The Use of Activated Charcoal in Pediatric Populations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
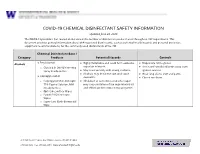
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Activated Charcoal for Acute Poisoning: One Toxicologist's Journey
J. Med. Toxicol. (2010) 6:190–198 DOI 10.1007/s13181-010-0046-1 REVIEW ARTICLE Activated Charcoal for Acute Poisoning: One Toxicologist’s Journey Kent R. Olson Published online: 20 May 2010 # The Author(s) 2010. This article is published with open access at Springerlink.com Keywords Activated charcoal . Gastrointestinal As summarized by Matthew [13], Harstad and Danish decontamination . Poisoning . Drug overdose colleagues reported in 1942 that relatively little phenobar- bital was recovered by lavage even shortly after overdose [14] and this, along with their finding of particles of When I began studying clinical toxicology in 1981, the issue charcoal in the lungs of patients who died, led them to call of gastrointestinal decontamination after acute ingestion for the abandonment of gastric lavage for poisoning.) “ ” seemed pretty well settled: universal antidote, apomor- In recent years, my colleagues and I have continued to – phine and salt wateremesiswerenolongerused[1, 2]; and I debate the value of various methods of gastric decontam- was taught that barring a specific contraindication, the awake ination and the role and risks of activated charcoal, and it is patient was given syrup of ipecac to induce emesis, and the clear to me that the issue remains muddy. Some have taken drowsy or uncooperative patient was lavaged [3]. After a firm stand that no treatment should be recommended that is gastric emptying, everyone received activated charcoal not supported by evidence from a randomized controlled trial (AC). The only controversy seemed to be over whether one (RCT). Position statements published jointly by the Amer- should add a cathartic to speed gastrointestinal transit [4]. -

Magnesium Sulfate
MAGNESIUM SULFATE Prepared at the 68th JECFA (2007), published in FAO JECFA Monographs 4 (2007), superseding the specifications prepared at the 63rd JECFA (2004) and published the Combined Compendium of Food Additive Specifications, FAO JECFA Monographs 1 (2005). An ADI “not specified” was established at the 68th JECFA (2007). SYNONYMS Epsom salt (heptahydrate); INS No.518 DEFINITION Magnesium sulfate occurs naturally in sea water, mineral springs and in minerals such as kieserite and epsomite. It is recovered from them or by reacting sulfuric acid and magnesium oxide. It is produced with one or seven molecules of water of hydration or in a dried form containing the equivalent of between 2 and 3 waters of hydration. Chemical names Magnesium sulfate C.A.S. number Monohydrate: 14168-73-1 Heptahydrate: 10034-99-8 Dried: 15244-36-7 Chemical formula Monohydrate: MgSO4.H2O Heptahydrate: MgSO4.7H2O Dried: MgSO4.xH2O, where x is the average hydration value (between 2 and 3) Formula weight Monohydrate: 138.38 Heptahydrate: 246.47 Assay Not less than 99.0 % and not more than 100.5% on the ignited basis DESCRIPTION Colourless crystals, granular crystalline powder or white powder. Crystals effloresce in warm, dry air. FUNCTIONAL USES Nutrient; flavour enhancer; firming agent; and processing aid (fermentation aid in the production of beer and malt beverages) CHARACTERISTICS IDENTIFICATION Solubility (Vol. 4) Freely soluble in water, very soluble in boiling water, and sparingly soluble in ethanol. Test for magnesium (Vol. 4) Passes test Test for sulfate (Vol. 4) Passes test PURITY Loss on ignition (Vol. 4) Monohydrate: between 13.0 and 16.0 %, Heptahydrate: between 40.0 and 52.0 %, Dried: between 22.0 and 32.0 % (105°, 2h, then 400° to constant weight) pH (Vol. -

Mechanosynthesis of Magnesium and Calcium Salt?Urea Ionic Cocrystal
Letter pubs.acs.org/journal/ascecg Mechanosynthesis of Magnesium and Calcium Salt−Urea Ionic Cocrystal Fertilizer Materials for Improved Nitrogen Management Kenneth Honer, Eren Kalfaoglu, Carlos Pico, Jane McCann, and Jonas Baltrusaitis* Department of Chemical and Biomolecular Engineering, Lehigh University, B336 Iacocca Hall, 111 Research Drive, Bethlehem, Pennsylvania 18015, United States *S Supporting Information ABSTRACT: Only 47% of the total fertilizer nitrogen applied to the environment is taken up by the plants whereas approximately 40% of the total fertilizer nitrogen lost to the environment reverts back into unreactive atmospheric dinitrogen that greatly affects the global nitrogen cycle including increased energy consumption for NH3 synthesis, as well as accumulation of nitrates in drinking water. In this letter, we provide a mechanochemical method of inorganic magnesium and calcium salt−urea ionic cocrystal synthesis to obtain enhanced stability nitrogen fertilizers. The solvent-free mechanochemical synthesis presented can result in a greater manufacturing process sustainability by reducing or eliminating the need for solution handling and evaporation. NH3 emission testing suggests that urea ionic cocrystals are capable of decreasing NH3 emissions to the environment when compared to pure urea, thus providing implications for a sustainable global solution to the management of the nitrogen cycle. KEYWORDS: Fertilizers, Nitrogen, urea, Mechanochemistry, Cocrystal, pXRD, NH3 Emissions, Stability ■ INTRODUCTION ammonia as opposed to up to 61.1% of soil treated with urea 7,8 fi only, which suggests that major improvements to the global Atmospheric dinitrogen, N2, xation to synthesize ammonia, 9,10 ’ 1 nitrogen cycle are achievable. Additionally, urea molecular NH3, consumes more than 1% of the world s primary energy. -
The Importance of Minerals in the Long Term Health of Humans Philip H
The Importance of Minerals in the Long Term Health of Humans Philip H. Merrell, PhD Technical Market Manager, Jost Chemical Co. Calcium 20 Ca 40.078 Copper 29 Cu 63.546 Iron Magnesium 26 12 Fe Mg 55.845 24.305 Manganese Zinc 25 30 Mn Zn 55.938 65.380 Table of Contents Introduction, Discussion and General Information ..................................1 Calcium ......................................................................................................3 Copper .......................................................................................................7 Iron ...........................................................................................................10 Magnesium ..............................................................................................13 Manganese ..............................................................................................16 Zinc ..........................................................................................................19 Introduction Daily intakes of several minerals are necessary for the continued basic functioning of the human body. The minerals, Calcium (Ca), Iron (Fe), Copper (Cu), Magnesium (Mg), Manganese (Mn), and Zinc (Zn) are known to be necessary for proper function and growth of the many systems in the human body and thus contribute to the overall health of the individual. There are several other trace minerals requirements. Minimum (and in some cases maximum) daily amounts for each of these minerals have been established by the Institute of -

Treatment of Self-Poisoned Adults G
Archives of Emergency Medicine, 1985, 2, 203-208 Ipecacuanha induced emesis in the treatment of self-poisoned adults G. GORDON Accident and Emergency Department, Manor Hospital, Nuneaton, Warwickshire, England SUMMARY One hundred consecutive adult patients presenting to an Accident and Emergency Department following intentional self-poisoning were given 50 to 80 ml Paediatric Ipecacuanha Emetic Mixture BP as an emetic, together with two or three glasses of strong orange juice. A satisfactory emetic result was obtained in 99 patients. No toxic effects were noted in these patients, or in the one patient in whom emesis did not occur, and who subsequently refused gastric lavage. The potential toxicity of Ipecacuanha Syrup itself is discussed, and attention drawn to the lower Emetine content of Paediatric Ipecacuanha Emetic Mixture (BP), rather than that of the formulations used in previously published reports. The use of Paediatric Ipecacuanha Emetic Mixture B.P. in adults is effective and safe in this dosage. INTRODUCTION The methods available for retrieval of poisoning agents from the stomach are gastric lavage and emesis. In the United Kingdom at the present time, gastric lavage is the method most commonly used in the treatment of adults. It is an unpleasant and time consuming procedure for both patient and staff, and it is not without risk (Matthew et al., 1966), even in the hands of the experienced nursing staff who usually carry it out. Doubt still remains about its effectiveness (Goulding & Volans, 1977), and the basis for its use rests more on the occasional recovery of large quantities of drug, rather than verification of its routine efficiency by studies in man (Melman & Morelli, 1978). -

Sulfate Resistance Study of Carbonated Low-Calcium Silicate Systems
Sixth International Conference on Durability of Concrete Structures Paper Number PSE12 18 - 20 July 2018 University of Leeds, Leeds, West Yorkshire, LS2 9JT, United Kingdom Sulfate Resistance Study of Carbonated Low-Calcium Silicate Systems R. Tokpatayeva and J. Olek Lyles School of Civil Engineering, Purdue University, West Lafayette, IN, USA J. Jain, A. Seth and N. DeCristofaro Solidia Technologies Inc., Piscataway, NJ, USA ABSTRACT This paper summarizes the results of sulfate resistance study of carbonated mortar specimens made with Solidia Cement (SC) and tested for expansion according to ASTM C1012 specification while exposed to three types of soak solutions: sodium sulfate, magnesium sulfate and deionized water. A control set of ordinary portland cement (OPC) mortars was also evaluated. Besides the length change measurements, visual observations of changes in the appearance of specimens were conducted after various lengths of exposure. In addition, microstructural characterization of the specimens was conducted using scanning electron microscopy (SEM), X-ray diffraction (XRD) and thermo-gravimetric analysis (TGA) techniques. Finally, changes in the concentration of the chemical species present in the soak solutions in contact with the SC specimens were evaluated using both, the ion chromatography (IC) and the inductively coupled plasma optical emission spectrometry (ICP-OES). As expected, the OPC mortar specimens started deteriorating early and reached the critical (i.e.0.1%) level of expansion in about 4 months in case of sodium sulfate solution and in about 6 months in case of magnesium sulfate solution. With respect to the SC mortar specimens, those exposed to magnesium sulfate solution showed higher expansion than those exposed to sodium sulfate solution. -

Managing Ferret Toxicoses J
CLINICIAN’S NOTEBOOK Managing Ferret Toxicoses J. RICHARDSON AND R. BALABUSZKO Jill A. Richardson, DVM, Dipl ACFE ASPCA National Animal Poison Control Center 1717 South Philo Road Suite 36 Urbana, Illinois 61802 [email protected] FERRETS ARE EXTREMELY CURIOUS and adept at accessing areas where PRACTICE TIP baits, cleaners, chemicals and medica- Rachel A. Balabuszko, CVT tions are stored. Ferrets can even pry ASPCA National Animal Poison caps from child-resistant bottles or Control Center chew through heavy plastic contain- ers. Products such as antifreeze, Dr. Jill A. Richardson received her DVM flavored medications or pest control degree from Tuskegee University in baits have an appealing taste. Because 1994. In 1996, following experience in the average weight of the adult ferret small animal practices in Tennessee and is less than 2 kg, even small amounts in West Virginia, Dr. Richardson joined of toxins can be dangerous when the ASPCA National Animal Poison ingested. Therefore, prompt treatment Control Center as a Veterinary Poison of toxicoses is essential. Information Specialist. Rachel Balabuszko, CVT, joined the In cases of oral exposure, ferrets have ASPCA National Animal Poison Control the ability to vomit. However, the Center as a Certified Veterinary length of time since ingestion of the Ferrets can be restrained by scruffing Technician in 1998, after receiving her toxicant, the ferret’s age, its previous the loose skin on the back of the neck. associate degree in veterinary technol- medical history, and the type of ogy from Parkland College. poison ingested all affect the decision to induce emesis. Tom Schaefges Photography Sidney, Illinois [email protected] EXOTIC DVM VOLUME 2.4 2000 23 CLINICIAN’S NOTEBOOK STEPS IN MANAGING FERRET TOXICOSES START ASSESS THE SITUATION STABILIZE THE FERRET ✖ Is the ferret seizuring? ✖ Administer oxygen if necessary ✖ Is the ferret breathing? ✖ Control seizures ✖ What is the heart rate? ✖ Correct any cardiovascular ✖ What color are the mucous abnormality membranes? Table 1. -

Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care
TOXICOLOGY/CONCEPTS Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care Richard C. Dart, MD, PhD From the Rocky Mountain Poison & Drug Center - Denver Health, Denver, CO (Dart, Heard, Schaeffer, Stephen W. Borron, MD, MS Bogdan, Alhelail, Buchanan, Hoppe, Lavonas, Mlynarchek, Phua, Rhyee, Varney, Zosel); Department of E. Martin Caravati, MD, MPH Surgery, University of Texas Health Sciences Center, San Antonio, TX (Borron); Division of Emergency Daniel J. Cobaugh, PharmD Medicine, Utah Poison Control Center, University of Utah Health Sciences Center, Salt Lake City, UT Steven C. Curry, MD (Caravati); ASHP Research and Education Foundation, Bethesda, MD (Cobaugh); Department of Jay L. Falk, MD Medical Toxicology and Banner Poison Control Center, Banner Good Samaritan Medical Center, Lewis Goldfrank, MD Phoenix, AZ (Curry); Department of Emergency Medicine, Orlando Regional Medical Center, University of Susan E. Gorman, PharmD, MS Florida, Orlando, FL (Falk); New York City Poison Center; New York University School of Medicine, New Stephen Groft, PharmD York, NY (Goldfrank); Division of Strategic National Stockpile, Centers for Disease Control and Kennon Heard, MD Prevention, Atlanta, GA (Gorman); Office of Rare Diseases Research, Bethesda, MD (Groft); Division of Ken Miller, MD, PhD Emergency Medicine, School of Medicine (Dart, Heard, Lavonas, Schaeffer) and Department of Kent R. Olson, MD Pharmaceutical Sciences, School of Pharmacy (Bogdan), University of Colorado Denver, Aurora, CO; Gerald O’Malley, DO Orange County Fire Authority and Orange County Health Care Agency Emergency Medical Services, Donna Seger, MD Irvine, CA, and National Association of EMS Physicians, Lenexa, KS, (Miller); University of California, Steven A. Seifert, MD San Francisco, and San Francisco Division, California Poison Control System, San Francisco, CA Marco L. -

Magnesium Sulfate for Neuroprotection Practice Guideline
[Type text] [Type text] Updated June 2013 Magnesium Sulfate for Neuroprotection Practice Guideline I. Background: Magnesium sulfate has been suggested to have neuro-protective effect in retrospective studies from 1987 and 1996. Since that time three randomized control trials have been performed to assess magnesium therapy for fetal neuroprotection. These studies have failed to demonstrate statistically significant decrease in combined outcome of cerebral palsy and death or improved overall neonatal survival. However, these results did demonstrate a significant decrease in cerebral palsy of any severity by 30%, particularly moderate-severe cerebral palsy (40-45%). The number needed to treat at less than 32 weeks gestation is 56. The presumptive mechanism of action for magnesium sulfate focuses on the N-methyl-D-aspartate receptor. Additional magnesium effects include calcium channel blockade resulting in cerebrovascular relaxation and magnesium mediated decreases in free radical production and reductions in the production of inflammatory cytokines. Magnesium sulfate should not be used as a tocolytic simply because of the potential for neuro-protective effects. In a recent committee opinion, ACOG states “the available evidence suggests that magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants” but specific guidelines should be established. “The U.S. FDA has recently changed the classification of magnesium sulfate injection from Category A to Category D. However, this change was based on a small number of neonatal outcomes in cases in which the average duration of exposure was 9.6 weeks. The ACOG Committee on Obstetric Practice and the Society for Maternal-Fetal Medicine continue to support the use of magnesium sulfate in obstetric care for appropriate conditions and for appropriate, short term (usually less than 48 hours) durations of treatment.” II. -

Reactions of Alcohols & Ethers 1
REACTIONS OF ALCOHOLS & ETHERS 1. Combustion (Extreme Oxidation) alcohol + oxygen carbon dioxide + water 2 CH3CH2OH + 6 O2 4 CO2 + 6 H2O 2. Elimination (Dehydration) ° alcohol H 2 S O 4/ 1 0 0 C alkene + water H2SO4/100 ° C CH3CH2CH2OH CH3CH=CH2 + H2O 3. Condensation ° excess alcohol H 2 S O 4 / 1 4 0 C ether + water H2SO4/140 ° C 2 CH3CH2OH CH3CH2OCH2CH3 + H2O 4. Substitution Lucas Reagent alcohol + hydrogen halide Z n C l2 alkyl halide + water ZnCl2 CH3CH2OH + HCl CH3CH2Cl + H2O • This reaction with the Lucas Reagent (ZnCl2) is a qualitative test for the different types of alcohols because the rate of the reaction differs greatly for a primary, secondary and tertiary alcohol. • The difference in rates is due to the solubility of the resulting alkyl halides • Tertiary Alcohol→ turns cloudy immediately (the alkyl halide is not soluble in water and precipitates out) • Secondary Alcohol → turns cloudy after 5 minutes • Primary Alcohol → takes much longer than 5 minutes to turn cloudy 5. Oxidation • Uses an oxidizing agent such as potassium permanganate (KMnO4) or potassium dichromate (K2Cr2O7). • This reaction can also be used as a qualitative test for the different types of alcohols because there is a distinct colour change. dichromate → chromium 3+ (orange) → (green) permanganate → manganese (IV) oxide (purple) → (brown) Tertiary Alcohol not oxidized under normal conditions CH3 KMnO4 H3C C OH NO REACTION K2Cr2O7 CH3 tertbutyl alcohol Secondary Alcohol ketone + hydrogen ions H O KMnO4 H3C C CH3 + K2Cr2O7 C + 2 H H3C CH3 OH propanone 2-propanol Primary Alcohol aldehyde + water carboxylic acid + hydrogen ions O KMnO4 O H H KMnO H H 4 + CH3CH2CH2OH C C C H C C C H + 2 H K2Cr2O7 + H2O K Cr O H H H 2 2 7 HO H H 1-propanol propanal propanoic acid 6. -

Poison/Drug Emergencies 1. Which Alcohol Is Used As an Antidote For
Student ID: 22195894 Exam: 084084RR - Poison/Drug Emergencies When you have completed your exam and reviewed your answers, click Submit Exam. Answers will not be recorded until you hit Submit Exam. If you need to exit before completing the exam, click Cancel Exam. Questions 1 to 20: Select the best answer to each question. Note that a question and its answers may be split across a page break, so be sure that you have seen the entire question and all the answers before choosing an answer. 1. Which alcohol is used as an antidote for ethylene glycol ingestions? A. Ethanol B. Isopropanol C. Methanol D. Tetradecanol 2. Which of the following statements about syrup of ipecac is not correct? A. Ipecac stimulates the area in the brain responsible for nausea and vomiting. B. Ipecac has a local irritant effect on the stomach. C. Ipecac should be used to induce vomiting in all patients, regardless of age or condition. D. Ipecac contains two active substances, emetine and cephaeline. 3. The odor of wintergreen on a child's breath might indicate ingestion of which chemical? A. Sodium hypochlorite B. Toluene C. Methyl salicylate D. Paradichlorobenzene 4. _______ is used to reverse an opiate (such as morphine or codeine) overdose. A. Flumazenil B. Atropine C. Naloxone D. Deferoxamine 5. Which of the following statements about syrup of ipecac is not correct? A. American poison control centers rarely recommend syrup of ipecac as an intervention. B. The side effects of ipecac ingestion include prolonged vomiting and lethargy. C. Syrup of ipecac has been available for years in pharmacies over-the-counter.