Antibiotic Guidelines 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prevalence of Self-Medication of Antibiotics Among People In
International Journal of Pharmacy Teaching & Practices 2013, Vol.4, Issue 1, 504-510. Prevalence of self-medication of antibiotics among people in Bangladesh Nishat Chowdhury*, Mohammad Rashedul Islam, Md. Mehedi Hasan, Md. Mahmudur Rouf *Department of Pharmacy, State University of Bangladesh, Dhanmondi, Dhaka, Bangladesh Introduction Research Article Widespread and inappropriate use of antibiotics increases health care costs (1) and contributes to Please cite this paper as: Nishat Chowdhury*, Mohammad Rashedul Islam, Md. Mehedi Hasan, Md. Mahmudur Rouf. Prevalence of self- antibiotic resistance (2)。 Antimicrobial medication medication of antibiotics among people in Bangladesh . IJPTP, 2013, management in Bangladesh has been highlighted by 4(1), 504-510. previous studies as an area for improvement (3). Corresponding Author: There is already enough evidence of growing resistance to antimicrobials in this country resulting Nishat Chowdhury, from misuse (4-6). Previous study showed that Department of Pharmacy, State University of Bangladesh, antimicrobials are widely available (18% incidents) in Dhanmondi, Dhaka, Bangladesh the home medicine cabinets of the Dhaka City Telephone -88028612992, population (7). Since there is no prescription-only Email: [email protected] drug in Bangladesh, people can purchase drugs like sedatives, antimicrobials without prescription even in the remote parts of the country (8-9). The relative Abstract lack of data on the morbidity and mortality attributable to antibiotic resistance, including the This study attempts to investigate the prevalence of self- economic impact on individuals as well as on health medication of antibiotics among people in Bangladesh.This care and societies, may explain the weak reaction study was conducted in six districts of Bangladesh (Dhaka, from politicians, public health workers, and Munshiganj, Kishoreganj, Chittagong, Chandpur, Kushtia) by consumers to this threat to public health (10). -

The Activity of Mecillinam Vs Enterobacteriaceae Resistant to 3Rd Generation Cephalosporins in Bristol, UK
The activity of mecillinam vs Enterobacteriaceae resistant to 3rd generation cephalosporins in Bristol, UK Welsh Antimicrobial Study Group Grŵp Astudio Wrthfiotegau Cymru G Weston1, KE Bowker1, A Noel1, AP MacGowan1, M Wootton2, TR Walsh2, RA Howe2 (1) BCARE, North Bristol NHS Trust, Bristol BS10 5NB (2) Welsh Antimicrobial Study Group, NPHS Wales, University Hospital of Wales, CF14 4XW Introduction Results Results Results Figure 1: Population Distributions of Mecillinam MICs for E. Figure 2: Population Distributions of MICs for ESBL- Resistance in coliforms to 3rd generation 127 isolates were identified by screening of which 123 were confirmed as resistant to CTX or coli (n=72), NON-E. coli Enterobacteriaceae (n=47) and multi- producing E. coli (n=67) against mecillinam or mecillinam + cephalosporins (3GC) is an increasing problem resistant strains (n=39) clavulanate CAZ by BSAC criteria. The majority of 3GC- both in hospitals and the community. Oral options MR Non-E. coli E. coli Mecalone Mec+Clav resistant strains were E. coli 60.2%, followed by for the treatment of these organisms is often 35 50 Enterobacter spp. 16.2%, Klebsiella spp. 12.2%, limited due to resistance to multiple antimicrobial 45 and others (Citrobacter spp., Morganella spp., 30 classes. Mecillinam, an amidinopenicillin that is 40 Pantoea spp., Serratia spp.) 11.4%. 25 available in Europe as the oral pro-drug 35 All isolates were susceptible to meropenem with s 20 30 e s pivmecillinam, is stable to many beta-lactamases. t e a t l a mecillinam the next most active agent with more l o 25 o s We aimed to establish the activity of mecillinam i s i 15 % than 95% of isolates susceptible (table). -

Antibiotic Use Guidelines for Companion Animal Practice (2Nd Edition) Iii
ii Antibiotic Use Guidelines for Companion Animal Practice (2nd edition) iii Antibiotic Use Guidelines for Companion Animal Practice, 2nd edition Publisher: Companion Animal Group, Danish Veterinary Association, Peter Bangs Vej 30, 2000 Frederiksberg Authors of the guidelines: Lisbeth Rem Jessen (University of Copenhagen) Peter Damborg (University of Copenhagen) Anette Spohr (Evidensia Faxe Animal Hospital) Sandra Goericke-Pesch (University of Veterinary Medicine, Hannover) Rebecca Langhorn (University of Copenhagen) Geoffrey Houser (University of Copenhagen) Jakob Willesen (University of Copenhagen) Mette Schjærff (University of Copenhagen) Thomas Eriksen (University of Copenhagen) Tina Møller Sørensen (University of Copenhagen) Vibeke Frøkjær Jensen (DTU-VET) Flemming Obling (Greve) Luca Guardabassi (University of Copenhagen) Reproduction of extracts from these guidelines is only permitted in accordance with the agreement between the Ministry of Education and Copy-Dan. Danish copyright law restricts all other use without written permission of the publisher. Exception is granted for short excerpts for review purposes. iv Foreword The first edition of the Antibiotic Use Guidelines for Companion Animal Practice was published in autumn of 2012. The aim of the guidelines was to prevent increased antibiotic resistance. A questionnaire circulated to Danish veterinarians in 2015 (Jessen et al., DVT 10, 2016) indicated that the guidelines were well received, and particularly that active users had followed the recommendations. Despite a positive reception and the results of this survey, the actual quantity of antibiotics used is probably a better indicator of the effect of the first guidelines. Chapter two of these updated guidelines therefore details the pattern of developments in antibiotic use, as reported in DANMAP 2016 (www.danmap.org). -

Guidelines on Urinary and Male Genital Tract Infections
European Association of Urology GUIDELINES ON URINARY AND MALE GENITAL TRACT INFECTIONS K.G. Naber, B. Bergman, M.C. Bishop, T.E. Bjerklund Johansen, H. Botto, B. Lobel, F. Jimenez Cruz, F.P. Selvaggi TABLE OF CONTENTS PAGE 1. INTRODUCTION 5 1.1 Classification 5 1.2 References 6 2. UNCOMPLICATED UTIS IN ADULTS 7 2.1 Summary 7 2.2 Background 8 2.3 Definition 8 2.4 Aetiological spectrum 9 2.5 Acute uncomplicated cystitis in pre-menopausal, non-pregnant women 9 2.5.1 Diagnosis 9 2.5.2 Treatment 10 2.5.3 Post-treatment follow-up 11 2.6 Acute uncomplicated pyelonephritis in pre-menopausal, non-pregnant women 11 2.6.1 Diagnosis 11 2.6.2 Treatment 12 2.6.3 Post-treatment follow-up 12 2.7 Recurrent (uncomplicated) UTIs in women 13 2.7.1 Background 13 2.7.2 Prophylactic antimicrobial regimens 13 2.7.3 Alternative prophylactic methods 14 2.8 UTIs in pregnancy 14 2.8.1 Epidemiology 14 2.8.2 Asymptomatic bacteriuria 15 2.8.3 Acute cystitis during pregnancy 15 2.8.4 Acute pyelonephritis during pregnancy 15 2.9 UTIs in post-menopausal women 15 2.10 Acute uncomplicated UTIs in young men 16 2.10.1 Pathogenesis and risk factors 16 2.10.2 Diagnosis 16 2.10.3 Treatment 16 2.11 References 16 3. UTIs IN CHILDREN 20 3.1 Summary 20 3.2 Background 20 3.3 Aetiology 20 3.4 Pathogenesis 20 3.5 Signs and symptoms 21 3.5.1 New-borns 21 3.5.2 Children < 6 months of age 21 3.5.3 Pre-school children (2-6 years of age) 21 3.5.4 School-children and adolescents 21 3.5.5 Severity of a UTI 21 3.5.6 Severe UTIs 21 3.5.7 Simple UTIs 21 3.5.8 Epididymo orchitis 22 3.6 Diagnosis 22 3.6.1 Physical examination 22 3.6.2 Laboratory tests 22 3.6.3 Imaging of the urinary tract 23 3.7 Schedule of investigation 24 3.8 Treatment 24 3.8.1 Severe UTIs 25 3.8.2 Simple UTIs 25 3.9 References 26 4. -

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -

WO 2010/025328 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 4 March 2010 (04.03.2010) WO 2010/025328 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (21) International Application Number: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, PCT/US2009/055306 DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 28 August 2009 (28.08.2009) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (26) Publication Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/092,497 28 August 2008 (28.08.2008) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): FOR¬ GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, EST LABORATORIES HOLDINGS LIMITED [IE/ ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, —]; 18 Parliament Street, Milner House, Hamilton, TM), European (AT, BE, BG, CH, CY, CZ, DE, DK, EE, Bermuda HM12 (BM). -

WHO Report on Surveillance of Antibiotic Consumption: 2016-2018 Early Implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some Rights Reserved
WHO Report on Surveillance of Antibiotic Consumption 2016-2018 Early implementation WHO Report on Surveillance of Antibiotic Consumption 2016 - 2018 Early implementation WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons. org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non- commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

2012 Harmonized Tariff Schedule Pharmaceuticals Appendix
Harmonized Tariff Schedule of the United States (2014) (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2014) (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACEVALTRATE 25161-41-5 ABAFUNGIN 129639-79-8 ACEXAMIC ACID 57-08-9 ABAGOVOMAB 792921-10-9 ACICLOVIR 59277-89-3 ABAMECTIN 65195-55-3 ACIFRAN 72420-38-3 ABANOQUIL 90402-40-7 ACIPIMOX 51037-30-0 ABAPERIDONE 183849-43-6 ACITAZANOLAST 114607-46-4 ABARELIX 183552-38-7 ACITEMATE 101197-99-3 ABATACEPT 332348-12-6 ACITRETIN 55079-83-9 ABCIXIMAB 143653-53-6 ACIVICIN 42228-92-2 ABECARNIL 111841-85-1 ACLANTATE 39633-62-0 ABETIMUS 167362-48-3 ACLARUBICIN 57576-44-0 ABIRATERONE 154229-19-3 ACLATONIUM NAPADISILATE 55077-30-0 ABITESARTAN 137882-98-5 ACLIDINIUM BROMIDE 320345-99-1 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURIN 178535-93-8 ACOLBIFENE 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDE 185106-16-5 -

Early Childhood Antibiotic Treatment for Otitis Media and Other Respiratory Tract Infections Is Associated with Risk of Type
Diabetes Care Volume 43, May 2020 991 Mona-Lisa Wernroth,1,2 Katja Fall,3,4 Early Childhood Antibiotic Bodil Svennblad,5 Jonas F. Ludvigsson,4,6 Arvid Sjolander,¨ 4 Catarina Almqvist,4,7 and Treatment for Otitis Media and Tove Fall1 Other Respiratory Tract Infections Is Associated With Risk of Type 1 Diabetes: A Nationwide Register- Based Study With Sibling Analysis EPIDEMIOLOGY/HEALTH SERVICES RESEARCH Diabetes Care 2020;43:991–999 | https://doi.org/10.2337/dc19-1162 OBJECTIVE The effect of early-life antibiotic treatment on the risk of type 1 diabetes is debated. This study assessed this question, applying a register-based design in children up to age 10 years including a large sibling-control analysis. RESEARCH DESIGN AND METHODS All singleton children (n 5 797,318) born in Sweden between 1 July 2005 and 1 30 September 2013 were included and monitored to 31 December 2014. Cox Molecular Epidemiology, Department of Med- ical Sciences, and Science for Life Laboratory, proportional hazards models, adjusted for parental and perinatal characteristics, Uppsala University, Uppsala, Sweden were applied, and stratified models were used to account for unmeasured con- 2Uppsala Clinical Research Center, Uppsala Uni- founders shared by siblings. versity, Uppsala, Sweden 3Clinical Epidemiology and Biostatistics, School RESULTS of Medical Sciences, Orebro¨ University, Orebro,¨ Sweden Type 1 diabetes developed in 1,297 children during the follow-up (median 4.0 years 4Department of Medical Epidemiology and Bio- [range 0–8.3]). Prescribed antibiotics in the 1st year of life (23.8%) were associated statistics, Karolinska Institutet, Stockholm, Sweden with anincreased risk oftype1diabetes(adjustedhazard ratio[HR]1.19[95%CI1.05– 5Department of Surgical Sciences, Uppsala Uni- versity, Uppsala, Sweden 1.36]), with larger effect estimates among children delivered by cesarean section 6 ¨ P 5 Department of Pediatrics, Orebro University ( for interaction 0.016). -
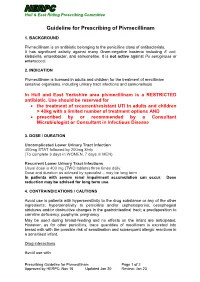
Guideline for Prescribing of Pivmecillinam
Hull & East Riding Prescribing Committee Guideline for Prescribing of Pivmecillinam 1. BACKGROUND Pivmecillinam is an antibiotic belonging to the penicillins class of antibacterials. It has significant activity against many Gram-negative bacteria including E coli, klebsiella, enterobacter, and salmonellae. It is not active against Ps aeruginosa or enterococci. 2. INDICATION Pivmecillinam is licensed in adults and children for the treatment of mecillinam sensitive organisms, including urinary tract infections and salmonellosis In Hull and East Yorkshire area pivmecillinam is a RESTRICTED antibiotic. Use should be reserved for the treatment of recurrent/resistant UTI in adults and children > 40kg with a limited number of treatment options AND prescribed by or recommended by a Consultant Microbiologist or Consultant in Infectious Disease 3. DOSE / DURATION Uncomplicated Lower Urinary Tract Infection 400mg STAT followed by 200mg 8hrly (To complete 3 days in WOMEN, 7 days in MEN) Recurrent Lower Urinary Tract Infections Usual dose is 400 mg (TWO tablets) three times daily. Dose and duration as advised by specialist – may be long term In patients with severe renal impairment accumulation can occur. Dose reduction may be advised for long term use. 4. CONTRAINDICATIONS / CAUTIONS Avoid use is patients with hypersensitivity to the drug substance or any of the other ingredients; hypersensitivity to penicillins and/or cephalosporins; oesophageal strictures and/or obstructive changes in the gastrointestinal tract; a predisposition to carnitine deficiency; porphyria; pregnancy. May be used during breast-feeding and no effects on the infant are anticipated. However, as for other penicillins, trace quantities of mecillinam is excreted into breast milk with the possible risk of sensitisation and subsequent allergic reactions in a sensitised infant. -

Cefotaxime: Rate of Bacterial Killing and Interactions with Serum and Leukocyte Activity
ACTA M~DICA PORTUGUESA 1983; 4: 167-171 ORIGINAL CEFOTAXIME: RATE OF BACTERIAL KILLING AND INTERACTIONS WITH SERUM AND LEUKOCYTE ACTIVITY GIULIANA GIALDRONI GRASSI, PATRIZIA MANGIAROTTI, ANNA FIETTA Chair of Chemotherapy. Istituto Forlanini. University of Pavia. Italy SUMMARY Cefotaxime (HR 756) was compared with cefazolin and cephaloridine with regard to the rate of bacterial killing and to the influence on the bactericidal activity of human serum and polyrnorphonuclear leukocytes. At concentrations equal to 1-2 x MIC cefotaxime showed a more rapid and complete bactericidal activity on E. coil K 12 than cephaloridine and cefazolin. In presence of the latters in fact, bacterial regrowth was observed after 24 hours. On S. aureus a complete killing activity of cefotaxime appeared at concentrations of 8 x MIC. A synergism seemed to exist between the complement dependent bactericidal activity of normal human serum and cephalosporins. E. coil K 12 (a rough strain) was killed by the combi nation of human serum and both cefotaxime and cefazolin at concentrations that were not bactericidal by themselves. Cephaloridine on the contrary showed an additive activity with normal human serum. Finally evidence that cefotaxime enhanced the bactericidal activity of human polymorphonuclear leukocytes against S. faecaiis, is reported. RESUMO Cefotaxirna: Poder Bactericida e Interaccao corn a Actividade Leucocitãria e do Soro. Cornparou-se o poder bactericida e a interferência da cefotaxima (HR 756) na actividade bactericida dos leucocitos polimorfonucleares e do soro corn os parametros equivalentes referentes a cefazolina e a cefaloridina. A concentracOes equivalentes a 1-2 vezes a concentracao Inibitória Minima (CIM) a cefotaxima revelou uma accAo bactericida mais rápida e completa sobre o E. -

Mechanisms and Dynamics of Mecillinam Resistance in Escherichia Coli
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1375 Mechanisms and Dynamics of Mecillinam Resistance in Escherichia coli ELISABETH THULIN ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-513-0090-0 UPPSALA urn:nbn:se:uu:diva-330856 2017 Dissertation presented at Uppsala University to be publicly examined in A1:111a, BMC, Husargatan 3, Uppsala, Friday, 24 November 2017 at 09:00 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in English. Faculty examiner: Professor Laura Piddock ( Institute of Microbiology and Infection, University of Birmingham, UK). Abstract Thulin, E. 2017. Mechanisms and Dynamics of Mecillinam Resistance in Escherichia coli. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1375. 69 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-513-0090-0. The introduction of antibiotics in healthcare is one of the most important medical achievements with regard to reducing human morbidity and mortality. However, bacterial pathogens have acquired antibiotic resistance at an increasing rate, and due to a high prevalence of resistance to some antibiotics they can no longer be used therapeutically. The antibiotic mecillinam, which inhibits the penicillin-binding protein PBP2, however, is an exception since mecillinam resistance (MecR) prevalence has remained low. This is particularly interesting since laboratory experiments have shown that bacteria can rapidly acquire MecR mutations by a multitude of different types of mutations. In this thesis, I examined mechanisms and dynamics of mecillinam resistance in clinical and laboratory isolates of Escherichia coli. Only one type of MecR mutations (cysB) was found in the clinical strains, even though laboratory experiments demonstrate that more than 100 genes can confer resistance Fitness assays showed that cysB mutants have higher fitness than most other MecR mutants, which is likely to contribute to their dominance in clinical settings.