulmonary arterial hypertension. In this case, the PAH is considered pulmonary arterial hypertension associated with congenital heart disease, such as associated with a VSD or ASD (either repaired or unrepaired). The problem is due to scarring in the small arteries in the lung. It’s important to repair congenital heart problems (when possible) before permanent pulmonary hypertensive changes develop. Intracardiac left-to-right shunts (such as a ventricular or atrial septal defect, a hole in the wall between the two ventricles or atria) can cause too much blood flow through the lungs. -

2020 GINA Pocket Guide for Asthma Management and Prevention
POCKET GUIDE FOR ASTHMA MANAGEMENT AND PREVENTION (for Adults and Children Older than 5 Years) DISTRIBUTE OR COPY NOT DO MATERIAL- COPYRIGHTED A Pocket Guide for Health Professionals Updated 2020 BASED ON THE GLOBAL STRATEGY FOR ASTHMA MANAGEMENT AND PREVENTION © 2020 Global Initiative for Asthma GLOBAL INITIATIVE FOR ASTHMA ASTHMA MANAGEMENT AND PREVENTION DISTRIBUTE for adults and children older ORthan 5 years COPY NOT A POCKET GUIDE FOR HEALTHDO PROFESSIONALS MATERIAL-Updated 2020 GINA Science Committee Chair: Helen Reddel, MBBS PhD COPYRIGHTED GINA Board of Directors Chair: Louis-Philippe Boulet, MD GINA Dissemination and Implementation Committee Chair: Mark Levy, MD (to Sept 2019); Alvaro Cruz, MD (from Sept 2019) GINA Assembly The GINA Assembly includes members from many countries, listed on the GINA website www.ginasthma.org. GINA Executive Director Rebecca Decker, BS, MSJ Names of members of the GINA Committees are listed on page 48. 1 LIST OF ABBREVIATIONS BDP Beclometasone dipropionate COPD Chronic obstructive pulmonary disease CXR Chest X-ray DPI Dry powder inhaler FeNO Fraction of exhaled nitric oxide FEV1 Forced expiratory volume in 1 second FVC Forced vital capacity GERD Gastroesophageal reflux disease HDM House dust mite ICS Inhaled corticosteroids ICS-LABA Combination ICS and LABA Ig Immunoglobulin IL Interleukin DISTRIBUTE IV Intravenous OR LABA Long-acting beta2-agonist COPY LAMA Long-acting muscarinic antagonist NOT LTRA Leukotriene receptor antagonistDO n.a. Not applicable NSAID Nonsteroidal anti-inflammatory drug MATERIAL- O2 Oxygen OCS Oral corticosteroids PEF Peak expiratory flow pMDI PressurizedCOPYRIGHTED metered dose inhaler SABA Short-acting beta2-agonist SC Subcutaneous SLIT Sublingual immunotherapy 2 TABLE OF CONTENTS List of abbreviations ........................................................................................ -

Asthma and COVID-19: Scientific Brief
Asthma and COVID-19 Scientific brief 19 April 2021 Background People with asthma (PWA) generally are considered at higher risk from respiratory infections, as is seen annually with influenza. At the outset of the COVID-19 pandemic, PWA were widely assumed to be at increased risk from COVID-19. However, as data emerged throughout 2020, the association between asthma and COVID-19 appeared less clear (1). A rapid systematic review was undertaken to inform this scientific brief. The review set out to assess the available peer-reviewed literature regarding whether PWA are at increased risk of infection with the virus that causes COVID-19, and/or of experiencing complications or death. In particular, the review set out to analyse evidence on the following questions. • Is asthma associated with increased risk of acquiring SARS-CoV-2 and COVID-19 disease? • Is asthma associated with hospitalization with COVID-19? • Is asthma associated with the severity of COVID-19 outcomes? Methods A protocol for the rapid review was documented in advance of evidence retrieval and data analysis. Searches included the Cochrane COVID-19 study register, Embase, MEDLINE and LitCOVID on 8 October 2020 for published literature or literature accepted for publication but not yet published, in any language. Two reviewers screened titles and abstracts, and full texts of selected references, according to the following inclusion criteria: • population: people diagnosed with asthma, with no limitations by age, disease severity or duration • exposure: SARS-CoV-2 infection • comparator: people without asthma • outcome: rates of SARS-CoV-2 infection and COVID-19 disease: confirmed/suspected infection; hospitalization; admission to intensive care unit (ICU); death.