Neurotoxic Disorders of Organophosphorus Compounds and Their Managements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Global Insecticide Use for Vector-Borne Disease Control
WHO/CDS/NTD/WHOPES/GCDPP/2007.2 GLOBAL INSECTICIDE USE FOR VECTOR-BORNE DISEASE CONTROL M. Zaim & P. Jambulingam DEPARTMENT OF CONTROL OF NEGLECTED TROPICAL DISEASES (NTD) WHO PESTICIDE EVALUATION SCHEME (WHOPES) First edition, 2002 Second edition, 2004 Third edition, 2007 © World Health Organization 2007 All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either express or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. The named authors alone are responsible for the views expressed in this publication. CONTENTS Page Acknowledgements i Introduction 1 Collection of information 2 Data analysis and observations on reporting 3 All uses in vector control 6 Malaria vector control 22 Dengue vector control 38 Chagas disease vector control 48 Leishmaniasis vector control 52 Other vector-borne disease control 56 Selected insecticides – DDT 58 Selected insecticides – Insect growth regulators 60 Selected insecticides – Bacterial larvicides 62 Country examples 64 Annex 1. -

US EPA Environmental Technology Verification Statement Removal of Chemical Contaminants in Drinking Water Watts Premier Inc
THE ENVIRONMENTAL TECHNOLOGY VERIFICATION PROGRAM U.S. Environmental Protection Agency NSF International ETV Joint Verification Statement TECHNOLOGY TYPE: POINT-OF-USE DRINKING WATER TREATMENT SYSTEM APPLICATION: REMOVAL OF CHEMICAL CONTAMINANTS IN DRINKING WATER PRODUCT NAME: WATTS PREMIER WP-4V COMPANY: WATTS PREMIER, INC. ADDRESS: 1725 WEST WILLIAMS DR. SUITE C-20 PHOENIX, AZ 85027 PHONE: 800-752-5582 NSF International (NSF) manages the Drinking Water Systems (DWS) Center under the U.S. Environmental Protection Agency’s (EPA) Environmental Technology Verification (ETV) Program. The DWS Center recently evaluated the performance of the Watts Premier WP-4V point-of-use (POU) drinking water treatment system. NSF performed all of the testing activities, and also authored the verification report and this verification statement. The verification report contains a comprehensive description of the test. EPA created the ETV Program to facilitate the deployment of innovative or improved environmental technologies through performance verification and dissemination of information. The goal of the ETV Program is to further environmental protection by accelerating the acceptance and use of improved and more cost-effective technologies. ETV seeks to achieve this goal by providing high-quality, peer- reviewed data on technology performance to those involved in the design, distribution, permitting, purchase, and use of environmental technologies. ETV works in partnership with recognized standards and testing organizations, stakeholder groups (consisting of buyers, vendor organizations, and permitters), and with the full participation of individual technology developers. The program evaluates the performance of innovative technologies by developing test plans that are responsive to the needs of stakeholders, conducting field or laboratory tests (as appropriate), collecting and analyzing data, and preparing peer reviewed reports. -
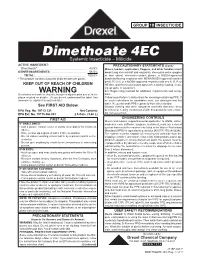
Dimethoate 4EC Systemic Insecticide – Miticide ACTIVE INGREDIENT: PRECAUTIONARY STATEMENTS (Cont.) Dimethoate*
GROUP 1B INSECTICIDE Dimethoate 4EC Systemic Insecticide – Miticide ACTIVE INGREDIENT: PRECAUTIONARY STATEMENTS (Cont.) Dimethoate* .......................................................... 43.5% Mixers, loaders, applicators, flaggers, and other handlers must OTHER INGREDIENTS: .......................................... 56.5% wear: Long-sleeved shirt and long pants, shoes plus socks, goggles TOTAL: .............................................................. 100.0% or face shield, chemical-resistant gloves, a NIOSH-approved * This product contains 4 pounds of dimethoate per gallon. dust/mist filtering respirator with MSHA/NIOSH approval number prefix TC-21C or a NIOSH-approved respirator with any N, R, P, or KEEP OUT OF REACH OF CHILDREN HE filter, and chemical-resistant apron when mixing, loading, clean- ing up spills, or equipment. WARNING See Engineering Controls for additional requirements and excep- Si usted no entiende la etiqueta, busque a alguien para que se la ex- tions. plique a usted en detalle. (If you do not understand the label, find Follow manufacturer’s instructions for cleaning/maintaining PPE. If someone to explain it to you in detail.) no such instructions for washables exist, use detergent and hot water. Keep and wash PPE separately from other laundry. See FIRST AID Below Discard clothing and other absorbent materials that have been EPA Reg. No. 19713-231 Net Content: drenched or heavily contaminated with this product’s concentrate. EPA Est. No. 19713-GA-001 2.5 Gals. (9.46 L) Do not reuse them. ENGINEERING CONTROLS FIRST AID Mixers and loaders supporting aerial application to alfalfa, cotton, IF SWALLOWED: soybeans, corn, safflower, sorghum, and wheat, must use a closed • Call a poison control center or doctor immediately for treatment system that meets the requirements listed in the Worker Protections advice. -

Toxic Influence of Diazinon As an Organophosphate Pesticide on Parameters of Dry Matter Degradability According to in Situ Technique M
International Journal of Basic & Applied Sciences IJBAS-IJENS Vol:12 No:06 229 Toxic Influence of Diazinon as an Organophosphate Pesticide on Parameters of Dry Matter Degradability According to in Situ Technique M. Kazemi*, A. M. Tahmasbi, R. Valizadeh, A. A. Naserian Department of Animal Science, Excellence Center for Animal Science, Faculty of Agriculture, Ferdowsi University of Mashhad, P. O. Box 91775-1163, Mashhad, Islamic Republic of Iran. *Corresponding author email: [email protected] Abstract-- Many feed and forages are exposed to low, medium metabolizing phosphate insecticides in vitro. Parathion was or high levels of organophosphorous (OP) pesticides. It is unclear reduced to aminoparathion by bovine rumen fluid. Kutches et whether these exposures (for example diazinon as an OP al. [15] reported that toxaphene was the most inhibitory of the pesticide) impact dry matter degradability parameters. So, pesticides tested and resulted in greater decreases of the in different levels (0, 0.7, 2.8 and 5.6 mg) of diazinon as an OP vitro dry matter disappearance, volatile fatty acids and rumen pesticide with different levels of calcium bentonite (CB) (0 and 100 mg) as a toxin binder were tested for their toxicological protozoa. Inhibitory effects of OP pesticides such as effects on in vitro dry matter disappearance. Also we investigated phosphomidon, chlorpyrifos and phosalone on tetrahymena whether CB can inactivate the probably deleterious effects of Spp. Were reported by Hoskin et al. [10]. Dauterman et al. [7] contaminated forage with diazinon in the situ procedure or not. treated rats and cattle with radioactive dimethoate and The study indicated that effect of diazinon with adding the analyzed blood, tissue, milk, and excreta. -

Validation Report 20
EURL for Cereals and Feeding stuff National Food Institute Technical University of Denmark Validation Report 20 Determination of pesticide residues in rice baby food by GC-MS/MS and LC-MS/MS (QuEChERS method) Parvaneh Hajeb Susan Strange Herrmann Mette Erecius Poulsen December 2015 Page 2 of 18 CONTENT: 1. Introduction ...................................................................................................................................... 3 2. Principle of analysis......................................................................................................................... 3 3. Validation design ............................................................................................................................. 4 4. Chromatograms and calibration curves .......................................................................................... 5 5. Validation parameters...................................................................................................................... 9 6. Criteria for the acceptance of validation results ........................................................................... 10 7. Results and discussion ................................................................................................................... 10 8. Conclusions .................................................................................................................................... 12 9. References ..................................................................................................................................... -

Determination of Age-Related Differences in Activation and Detoxication of Organophosphates in Rat and Human Tissues
Mississippi State University Scholars Junction Theses and Dissertations Theses and Dissertations 8-10-2018 Determination of Age-Related Differences in Activation and Detoxication of Organophosphates in Rat and Human Tissues Edward Caldwell Meek Follow this and additional works at: https://scholarsjunction.msstate.edu/td Recommended Citation Meek, Edward Caldwell, "Determination of Age-Related Differences in Activation and Detoxication of Organophosphates in Rat and Human Tissues" (2018). Theses and Dissertations. 1339. https://scholarsjunction.msstate.edu/td/1339 This Dissertation - Open Access is brought to you for free and open access by the Theses and Dissertations at Scholars Junction. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Scholars Junction. For more information, please contact [email protected]. Template A v3.0 (beta): Created by J. Nail 06/2015 Determination of age-related differences in activation and detoxication of organophosphates in rat and human tissues By TITLE PAGE Edward Caldwell Meek A Dissertation Submitted to the Faculty of Mississippi State University in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Environmental Toxicology in the College of Veterinary Medicine Mississippi State, Mississippi August 2018 Copyright by COPYRIGHT PAGE Edward Caldwell Meek 2018 Determination of age-related differences in activation and detoxication of organophosphates in rat and human tissues By APPROVAL PAGE Edward Caldwell Meek -

Agents for Defense Against Chemical Warfare: Reactivators of Acetylcholinesterase Inhibited with Neurotoxic Organophosphorus Compounds **
Mil. Med. Sci. Lett. (Voj. Zdrav. Listy) 2015, vol. 84(3), p. 115-127 ISSN 0372-7025 DOI: 10.31482/mmsl.2015.013 REVIEW ARTICLE AGENTS FOR DEFENSE AGAINST CHEMICAL WARFARE: REACTIVATORS OF ACETYLCHOLINESTERASE INHIBITED WITH NEUROTOXIC ORGANOPHOSPHORUS COMPOUNDS ** Petronilho, E. C., Figueroa-Villar, J. D. Chemistry Engineering Section, Medicinal Chemistry Group, Military Institute of Engineering, Praça General Tibúrcio, 80, Urca, 22290-270, Rio de Janeiro, RJ, Brazil. Received 30 th April 2015. Revised 7 th July 2015. Published 4 th September 2015. Summary The chemical warfare agents and neurotoxic agents are an important threat to people all over the world, and require special attention because they are highly dangerous. Most of these agents are neurotoxic organophosphorus compounds (OP), which inhibit the enzyme acetylcholinesterase (AChE), which is responsible for controlling the transmission of nerve impulses. To be inhibited by these compounds, AChE can sometimes be reactivated using cationic oximes, which are the most used substances for this reactivation. Until today there have not been discovered agents for complete treatment of poisoning by all OPs. For this reason, the treatment of intoxicated people requires the determination of the absorbed OP, in order to select the appropriate activator, a process that usually requires long time and may cause death. Therefore, this study aims to do a review on the OPs used as chemical warfare agents and the process of inhibition and reactivation of AChE, especially to motivate the development of new agents for defense against chemical weapons, a process that is very important for protecting all humanity. Key words: acetylcholinesterase; AChE reactivators; organophosphorus; oximes; warfare agents INTRODUCTION pounds (OP), which are highly toxic, allowing their use with small quantities in order to cause seizures The use of chemical warfare agents is a major and death. -
EPA Method 538: Determination of Selected Organic Contaminants in Drinking Water with Direct Aqueous Injection LC/MS/MS
EPA Method 538: Determination of Selected Organic Contaminants in Drinking Water with Direct Aqueous Injection LC/MS/MS E. Michael Thurman and Imma Ferrer Center for Environmental Mass Spectrometry University of Colorado Boulder, CO, USA Confidentiality Label 1 March 20, 2012 Abstract EPA Method 538 is a new method from EPA for organophosphate pesticides in drinking water. It uses direct aqueous injection; thus, no sample preparation is needed. We use both UHPLC (Agilent 1290) and MS/MS (Agilent 6460) analysis for rapid analysis and sensitive detection with ng/L limits of detection. A second MRM is added for more reliable identification. Confidentiality Label 2 March 20, 2012 Hypothesis Direct injection of organophosphate pesticides (EPA Method 538) will work by UHPLC (Agilent Model 1290) and LC/MS/MS with Jetstream (Agilent Model 6460) with trace level detection at ng/L concentrations. Confidentiality Label 3 March 20, 2012 1. Introduction-Summary 1.1 EPA Method 538 (published in November 2009 by Shoemaker) deals with Organophosphate pesticides in drinking water (1) and one other contaminant, quinoline. 1.2 The method consists of 10 compounds: acephate, aldicarb, aldicarb sulfoxide, dicrotophos, diisopropylmethylphosphonate (DIMP), fenamiphos sulfone, fenamiphos sulfoxide, methamidophos, oxydemeton methyl, quinoline, and thiofanox with 5 labeled internal standards. 1.3 Direct aqueous injection is used with a large volume sample of 100 microliters; thus, no sample preparation is needed. 1.4 Because solid phase extraction (i.e. concentration of the sample is not carried out) suppression is mimimized in the analysis. 1.5 Part-per-Trillion Detection Limits. Confidentiality Label 4 March 20, 2012 Introduction 1.1: EPA Method 538: Determination of Selected Organic Contaminants in Drinking Water by Direct Aqueous Injection by Jody Shoemaker, EPA Cincinnati, OH [email protected] 513-569-7298 Confidentiality Label 5 March 20, 2012 Introduction: 1.2. -

Development and Validation of a Method for the Simultaneous
CORE Metadata, citation and similar papers at core.ac.uk Provided by UGD Academic Repository American Journal of Applie d Chemistry 2014; 2(4): 46-54 Published online August 10, 2014 (http://www.sciencepublishinggroup.com/j/ajac) doi: 10.11648/j.ajac.20140204.11 ISSN: 2330-8753 (Print); ISSN: 2330-8745 (Online) Development and validation of a method for the simultaneous determination of 20 organophosphorus pesticide residues in corn by accelerated solvent extraction and gas chromatography with nitrogen phosphorus detection Vesna Kostik *, Biljana Gjorgeska, Bistra Angelovska Medical Faculty, Department of Pharmacy, University “Goce Delchev”, Shtip, Republic of Macedonia Email address: [email protected] (V. Kostik), [email protected] (B. Gjorgeska), [email protected] (B. Angelovska) To cite this article: Vesna Kostik, Biljana Gjorgeska, Bistra Angelovska. Development and Validation of a Method for the Simultaneous Determination of 20 Organophosphorus Pesticide Residues in Corn by Accelerated Solvent Extraction and Gas Chromatography with Nitrogen Phosphorus Detection. American Journal of Applied Chemistry. Vol. 2, No. 4, 2014, pp. 46-54. doi: 10.11648/j.ajac.20140204.11 Abstract: The method for simultaneous determination of 20 organophosphorus pesticide residues in corn samples has been developed and validated. For the extraction of organophosporus pesticide residues from the samples, the accelerated solvent technique with the mixture of dichloromethane: acetone (1:1, V/V ) was used. Clean up was done using liquid – liquid extraction with n – hexane, followed by solid phase extraction on primary secondary amine adsorbent, and elution with the mixture of acetone: toluene (65:35). The determination of the pesticides was carried out by gas chromatography with nitrogen phosphorus detection. -

20110628140658587.Pdf
1210 YUE ET AL.:JOURNAL OF AOAC INTERNATIONAL VOL. 91, NO. 5, 2008 SPECIAL GUEST EDITOR SECTION High-Performance Thin-Layer Chromatographic Analysis of Selected Organophosphorous Pesticide Residues in Tea YONGDE YUE International Center for Bamboo and Rattan, 100102, Beijing, People’s Republic of China RONG ZHANG and WEI FAN Key Laboratory for Agri-Food Safety of Anhui Province, School of Resources and Environment, Anhui Agricultural University, Hefei, Anhui, 230036, People’s Republic of China FENG TANG International Center for Bamboo and Rattan, 100102, Beijing, People’s Republic of China The separation of 9 organophosphates determination procedure. In many cases, searching for a fast (monocrotophos, quinalphos, triazophos, and efficient method for enrichment and determination of parathion-methyl, isofenphos-methyl, temephos, organophosphorous residues from complex matrixes is still a parathion, phoxim-ethyl, and chlorpyrifos) by challenge for many researchers. high-performance thin-layer chromatography In many analytical situations, modern quantitative (HPTLC) with automated multiple development was high-performance thin-layer chromatography (HPTLC), studied. The HPTLC method was developed and when properly performed by well-trained analysts, has many validated for analysis of residues of phoxim-ethyl advantages over HPLC or GC. These advantages include and chlorpyrifos in tea. The sample was extracted simplicity of operation, the availability of many sensitive and with acetonitrile and cleaned up by ENVI-CARB selective reagents for detection and confirmation without solid-phase extraction. The extract was directly interference from the mobile phase, the ability to repeat applied as bands to glass-backed silica gel 60F254 detection and quantification at any time with changed HPTLC plates. -
Guide No. 1 – October 2020 2/12 the CONCEPT and IMPLEMENTATION of CPA GUIDANCE RESIDUE LEVELS
Cooperation Centre for Scientific Research Relative to Tobacco CORESTA GUIDE N° 1 The Concept and Implementation of CPA Guidance Residue Levels October 2020 Agro-Chemical Advisory Committee CORESTA TECHNICAL GUIDE N° 1 Title: The Concept and Implementation of CPA Guidance Residue Levels Status: Valid Note: This document will be periodically reviewed by CORESTA Document history: Date of review Information July 2003 Version 1 GRL for Pyrethrins () and Terbufos corrected. December 2003 CPA terminology corrected. June 2008 Version 2 – GRLs revised and residue definitions added Provisional GRL of 2.00 ppm for Cyfluthrin to replace previous June 2010 GRL of 0.50 ppm July 2013 Version 3 – GRLs revised October 2013 Note for Maleic Hydrazide revised Version 4 – GRLs revised + clarification that scope of GRLs July 2016 applies predominantly to the production of traditional cigarette tobaccos and GAP associated with their cultivation. June 2018 Fluopyram GRL of 5 ppm added to GRL list Version 5 – Nine new CPAs with GRL added to list. November 2019 Revision of GRLs for Chlorantraniliprole and Indoxacarb. Updated web links. October 2020 Version 6 – Flupyradifurone GRL of 21 ppm added to GRL list. CORESTA Guide No. 1 – October 2020 2/12 THE CONCEPT AND IMPLEMENTATION OF CPA GUIDANCE RESIDUE LEVELS Executive Summary • Guidance Residue Levels (GRLs) are in the remit of the Agro-Chemical Advisory Committee (ACAC) of CORESTA. Their development is a joint activity of all ACAC members, who represent the leaf production, processing and manufacturing sectors of the Tobacco Industry. The concept of GRLs and their implementation are described in this guide. • GRLs provide guidance to tobacco growers and assist with interpretation and evaluation of results from analyses of residues of Crop Protection Agents (CPAs*). -

162998571.Pdf
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Liverpool Repository Please do not adjust margins Investigating the breakdown of the nerve agent simulant methyl paraoxon and chemical warfare agents GB and VX using nitrogen containing bases Received 00th January 20xx, Accepted 00th January 20xx Craig Wilson,a Nicholas J. Cooper,b Michael E. Briggs,a Andrew I. Cooper,*a and Dave J. Adams*c DOI: 10.1039/x0xx00000x A range of nitrogen containing bases was tested for the hydrolysis of a nerve agent simulant, methyl paraoxon (MP), and www.rsc.org/ the chemical warfare agents, GB and VX. The product distribution was found to be highly dependant on the basicity of the base and the quantity of water used for the hydrolysis. This study is important in the design of decontamination technology, which often involve mimics of CWAs. production of EA-2192 Introduction (S-(2-diisopropylaminoethyl) methylphosphonothioic acid), which exhibits roughly the same toxicity as VX itself.12 The Chemical warfare agents (CWAs) have a devastating effect on blister agent HD (Fig. 1d) can also undergo deactivation via the body and will disable or kill on exposure. Blister agents, such hydrolysis.13 However, its poor water solubility reduces the as sulfur mustard (HD, bis(2-chloroethyl) sulfide), target the skin efficiency of this decontamination method.14 As a result, and respiratory system causing severe pain and damage to the oxidation to the sulfoxide, or the addition of a co-solvent is most body whereas nerve agents, such as sarin (GB, isopropyl commonly used for HD deactivation.15-17 methylphosphonofluoridate) and VX (O-ethyl The high toxicity of CWAs means that research into their S-[2-(diisopropylamino)ethyl] methylphosphonothioate), target deactivation is often carried out using simulants.