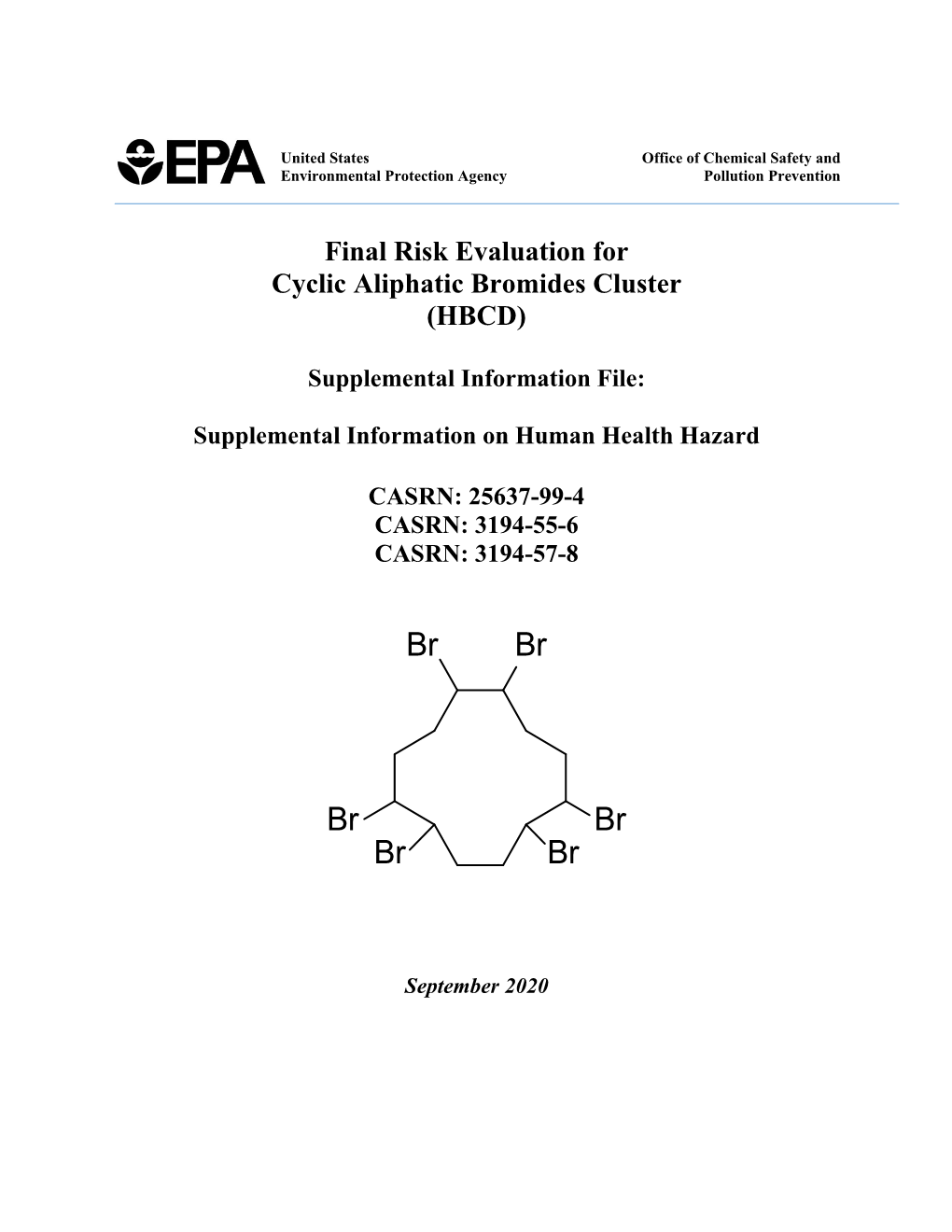
Supplemental Information on Human Health Hazard
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ethnicity, Confession and Intercultural Dialogue at the European Union's
Munich Personal RePEc Archive Ethnicity, Confession and Intercultural Dialogue at the European Union’s East Border Brie, Mircea and Horga, Ioan and Şipoş, Sorin University of Oradea, Romania 2011 Online at https://mpra.ub.uni-muenchen.de/44082/ MPRA Paper No. 44082, posted 31 Jan 2013 05:28 UTC ETHNICITY, CONFESSION AND INTERCULTURAL DIALOGUE AT THE EUROPEAN UNION EASTERN BORDER ETHNICITY, CONFESSION AND INTERCULTURAL DIALOGUE AT THE EUROPEAN UNION EASTERN BORDER Mircea BRIE Ioan HORGA Sorin ŞIPOŞ (Coordinators) Debrecen/Oradea 2011 This present volume contains the papers of the international conference Ethnicity, Confession and Intercultural Dialogue at the European Union‟s East Border, held in Oradea between 2nd-5th of June 2011, organized by Institute for Euroregional Studies Oradea-Debrecen, University of Oradea and Department of International Relations and European Studies, with the support of the European Commission and Bihor County Council. CONTENTS INTRODUCTORY STUDIES Mircea BRIE Ethnicity, Religion and Intercultural Dialogue in the European Border Space.......11 Ioan HORGA Ethnicity, Religion and Intercultural Education in the Curricula of European Studies .......19 MINORITY AND MAJORITY IN THE EASTERN EUROPEAN AREA Victoria BEVZIUC Electoral Systems and Minorities Representations in the Eastern European Area........31 Sergiu CORNEA, Valentina CORNEA Administrative Tools in the Protection and Promotion of the Rights of Ethnic Minorities .............................................................................................................47 -

March 2007 Master Name Index List * Number in Front of Each
March 2007 Master Name Index List 2 Caas, 1 Cadenhead,Jim 3 Cady,Charlotte 1 Caas,Catherine 2 Cadieux, 1 Cady,Cornelius S. 2 Caas,Frank 1 Cadle, 1 Cady,Eliza L.(Everetts) 2 Caas,John 1 Cadle,Sarah 1 Cady,Frank W. 2 Caas,John F. 1 Cadogan,Catherine 1 Cady,Fred 1 Caas,John N. 1 Cadogan,Lavina(Bradshaw) 1 Cady,G.C. 1 Caas,N. 1 Cadogan,Nellie 1 Cady,H.N. 1 Caas,Nic 1 Cadogan,Walter 1 Cady,H.Olin 1 Caas,Nic. 1 Cadwallader, 1 Cady,Harriett(Bishop) 9 Caas,Nicholas 1 Cadwallader,John 1 Cady,Hattie(Yates) 1 Caas,Susie 1 Cadwallader,Mary A.(Collins) 1 Cady,Helen L.(Howard) 1 Caas,Theresa(Wolf) 1 Cadwallader,Morris 1 Cady,Louis 1 Caas,Vic 1 Cadwalter, 1 Cady,Louis N. 1 Caballero,Hector M. 1 Cadwalter,Dennis 1 Cady,M.E. 1 Cabel, 2 Cadwell, 3 Cady,Martin E. 3 Cable, 1 Cadwell,Addie M. 1 Cady,Mary L. 1 Cable,Betsey K. 1 Cadwell,B. 4 Cady,Nancy 1 Cable,C. 1 Cadwell,Badish 1 Cady,Oliver 2 Cable,Cornelia 2 Cadwell,Bradish 2 Cady,Palmer 1 Cable,F.S. 1 Cadwell,C. 1 Cady,Ruby M. 2 Cable,H.B. 1 Cadwell,Clara 1 Cady,Sarah M. 1 Cable,M.A. 5 Cadwell,Cordelia 1 Cady,Willia1m 1 Cable,M.C. 1 Cadwell,E. 1 Cady,William 2 Cable,M.H. 5 Cadwell,Edgar 4 Cady,Wm. 2 Cable,Marvin H. 1 Cadwell,Ernest 1 Cady,Wm.W. 1 Cable,Stella M. -

ROCZNIKI PAŃSTWOWEGO ZAKŁADU HIGIENY - 2019, Vol
ROCZNIKI PAŃSTWOWEGO ZAKŁADU HIGIENY ISSN 0035-7715 [ANNALS OF THE NATIONAL INSTITUTE OF HYGIENE] eISSN 2451-2311 Volume 70 2019 Number 3 Nutrition of vegetarians in Poland – a review of research. Paulina Skorek, Paweł Glibowski, Katarzyna Banach ..................................................................................................... 217 Mobile telephony and its effects on human health. ROCZNIKI Andrzej Magiera, Jolanta Solecka .................................................................................................................................... 225 Role of nutritional support provided by qualified dietitians in the prevention and treatment of non-communicable diseases. Barbara Bednarczuk, Anna Czekajło-Kozłowska ............................................................................................................. 235 PAŃSTWOWEGO Body composition and nutrition of female athletes. Karol Pilis, Krzysztof Stec, Anna Pilis, Agata Mroczek, Cezary Michalski, Wiesław Pilis .............................................. 243 ZAKŁADU HIGIENY Lower weight gain after vaping cessation than after smoking quitting. Ewelina Wawryk-Gawda, Michał K. Zarobkiewicz, Patrycja Chylińska-Wrzos, Barbara Jodłowska-Jędrych ............... 253 Assessment of selected food intake frequency in patients with type 1 diabetes treated with personal insulin pumps. Sabina Krzyżowska, Bartłomiej Matejko, Beata Kieć-Wilk, Magdalena Wilk, Maciej Małecki, Tomasz Klupa .............. 259 Obesity diagnosis and mortality risk based on a body shape -

Endocrine Disrupters, Mahmoud Et Al 2005 for AMINAL 1 Identificatie Van
Identificatie van indicatoren voor impact van endocrien verstorende stoffen /hormonale stoorstoffen (in het Engels) Identification of indicators for the impact of endocrine/hormone disrupting substances Studie uitgevoerd door Universiteit Gent en Katholieke Universiteit Leuven Mahmoud A., Comhaire F., Van Larebeke N. (University Ghent) Van Kersschaever G. (Catholic University Leuven) In opdracht van For AMINAL (Administratie Milieu,- Natuur-, Land- en Waterbeheer) Project number DTG/OL200300064/3185/M&G Endocrine disrupters, Mahmoud et al 2005 for AMINAL 1 Acknowledgments The generous exchange of information by many clinicians and national as well as international organizations has significantly contributed to the realization of this work. We are especially grateful to organizations that follow an open policy and make their data available in an interactive form on their websites such as MINECO and EUROCAT. This facilitated the recalculation of some data for the present work. The authors would like to thank the members of the steering committee for their expert advice and critical comments. The authors Endocrine disrupters, Mahmoud et al 2005 for AMINAL 2 Summary Based on the evidence we gathered on the possible health impacts of endocrine disruption, we generated a list of pathologies possibly related to endocrine disruptors. The availability of medical data on the relevant pathologies in Flanders was then explored through contacts with many organizations and experts. A suggested strategy was developed for the retrieval of these data and linking them to data on environmental pollution. The relevant pathologies were then ranked according to the evidence available and the relevance to the Flemish situation in a descending order of priority (see below). -

Ethnic Differences in Smoking Behaviour: the Situation of Roma in Eastern Europe (Original Research)
Duval L, Wolff FC, McKee M, Roberts B. Ethnic differences in smoking behaviour: The situation of Roma in Eastern Europe (Original research). SEEJPH 2016, posted: 14 December 2016. DOI:10.4119/UNIBI/SEEJPH- 2016-132 ORIGINAL RESEARCH Ethnic differences in smoking behaviour: The situation of Roma in Eastern Europe Laetitia Duval1, François-Charles Wolff2, Martin McKee3, Bayard Roberts3 1 School of Public Health, Imperial College London, Norfolk Place, London W2 1PG, United Kingdom; 2 LEMNA, Université de Nantes, BP 52231 Chemin de la Censive du Tertre, 44322 Nantes Cedex, France and INED, Paris, France; 3 ECOHOST – The Centre for Health and Social Change, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London, United Kingdom. Corresponding author: Laetitia Duval, School of Public Health, Imperial College London; Address: Norfolk Place, London W2 1PG, United Kingdom; E-mail: [email protected] 1 Duval L, Wolff FC, McKee M, Roberts B. Ethnic differences in smoking behaviour: The situation of Roma in Eastern Europe (Original research). SEEJPH 2016, posted: 14 December 2016. DOI:10.4119/UNIBI/SEEJPH- 2016-132 Abstract Aim: To investigate ethnic differences in smoking between Roma and non-Roma and their determinants, including how discrimination faced by Roma may influence smoking decisions. Methods: We analysed data from the Roma Regional Survey 2011 implemented in twelve countries of Central and South-East Europe with random samples of approximately 750 households in Roma settlements and 350 households in nearby non-Roma communities in each country. The overall sample comprises 11,373 individuals (8,234 Roma) with a proportion of women of 57% and an average age of 36 years. -

Closing the Life Expectancy Gap of Roma in Europe Executive Summary
CLOSING THE LIFE EXPECTANCY GAP OF ROMA IN EUROPE EXECUTIVE SUMMARY The European Public Health Alliance (EPHA) is currently undertaking an evidence-based literature review on the Roma life expectancy gap, based on the following indicators: 1. Life expectancy gap between Roma and non-Roma 2. Roma children and infant mortality 3. Determinants of life expectancy The poor state of health in Roma communities is prevalent—and largely ignored—across Europe. Some Roma are completely excluded from health care, while most face hostility and discrimination within healthcare settings. Available literature on Roma and health agrees that: • Roma people suffer from poorer health and unhealthier living conditions compared to majority populations; • better data is needed to explain the Roma health gap and design better interventions to reduce this gap; • the poor health of Roma is closely linked to the social determinants of health¹. Studies have consistently found that Roma health is worse than the health of the majority populations or other ethnic minority groups. Estimated life expectancy for Roma is consistently lower than corresponding national averages. Infant mortality among Roma is estimated to exceed national averages by several percentage points. Roma are less likely to be covered by health insurance. Roma do not appear to enjoy preventive health care on equal footing with non-Roma and instead are more likely to rely on emergency services. Academics and advocates identify inadequate living conditions, poverty, limited education, and pervasive discrimination against Roma by health care professionals and the public as the key reasons for the poor health of Roma². Like all Europeans, Roma represent patients, caregivers, and families. -

Ecologia Balkanica
ECOLOGIA BALKANICA International Scientific Research Journal of Ecology Volume 4, Issue 1 June 2012 UNION OF SCIENTISTS IN BULGARIA – PLOVDIV UNIVERSITY OF PLOVDIV PUBLISHING HOUSE ii International Standard Serial Number Print ISSN 1314-0213; Online ISSN 1313-9940 Aim & Scope „Ecologia Balkanica” is an international scientific journal, in which original research articles in various fields of Ecology are published, including ecology and conservation of microorganisms, plants, aquatic and terrestrial animals, physiological ecology, behavioural ecology, population ecology, population genetics, community ecology, plant-animal interactions, ecosystem ecology, parasitology, animal evolution, ecological monitoring and bioindication, landscape and urban ecology, conservation ecology, as well as new methodical contributions in ecology. Studies conducted on the Balkans are a priority, but studies conducted in Europe or anywhere else in the World is accepted as well. Published by the Union of Scientists in Bulgaria – Plovdiv and the University of Plovdiv Publishing house – twice a year. Language: English. Peer review process All articles included in “Ecologia Balkanica” are peer reviewed. Submitted manuscripts are sent to two or three independent peer reviewers, unless they are either out of scope or below threshold for the journal. These manuscripts will generally be reviewed by experts with the aim of reaching a first decision as soon as possible. The journal uses the double anonymity standard for the peer-review process. Reviewers do not have to sign their reports and they do not know who the author(s) of the submitted manuscript are. We ask all authors to provide the contact details (including e-mail addresses) of at least four potential reviewers of their manuscript. -
2012 All Rights Reserved to the Editor
E U R O P E A N E X H I B I T I O N O F C R E A T I V I T Y A N D I N N O V A T I O N 22001122 ISBN: 978‐973‐703‐759‐6 Editor: Eng. Andrei‐Victor SANDU Graphics & text: Eng. Andrei‐Victor SANDU Copyright © 2012 All Rights reserved to the Editor All the patents and researches information are provided by the authors. No major correction were applied by editor. Gheorghe Asachi Technical University of Iasi The Gheorghe Asachi Technical University of Iasi (TU IASI) has the oldest tradition in the engineering field of education in Romania. In 1813 the scholar Gheorghe Asachi established the first school for surveyors and civil engineers considered to be the nucleus of the technical higher education in Iasi. Currently, the Gheorghe Asachi Technical University of Iasi has 11 faculties and 4 departments that offer educational and doctoral programmes for more than 17000 students in 61 engineering specializations, 73 Master of Science programs and 10 doctoral schools. Besides its educational mission, the Gheorghe Asachi Technical University of Iasi has an important research dimension, having 21 accredited centers and laboratories for scientific research. These centers activate in different fields, within national and international research grants, research contracts with industry or governmental organizations, their activities placing our university in the Romanian top of scientific research. The constant focus on interdisciplinary research, on innovation and knowledge transfer, as well the quality of the research staff and their commitment for excellence provided a constant dynamics of research activities and the recognition and visibility of our university. -

Spatial Differences and Temporal Changes in Illicit Drug Use in Europe Quantified by Wastewater Analysis
UvA-DARE (Digital Academic Repository) Spatial differences and temporal changes in illicit drug use in Europe quantified by wastewater analysis Ort, C.; van Nuijs, A.L.N.; Berset, J.-D.; Bijlsma, L.; Castiglioni, S.; Covaci, A.; de Voogt, P.; Emke, E.; Fatta-Kassinos, D.; Griffiths, P; Hernández, F.; González-Mariño, I.; Grabic, R.; Kasprzyk-Hordern, B.; Mastroianni, N; Meierjohann, A.; Nefau, T.; Östman, M.; Pico, Y.; Racamonde, I; Reid, M.; Slobodnik, J.; Terzic, S.; Thomaidis, N; Thomas, K.V. DOI 10.1111/add.12570 Publication date 2014 Document Version Final published version Published in Addiction Link to publication Citation for published version (APA): Ort, C., van Nuijs, A. L. N., Berset, J-D., Bijlsma, L., Castiglioni, S., Covaci, A., de Voogt, P., Emke, E., Fatta-Kassinos, D., Griffiths, P., Hernández, F., González-Mariño, I., Grabic, R., Kasprzyk-Hordern, B., Mastroianni, N., Meierjohann, A., Nefau, T., Östman, M., Pico, Y., ... Thomas, K. V. (2014). Spatial differences and temporal changes in illicit drug use in Europe quantified by wastewater analysis. Addiction, 109(8), 1338-1352. https://doi.org/10.1111/add.12570 General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material UvA-DAREinaccessible is a serviceand/or provided remove by it the from library the of website. -

Health Deprivation Among Roma in the Western Balkans
Health deprivation among Roma in the Western Balkans New evidence on the social, economic and environmental determinants of health among marginalised Roma populations Health deprivation among Roma - UNDP 2018 Health deprivation 1 Roma Inclusion series This publication was prepared with support from the European Union © United Nations Development Programme (UNDP), 2018 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in all forms by any means, mechanical, photocopying, recording or otherwise prior permission. Cover photo: UNDP Cover design and layout: Ikromjon Mamadov The content of this publication can in no way be taken to reflect the view of UNDP or the European Union. To be cited as: Nikoloski, Z., Marnie, S. (2018). Health deprivation among Roma in the Western Balkans: New evidence on the social, economic and environmental determinants of health among marginalised Roma populations Table of contents 1. INTRODUCTION AND SUMMARY .................................................................................................................. 1 2. LITERATURE REVIEW .................................................................................................................................... 4 2.1. Roma self-rated health .............................................................................................................................. 4 2.2. Access to healthcare ................................................................................................................................. -

Strony Redakcyjne Nowe.Qxd
ACTA POLONIAE PHARMACEUTICA VOL. 71 No. 1 January/February 2014 ISSN 0001-6837 Drug Research EDITOR Aleksander P. Mazurek National Medicines Institute, The Medical University of Warsaw ASSISTANT EDITOR Jacek Bojarski Medical College, Jagiellonian University, KrakÛw EXECUTIVE EDITORIAL BOARD Miros≥awa Furmanowa The Medical University of Warsaw Boøenna Gutkowska The Medical University of Warsaw Roman Kaliszan The Medical University of GdaÒsk Jan Pachecka The Medical University of Warsaw Jan Pawlaczyk K. Marcinkowski University of Medical Sciences, PoznaÒ Janusz Pluta The Medical University of Wroc≥aw Witold Wieniawski Polish Pharmaceutical Society, Warsaw Pavel Komarek Czech Pharmaceutical Society Henry Ostrowski-Meissner Charles Sturt University, Sydney Erhard Rˆder Pharmazeutisches Institut der Universit‰t, Bonn Phil Skolnick DOV Pharmaceutical, Inc. Zolt·n Vincze Semmelweis University of Medicine, Budapest This Journal is published bimonthly by the Polish Pharmaceutical Society (Issued since 1937) The paper version of the Publisher magazine is a prime version. Starting from volume 71, issue no. 2/2014, the journal Acta Poloniae Pharmaceutica - Drug Research will be published exclusively in an electronic version. This version can be found in the Internet on page www.actapoloniaepharmaceutica.pl An access to the journal in its electronic version is free of charge. Impact factor (2013): 0.665 MNiSW score (2013): 15 points Index Copernicus (2012): 13.18 Cited in: Chemical Abstracts, International Pharmaceutical Abstracts, EMBASE/Excerpta Medica, Index Medicus, MEDLINE Science Citation Index Expanded Journal Citation Reports/Sci. Ed., Derwent Drug File Typeset by RADIUS, Warszawa; Printed by Oficyna Wydawniczo-Poligraficzna, Zπbki Acta Poloniae Pharmaceutica ñ Drug Research Volume 71, Number 1 January/February 2014 CONTENTS REVIEW 3. -

PUSHED to the WASTELANDS Environmental Racism Against Roma Communities in Central and Eastern Europe
PUSHED TO THE WASTELANDS Environmental racism against Roma communities in Central and Eastern Europe 1 Authors Patrizia Heidegger (EEB) Katy Wiese (EEB) Report available online at www.eeb.org/library/pushed-to-the-wastelands How to cite this report Heidegger, P.; and Wiese, K. (2020). Pushed to the wastelands: Environmental racism against Roma communities in Central and Eastern Europe. Brussels: European Environmental Bureau Report produced and disseminated by European Environmental Bureau (eeb.org) ERGO network (ergonetwork.org) In cooperation with Environmental Science and Technology Institute at the Universitat Autònoma de Barcelona (ICTA-UAB) Editor responsible Jeremy Wates Researchers Ksenija Hanaček and Federico Demaria (ICTA-UAB) European Environmental Bureau (EEB) Radost Zaharieva (Bulgaria) Rue des Deux Eglises 14-16 Mustafa Asanovski (North Macedonia) Brussels, Belgium Ciprian-Valentin Nodis (Romania) +32 (0)2 289 1090 Florin Botonogu (Romania) [email protected] Zsuzsanna Kovács (Hungary) Ondrej Poduska (Slovakia) An International non-profit Association Association Internationale sans but lucratif Acknowledgements EC transparency register number We would like to thank everyone else who has 06798511314-27 contributed to this report in various ways: Marek Szilvasi (Open Society Foundations) Design Joan Martinez-Alier and Daniela Del Bene (ICTA-UAB) Gemma Bowcock (EEB) Nick Meynen, Khaled Diab and Richard Filčák (EEB) Printing Beelzepub (beelzepub.com) The responsibility for errors remains with the authors. Printed in Brussels on 100%