Côte D'ivoire Country Operational Plan (COP) 2016 Strategic Direction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

C O M M U N I Q
MINISTERE DE LA CONSTRUCTION, DU LOGEMENT REPUBLIQUE DE COTE D'IVOIRE DE L’ASSAINISSEMENT ET DE L'URBANISME Union - Discipline - Travail LE MINISTRE Abidjan, le N ________/MCLAU/CAB/bfe C O M M U N I Q U E Le Ministre de la Construction, de l’Assainissement et de l’Urbanisme a le plaisir d’informer les usagers demandeurs d’arrêté de concession définitive, dont les noms sont mentionnés ci-dessous que les actes demandés ont été signés et transmis à la Conservation Foncière. Les intéressés sont priés de se rendre à la Conservation Foncière concernée en vue du paiement du prix d'aliénation du terrain ainsi que des droits et taxes y afférents. Cinq jours après le règlement du prix d'aliénation suivi de la publication de votre acte au livre foncier, vous vous présenterez pour son retrait au service du Guichet Unique du Foncier et de l'Habitat. -

To the Management of Surface Water Resources in the Ivory Coast Basin of the Aghien Lagoon
International Journal of Scientific & Engineering Research Volume 10, Issue 10, October-2019 1605 ISSN 2229-5518 Application of the water evaluation and planning model (WEAP) to the management of surface water resources in the Ivory Coast basin of the Aghien lagoon 1Dabissi NOUFÉ Djibril, 2ZAMBLE Armand Tra Bi, 1DIALLO Seydou, 1SORO Emile Gnénéyougo, 1DAO Amidou, 1DIOMANDE Souleymane, EFFEBI Kôkôh Rose, 1KAMAGATÉ Bamory, 1GONÉ Droh Laciné, 3PATUREL Jean-Emmanuel, 2MAHE Gil, 1GOULA Bi Tié Albert, 3SERVAT Éric. Abstract —Water, an essential element of life, is of paramount importance in our countries, where it is increasingly scarce and threatened; we are constantly maintained by news where pollution, scarcity, flooding are mixed. As a result of cur- rent rapid climatic and demographic changes, the management of water resources by human being is becoming one of the major challenges of the 21st century, as water becoming an increasingly limited resource. It will now be necessary to use with modera- tion. This study is part of the project "Aghien Lagoon" (Abidjan) and its potential in terms of safe tape water resources. Mega- lopolis of about six million inhabitants (RGPH, 2014), Abidjan encounters difficulties of access to safe tape water due to the de- cline of the underground reserves and the increase the demand related to urban growth. Thus, the Aghien lagoon, the largest freshwater reserve near Abidjan, has been identified by the State of Côte d'Ivoire as a potential source of additive production of safe tape water. However, urbanization continues to spread on the slopes of this basin, while, at the same time, market garden- ing is developing, in order to meet the demand. -

Côte D'ivoire
CÔTE D’IVOIRE COI Compilation August 2017 United Nations High Commissioner for Refugees Regional Representation for West Africa - RSD Unit UNHCR Côte d’Ivoire UNHCR Regional Representation for West Africa - RSD Unit UNHCR Côte d’Ivoire Côte d’Ivoire COI Compilation August 2017 This report collates country of origin information (COI) on Côte d’Ivoire up to 15 August 2017 on issues of relevance in refugee status determination for Ivorian nationals. The report is based on publicly available information, studies and commentaries. It is illustrative, but is neither exhaustive of information available in the public domain nor intended to be a general report on human-rights conditions. The report is not conclusive as to the merits of any individual refugee claim. All sources are cited and fully referenced. Users should refer to the full text of documents cited and assess the credibility, relevance and timeliness of source material with reference to the specific research concerns arising from individual applications. UNHCR Regional Representation for West Africa Immeuble FAALO Almadies, Route du King Fahd Palace Dakar, Senegal - BP 3125 Phone: +221 33 867 62 07 Kora.unhcr.org - www.unhcr.org Table of Contents List of Abbreviations .............................................................................................................. 4 1 General Information ....................................................................................................... 5 1.1 Historical background ............................................................................................ -

L-Economie-Locale-D-Odienne-Denguele-Volume-1 5Lmqcr2k5kr5.Pdf
Commission Européenne /·e&2120,( /2&$/( '·2',(11e '(1*8e/e &Ñ7( '·,92,5( &RPSWHV DFWHXUV HW G\QDPLVPHV GH O·pFRQRPLH ORFDOH MALI BURKINA Korhogo Odienné GUINEE Boundiali Ferkessédougou Bouna Touba Katiola Dabakala Séguéla Bondoukou Man Daloa Abengourou YAMOUSSOUKRO Dimbokro GHANA LIBERIA ABIDJAN San Pedro Sassandra Grand Bassam Tabou 9ROXPH5DSSRUWJpQpUDO 6$+' -DQYLHU OCDE OECD ORGANISATION DE COOPERATION ET ORGANISATION FOR ECONOMIC DE DEVELOPPEMENT ECONOMIQUES CO-OPERATION AND DEVELOPMENT RÉPUBLIQUE DE CÔTE D’IVOIRE — Union – Discipline - Travail — MINISTÈRE DE L’INTÉRIEUR ET DE LA DÉCENTRALISATION L’économie locale d’Odienné (Denguélé) (Côte d’Ivoire) Comptes, acteurs et dynamiques de l’économie locale Volume 1 : Rapport général Commission Européenne Etude réalisée par : Ecole Nationale supérieure de Statistique et d’Economie Appliquée (ENSEA) Institut de recherche pour le développement (IRD) Septembre 2000 Table des matières AVANT-PROPOS........................................................................................................................................................ 3 CHAPITRE 1 : ODIENNÉ ET SON HINTERLAND. REPÈRES HISTORIQUES ............................................. 5 1. L’IMPLANTATION MALINKÉ DANS LA RÉGION. UNE VOCATION MARCHANDE, UNE ORGANISATION SOCIALE HIÉRARCHISÉE ............................................................................................................................................................ 5 2. LA VILLE D’ODIENNÉ........................................................................................................................................ -

Liste Des Centres De Collecte Du District D'abidjan
LISTE DES CENTRES DE COLLECTE DU DISTRICT D’ABIDJAN Région : LAGUNES Centre de Coordination: ABIDJAN Nombre total de Centres de collecte : 774 ABIDJAN 01 ABOBO Nombre de Centres de collecte : 155 CODE CENTRE DE COLLECTE 001 EPV CATHOLIQUE ST GASPARD BERT 002 EPV FEBLEZY 003 GROUPE SCOLAIRE LE PROVENCIAL ABOBO 004 COLLEGE PRIVE DJESSOU 006 COLLEGE COULIBALY SANDENI 008 G.S. ANONKOUA KOUTE I 009 GROUPE SCOLAIRE MATHIEU 010 E-PP AHEKA 011 EPV ABRAHAM AYEBY 012 EPV SAHOUA 013 GROUPE SCOLAIRE EBENEZER 015 GROUPE SCOLAIRE 1-2-3-4-5 BAD 016 GROUPE SCOLAIRE SAINT MOISE 017 EPP AGNISSANKO III 018 EPV DIALOGUE ET DESTIN 2 019 EPV KAUNAN I 020 GROUPE SCOLAIRE ABRAHAM AYEBY 021 EPP GENDARMERIE 022 GROUPE SAINTE FOI ABIDJAN 023 G. S. LES AMAZONES 024 EPV AMAZONES 025 EPP PALMERAIE 026 EPV DIALOGUE 1 028 INSTITUT LES PREMICES 030 COLLEGE GRACE DIVINE 031 GROUPE SCOLAIRE RAIL 4 BAD B ET C 032 EPV DIE MORY 033 EPP SAGBE I (BOKABO) 034 EPP ATCHRO 035 EPV ANOUANZE 036 EPV SAINT PAUL 037 EPP N'SINMON 039 COLLEGE H TAZIEFE 040 EPV LESANGES-NOIRS 041 GROUPE SCOLAIRE ASSAMOI 045 COLLEGE ANADOR 046 EPV LA PROVIDENCE 047 EPV BEUGRE 048 GROUPE SCOLAIRE HOUANTOUE 049 EPV SAINT-CYR 050 GROUPE SCOLAIRE SAINTE JEANNE 051 GROUPE SCOLAIRE SAINTE ELISABETH 052 EPP PLATEAU-DOKUI BAD 054 GROUPE SCOLAIRE ABOBOTE ANNEXE 055 GROUPE SCOLAIRE FENDJE 056 GROUPE SCOLAIRE ABOBOTE 057 EPV CATHOLIQUE SAINT AUGUSTIN 058 GROUPE SCOLAIRE LES ORCHIDEES 059 CENTRE D'EDUCATION PRESCOLAIRE 060 EPV REUSSITE 061 EPP GISCARD D'ESTAING 062 EPP LES FLAMBOYANTS 063 GROUPE SCOLAIRE ASSEMBLEE -

Côte D'ivoire Country Focus
European Asylum Support Office Côte d’Ivoire Country Focus Country of Origin Information Report June 2019 SUPPORT IS OUR MISSION European Asylum Support Office Côte d’Ivoire Country Focus Country of Origin Information Report June 2019 More information on the European Union is available on the Internet (http://europa.eu). ISBN: 978-92-9476-993-0 doi: 10.2847/055205 © European Asylum Support Office (EASO) 2019 Reproduction is authorised, provided the source is acknowledged, unless otherwise stated. For third-party materials reproduced in this publication, reference is made to the copyrights statements of the respective third parties. Cover photo: © Mariam Dembélé, Abidjan (December 2016) CÔTE D’IVOIRE: COUNTRY FOCUS - EASO COUNTRY OF ORIGIN INFORMATION REPORT — 3 Acknowledgements EASO acknowledges as the co-drafters of this report: Italy, Ministry of the Interior, National Commission for the Right of Asylum, International and EU Affairs, COI unit Switzerland, State Secretariat for Migration (SEM), Division Analysis The following departments reviewed this report, together with EASO: France, Office Français de Protection des Réfugiés et Apatrides (OFPRA), Division de l'Information, de la Documentation et des Recherches (DIDR) Norway, Landinfo The Netherlands, Immigration and Naturalisation Service, Office for Country of Origin Information and Language Analysis (OCILA) Dr Marie Miran-Guyon, Lecturer at the École des Hautes Études en Sciences Sociales (EHESS), researcher, and author of numerous publications on the country reviewed this report. It must be noted that the review carried out by the mentioned departments, experts or organisations contributes to the overall quality of the report, but does not necessarily imply their formal endorsement of the final report, which is the full responsibility of EASO. -

“Abidjan: Floods, Displacements, and Corrupt Institutions”
“Abidjan: Floods, Displacements, and Corrupt Institutions” Abstract Abidjan is the political capital of Ivory Coast. This five million people city is one of the economic motors of Western Africa, in a country whose democratic strength makes it an example to follow in sub-Saharan Africa. However, when disasters such as floods strike, their most vulnerable areas are observed and consequences such as displacements, economic desperation, and even public health issues occur. In this research, I looked at the problem of flooding in Abidjan by focusing on their institutional response. I analyzed its institutional resilience at three different levels: local, national, and international. A total of 20 questionnaires were completed by 20 different participants. Due to the places where the respondents lived or worked when the floods occurred, I focused on two out of the 10 communes of Abidjan after looking at the city as a whole: Macory (Southern Abidjan) and Cocody (Northern Abidjan). The goal was to talk to the Abidjan population to gather their thoughts from personal experiences and to look at the data published by these institutions. To analyze the information, I used methodology combining a qualitative analysis from the questionnaires and from secondary sources with a quantitative approach used to build a word-map with the platform Voyant, and a series of Arc GIS maps. The findings showed that the international organizations responded the most effectively to help citizens and that there is a general discontent with the current local administration. The conclusions also pointed out that government corruption and lack of infrastructural preparedness are two major problems affecting the overall resilience of Abidjan and Ivory Coast to face this shock. -

Region Du Kabadougou
REPUBLIQUE DE CÔTE D’IVOIRE Union- Discipline-Travail MINISTERE DE L’EDUCATION NATIONALE, DE L’ENSEIGNEMENT TECHNIQUE ET DE LA FORMATION PROFESSIONNELLE REGION DU KABADOUGOU ANNUAIRE STATISTIQUE SCOLAIRE 2017 - 2018 MENET-FP/DSPS/DRENET ODIENNE/ANNUAIRE STATISTIQUE SCOLAIRE 2017-2018:REGION DU KABADOUGOU PAGE 1 SOMMAIRE A .PRESCOLAIRE ................................................................................................................ Erreur ! Signet non défini. A-1. DONNEES SYNTHETIQUES ........................................................................................ Erreur ! Signet non défini. Tableau 1 : Répartition des infrastructures, des effectifs élèves et des enseignants par département, par sous-préfecture et par statut .......................................................................................... Erreur ! Signet non défini. Graphique A-1. Proportion des écoles par statut dans le préscolaire ........................ Erreur ! Signet non défini. Graphique A-2. Proportion des élèves par statut dans le préscolaire ........................ Erreur ! Signet non défini. Graphique A-3. Proportion des élèves selon le genre dans le préscolaire .................. Erreur ! Signet non défini. Tableau 2 : Répartition des élèves par niveau d’études et selon l’âge .................... Erreur ! Signet non défini. A-2. INDICATEURS GLOBAUX ........................................................................................... Erreur ! Signet non défini. Tableau 3 : Proportion des élèves filles et des enseignantes -

Côte D'ivoire
Côte d’Ivoire Human Rights Violations in Abidjan during an Opposition Demonstration - March 2004 Human Rights Watch Briefing Paper, October 2004 Introduction................................................................................................................................... 1 Background to Events Surrounding the March 25, 2004 Demonstration ........................... 2 The Ivorian Government Position............................................................................................. 4 Violations by Pro-Government forces: Ivorian Police, Gendarmes and Army .................. 6 Violations by Pro-Government Forces: Militias and FPI Militants ..................................... 9 The Role of Armed Demonstrators.........................................................................................12 Mob Violence by the Demonstrators ......................................................................................14 Lack of Civilian Protection by Foreign Military Forces........................................................16 Legal Aspects ...............................................................................................................................17 Conclusion....................................................................................................................................18 Introduction The events associated with a demonstration in the Ivorian commercial capital of Abidjan by opposition groups planned for March 25, 2004, were accompanied by a deadly crackdown by government -
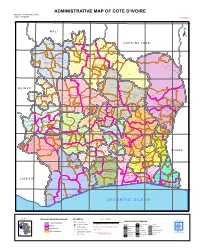
ADMINISTRATIVE MAP of COTE D'ivoire Map Nº: 01-000-June-2005 COTE D'ivoire 2Nd Edition
ADMINISTRATIVE MAP OF COTE D'IVOIRE Map Nº: 01-000-June-2005 COTE D'IVOIRE 2nd Edition 8°0'0"W 7°0'0"W 6°0'0"W 5°0'0"W 4°0'0"W 3°0'0"W 11°0'0"N 11°0'0"N M A L I Papara Débété ! !. Zanasso ! Diamankani ! TENGRELA [! ± San Koronani Kimbirila-Nord ! Toumoukoro Kanakono ! ! ! ! ! !. Ouelli Lomara Ouamélhoro Bolona ! ! Mahandiana-Sokourani Tienko ! ! B U R K I N A F A S O !. Kouban Bougou ! Blésségué ! Sokoro ! Niéllé Tahara Tiogo !. ! ! Katogo Mahalé ! ! ! Solognougo Ouara Diawala Tienny ! Tiorotiérié ! ! !. Kaouara Sananférédougou ! ! Sanhala Sandrégué Nambingué Goulia ! ! ! 10°0'0"N Tindara Minigan !. ! Kaloa !. ! M'Bengué N'dénou !. ! Ouangolodougou 10°0'0"N !. ! Tounvré Baya Fengolo ! ! Poungbé !. Kouto ! Samantiguila Kaniasso Monogo Nakélé ! ! Mamougoula ! !. !. ! Manadoun Kouroumba !.Gbon !.Kasséré Katiali ! ! ! !. Banankoro ! Landiougou Pitiengomon Doropo Dabadougou-Mafélé !. Kolia ! Tougbo Gogo ! Kimbirila Sud Nambonkaha ! ! ! ! Dembasso ! Tiasso DENGUELE REGION ! Samango ! SAVANES REGION ! ! Danoa Ngoloblasso Fononvogo ! Siansoba Taoura ! SODEFEL Varalé ! Nganon ! ! ! Madiani Niofouin Niofouin Gbéléban !. !. Village A Nyamoin !. Dabadougou Sinémentiali ! FERKESSEDOUGOU Téhini ! ! Koni ! Lafokpokaha !. Angai Tiémé ! ! [! Ouango-Fitini ! Lataha !. Village B ! !. Bodonon ! ! Seydougou ODIENNE BOUNDIALI Ponondougou Nangakaha ! ! Sokoro 1 Kokoun [! ! ! M'bengué-Bougou !. ! Séguétiélé ! Nangoukaha Balékaha /" Siempurgo ! ! Village C !. ! ! Koumbala Lingoho ! Bouko Koumbolokoro Nazinékaha Kounzié ! ! KORHOGO Nongotiénékaha Togoniéré ! Sirana -

Côte D'ivoire
AFRICAN DEVELOPMENT BANK GROUP PROJECT: ROAD DEVELOPMENT AND TRANSPORT FACILITATION PROGRAMME WITHIN THE MANO RIVER UNION COUNTRY: COTE D’IVOIRE, GUINEA, AND LIBERIA SUMMARY ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT (ESIA) Team Leader J. N. ILBOUDO, Transport Engineer OITC.1 5012 J.B. AGUMA, Transport Economist OITC.1 1956 J. P.M. KALALA , Chief Socio-Economist OITC.1 3561 N. KULEMEKA, Chief Socio-Economist SARC/ONEC.3 8452 L. M. KINANE, Environmentalist ONEC.3 2933 E. NDINYA, Environmentalist SARC/ONEC.3 1541 LRFO/OITC.1 7072 P. TAMBAH, Infrastructure Engineer Team Members Project Malick Soumare, Procurement Specialist ORPF.1/ LRFO Team M. H . SANON , Socio-Economist ONEC-3 Mose Mabe-Koofhethile, Procurement Specialist ORPF.1/ SNFO Sector Division Jean Kizito KABANGUKA OITC1 2143 Manager Sector Director Amadou OUMAROU OITC 3075 Regional Director Franck Joseph PERRAULT ORWA 4046 Director, Regional Janvier K. LITSE ONRI 4047 Integration and Trade 2 SUMMARY ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT Project Name : Road Development and Transport Project No.: P-Z1-DB0-103 Facilitation Programme Within the Mano River Union Countries: Cote d’Ivoire, Guinea and Liberia Depart ment : OITC Division: OITC-1 Introduction This document is a Summary Environmental and Social Impact Assessment (ESIA) of the Ivorian section of the Road Development and Transport Facilitation Programme within the Mano River Union. The summary has been prepared in accordance with the guidelines and procedures for environmental and social assessment of the African Development Bank (AfDB) for Category 1 projects, as well as with the policies in force in Côte d'Ivoire. The project description and rationale are presented first, followed by the applicable legal and institutional framework in Côte d'Ivoire. -

Update No. 12 Côte D'ivoire Situation
Update No. 12 Côte d’Ivoire Situation 05 May 2011 HIGHLIGHTS • The inauguration of Mr. Alassane Ouattara as President of Côte d’Ivoire is scheduled to take place on 21 May. • The Ivorian Red Cross reported 60 dead bodies in the Yopougon neighbourhood of Abidjan after ongoing fighting between the “Forces Républicaines de Côte d’Ivoire” and the pro-Gbagbo militias. • On Monday 02 May, Laurent Gbagbo met with the South-African Archbishop, Desmond Tutu alongside former UN Secretary-General Kofi Annan and former Irish President and UN human rights chief Mary Robinson in Korhogo in the north of Côte d’Ivoire. • The government has started paying civil service salaries, which were on hold during the conflict. • Long queues formed at banks that re-opened on 26 April, after having been closed for two and a half months. Armed robberies of the Banque de l’Habitat de Côte d’Ivoire and Group BNP Paribas vaults were reported on the same day. Community members in Awobo Village, Anyama (Abidjan) met UNHCR, ASAPSU and MESAD at the home of their chief to share the news and express the trauma inflicted upon their community during the period of conflict. (PERHAM S/ UNHCR/29 April 2011). Population Movement Burkina Guinea Sierra Country Guinea Mali Ghana Togo Benin Niger Nigeria Senegal Gambia Faso Bissau Leone Refugees/ Asylum 2,699 107 880 13,508 3,851 239 38 104 41 38 47 10 seekers Liberia 45,729 Ivorian refugees individually registered and 120,192 through the rapid emergency registration. In view of the volatile situation in Côte d’Ivoire, UNHCR is not yet in a position to provide exact figures.