Public Health Situation Analysis (PHSA) – Long-Form
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
For Free Distribution
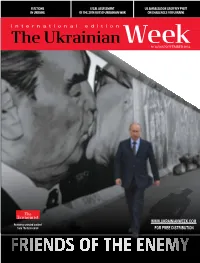
ELECTIONS LeGAL ASSESSMENT US AMBASSADOR GeOFFREY PYATT IN UKRAINE OF THE 2014 RuSSO-UKRAINIAN WAR ON CHALLENGES FOR UKRAINE № 14 (80) NOVEMBER 2014 WWW.UKRAINIANWEEK.COM Featuring selected content from The Economist FOR FREE DISTRIBUTION |CONTENTS BRIEFING Lobbymocracy: Ukraine does not have Rapid Response Elections: The victory adequate support in the West, either in of pro-European parties must be put political circles, or among experts. The to work toward rapid and irreversible situation with the mass media and civil reforms. Otherwise it will quickly turn society is slightly better into an equally impressive defeat 28 4 Leonidas Donskis: An imagined dialogue on several clichés and misperceptions POLITICS 30 Starting a New Life, Voting as Before: Elections in the Donbas NEIGHBOURS 8 Russia’s gangster regime – the real story Broken Democracy on the Frontline: “Unhappy, poorly dressed people, 31 mostly elderly, trudged to the polls Karen Dawisha, the author of Putin’s to cast their votes for one of the Kleptocracy, on the loyalty of the Russian richest people in Donetsk Oblast” President’s team, the role of Ukraine in his grip 10 on power, and on Russia’s money in Europe Poroshenko’s Blunders: 32 The President’s bloc is painfully The Bear, Master of itsT aiga Lair: reminiscent of previous political Russians support the Kremlin’s path towards self-isolation projects that failed bitterly and confrontation with the West, ignoring the fact that they don’t have a realistic chance of becoming another 12 pole of influence in the world 2014 -

National Coordination Meeting
National Coordination Meeting Kyiv, 20 January 2021 Business of the Day 1. Q&A on Health Reform. Guest speakers: • Dr. Elina Dale, Adviser on Health Policy at WHO Ukraine • Anastasiya Brylova, Officer on Service Delivery, WHO Ukraine 2. Health Cluster Calendar 2021 3. Situation update: COVID-19 and ECA - WHO & partners 4. Update on Public Health Situation Analysis (PHSA) and ongoing assessments 5. Health Cluster M&E Framework 6. AOB • Update on Q4 2020 HRP and COVID-19 reporting • Update on COVID-19 Distribution Planning Tool (4W) • Health Cluster Assessment Database Health Cluster Meeting Q&A on Health Reform in Ukraine Dr. Elina Dale, Adviser on Health Policy Anastasiya Brylova , Officer on Service Delivery WHO Ukraine 2. HС Calendar Q1 & Q2 2021 # Month Date Q&A topics (TBC) 1 January 20 Health reform HeRAMS, Attacks on Health 2 February 3 Facilities 3 February 17 IPC & WASH 4 March 3 MHPSS 5 March 17 HIV/TB 6 April 14 Laboratories 7 April 28 Field focus: GCA & NGCA 8 May 12 Post COVID Rehab Human Rights/Protection and 9 May 26 Health 10 June 2 Epi and Surveillance 11 June 9 Behavioral Insights 12 June 16 Comms in Health 4. Public Health Situation Analysis (PHSA) • PHSA is part of the Public Health Information Services (PHIS) tools of the Global Health Cluster. • Provides all health sector partners with a common and comprehensive understanding of the public health situation in a crisis in order to inform evidence-based collective humanitarian health response planning. Focus of the assessment: Donetska & Luhanska Oblasts Eastern Ukraine -
![English.Pdf Purchasing Power Parity [PPP])—Much Lower Than 2 World Bank](https://docslib.b-cdn.net/cover/2888/english-pdf-purchasing-power-parity-ppp-much-lower-than-2-world-bank-1082888.webp)
English.Pdf Purchasing Power Parity [PPP])—Much Lower Than 2 World Bank
CENTRAL Public Disclosure Authorized AFRICAN REPUBLIC ECONOMIC Public Disclosure Authorized UPDATE FOURTH EDITION Investing in Public Disclosure Authorized Human Capital to Protect the Future JULY 2021 Public Disclosure Authorized © 2021 The World Bank 1818 H Street NW, Washington DC 20433 Telephone: 202-473-1000; Internet: www.worldbank.org Some rights reserved This work is a product of the staff of The World Bank. The findings, interpretations, and conclusions expressed in this work do not necessarily reflect the views of the Executive Directors of The World Bank or the governments they represent. The World Bank does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgment on the part of The World Bank concerning the legal status of any territory or the endorsement or acceptance of such boundaries. Rights and Permissions The material in this work is subject to copyright. Because The World Bank encourages dissemination of its knowledge, this work may be reproduced, in whole or in part, for noncommercial purposes as long as full attribution to this work is given. Attribution—Please cite the work as follows: “World Bank. 2021. Central African Republic Economic Update: Investing in Human Capital to Protect the Future. © World Bank.” All queries on rights and licenses, including subsidiary rights, should be addressed to World Bank Publications, The World Bank Group, 1818 H Street NW, Washington, DC 20433, USA; fax: 202-522-2625; -

State Building in Revolutionary Ukraine
STATE BUILDING IN REVOLUTIONARY UKRAINE Unauthenticated Download Date | 3/31/17 3:49 PM This page intentionally left blank Unauthenticated Download Date | 3/31/17 3:49 PM STEPHEN VELYCHENKO STATE BUILDING IN REVOLUTIONARY UKRAINE A Comparative Study of Governments and Bureaucrats, 1917–1922 UNIVERSITY OF TORONTO PRESS Toronto Buffalo London Unauthenticated Download Date | 3/31/17 3:49 PM © University of Toronto Press Incorporated 2011 Toronto Buffalo London www.utppublishing.com Printed in Canada ISBN 978-1-4426-4132-7 Printed on acid-free, 100% post-consumer recycled paper with vegetable- based inks. Library and Archives Canada Cataloguing in Publication Velychenko, Stephen State building in revolutionary Ukraine: a comparative study of governments and bureaucrats, 1917–1922/Stephen Velychenko. Includes bibliographical references and index. ISBN 978-1-4426-4132-7 1. Ukraine – Politics and government – 1917–1945. 2. Public adminstration – Ukraine – History – 20th century. 3. Nation-building – Ukraine – History – 20th century 4. Comparative government. I. Title DK508.832.V442011 320.9477'09041 C2010-907040-2 The research for this book was made possible by University of Toronto Humanities and Social Sciences Research Grants, by the Katedra Foundation, and the John Yaremko Teaching Fellowship. This book has been published with the help of a grant from the Canadian Federation for the Humanities and Social Sciences, through the Aid to Scholarly Publications Programme, using funds provided by the Social Sciences and Humanities Research Council of Canada. University of Toronto Press acknowledges the fi nancial assistance to its publishing program of the Canada Council for the Arts and the Ontario Arts Council. University of Toronto Press acknowledges the fi nancial support of the Government of Canada through the Canada Book Fund for its publishing activities. -

CRIMEAN ALBUM: Stories of Human Rights Defenders IRYNA VYRTOSU CRIMEAN ALBUM: STORIES of HUMAN RIGHTS DEFENDERS УДК 342.72/.73(477.75-074)(092) К82
IRYNA VYRTOSU CRIMEAN ALBUM: Stories Of Human Rights Defenders IRYNA VYRTOSU CRIMEAN ALBUM: STORIES OF HUMAN RIGHTS DEFENDERS УДК 342.72/.73(477.75-074)(092) К82 Author of text: Iryna Vyrtosu. Editor and author of idea: Tetiana Pechonchyk. Production photographer: Valeriya Mezentseva. Photographers: Mykola Myrnyi, Iryna Kriklya, Olexiy Plisko, as well as photos from the personal archives of the heroes. Transcription of the interviews: Yana Khmelyuk. Translator: Olga Lobastova. Proofreader: Arthur Rogers. Design composition and layout: Pavlo Reznikov. I. Vyrtosu К82 Crimean Album: Stories of Human Rights Defenders / I. Vyrtosu; edit. Т. Pechonchyk; Human Rights Information Centre. – Kyiv: KBC, 2019. – 232 p. ISBN 978-966-2403-16-9 This book contains evidence and memories of Crimean human rights defenders including their work experience before and after the occupation. There are twenty personal stories about the past, present and future of people, who continue to fight for the protection of human rights in Crimea even after losing their home, as well as those, who oppose reprisals living under the occupation. These are stories of Olga Anoshkina, Eskender Bariyev, Mykhailo Batrak, Oleksandra Dvoretska, Abdureshyt Dzhepparov, Lilia Hemedzhy, Sergiy Zayets, Synaver Kadyrov, Emil Kurbedinov, Alyona Luniova, Roman Martynovsky, Ruslan Nechyporuk, Valentyna Potapova, Anna Rassamakhina, Daria Svyrydova, Olga Skrypnyk and Vissarion Aseyev, Iryna Sedova and Oleksandr Sedov, Tamila Tasheva, Maria Sulialina, Volodymyr Chekryhin. The book is intended -

Kerch Strait En Route to the Ukrainian Port of Berdyansk, on the Sea of Azov, According to Official Ukrainian and Russian Reports (See Figure 1)
CRS INSIGHT Russia's Use of Force Against the Ukrainian Navy December 3, 2018 (IN11004) | Related Author Cory Welt | Cory Welt, Analyst in European Affairs ([email protected], 7-0530) Naval Incident Escalates Tensions On November 25, 2018, Russian coast guard vessels in the Black Sea forcibly prevented two small Ukrainian armored artillery boats and a tugboat from transiting the Kerch Strait en route to the Ukrainian port of Berdyansk, on the Sea of Azov, according to official Ukrainian and Russian reports (see Figure 1). After ramming the tugboat and blockading all three boats for hours, the Russian vessels reportedly fired on them as they sought to leave the area, injuring six sailors. The Ukrainian boats and their 24 crew members were detained and taken to Kerch, in the Russian-occupied Ukrainian region of Crimea. The sailors were arrested and placed in pretrial detention on charges of illegally crossing what Russia refers to as its state border (i.e., the territorial waters around occupied Crimea). Observers generally viewed the incident as a major escalation of tensions between Russia and Ukraine. Russia Tightens Control In May 2018, Russian President Vladimir Putin opened a new 12-mile-long bridge linking Russia to Crimea over the Kerch Strait, the waterway connecting the Black Sea to the Sea of Azov. The bridge was designed to accommodate an existing shipping lane, but it imposes new limits on the size of ships that transit the strait. Observers note that since the bridge's opening, Russia has stepped up its interference with commercial traffic traveling to and from Ukrainian ports in Mariupol and Berdyansk, which export steel, grain, and coal. -

Constitution of Ukraine
CONSTITUTION OF UKRAINE Adopted at the Fifth Session of the Verkhovna Rada of Ukraine on June 28, 1996 Amended by the Laws of Ukraine № 2222-IV dated December 8, 2004, № 2952-VI dated February 1, 2011, № 586-VII dated September 19, 2013, № 742-VII dated February 21, 2014, № 1401-VIII dated June 2, 2016 № 2680-VIII dated February 7, 2019 The Verkhovna Rada of Ukraine, on behalf of the Ukrainian people - citizens of Ukraine of all nationalities, expressing the sovereign will of the people, based on the centuries-old history of Ukrainian state-building and on the right to self-determination realised by the Ukrainian nation, all the Ukrainian people, providing for the guarantee of human rights and freedoms and of the worthy conditions of human life, caring for the strengthening of civil harmony on Ukrainian soil, and confirming the European identity of the Ukrainian people and the irreversibility of the European and Euro-Atlantic course of Ukraine, striving to develop and strengthen a democratic, social, law-based state, aware of responsibility before God, our own conscience, past, present and future generations, guided by the Act of Declaration of the Independence of Ukraine of August 24, 1991, approved by the national vote on December 1, 1991, adopts this Constitution - the Fundamental Law of Ukraine. Chapter I General Principles Article 1 Ukraine is a sovereign and independent, democratic, social, law-based state. Article 2 The sovereignty of Ukraine extends throughout its entire territory. Ukraine is a unitary state. The territory of Ukraine within its present border is indivisible and inviolable. Article 3 The human being, his or her life and health, honour and dignity, inviolability and security are recognised in Ukraine as the highest social value. -
Assessments of Health Services Availability in Humanitarian Emergencies: a Review of Assessments in Haiti and Sudan Using a Health Systems Approach Jason W
Nickerson et al. Conflict and Health (2015) 9:20 DOI 10.1186/s13031-015-0045-6 RESEARCH ARTICLE Open Access Assessments of health services availability in humanitarian emergencies: a review of assessments in Haiti and Sudan using a health systems approach Jason W. Nickerson1,2,3*, Janet Hatcher-Roberts3, Orvill Adams4, Amir Attaran5 and Peter Tugwell3,6 Abstract Background: Assessing the availability of health services during humanitarian emergencies is essential for understanding the capacities and weaknesses of disrupted health systems. To improve the consistency of health facilities assessments, the World Health Organization has proposed the use of the Health Resources Availability Mapping System (HeRAMS) developed in Darfur, Sudan as a standardized assessment tool for use in future acute and protracted crises. This study provides an evaluation of HeRAMS’ comprehensiveness, and investigates the methods, quality and comprehensiveness of health facilities data and tools in Haiti, where HeRAMS was not used. Methods and findings: Tools and databases containing health facilities data in Haiti were collected using a snowball sampling technique, while HeRAMS was purposefully evaluated in Sudan. All collected tools were assessed for quality and comprehensiveness using a coding scheme based on the World Health Organization’s health systems building blocks, the Global Health Cluster Suggested Set of Core Indicators and Benchmarks by Category, and the Sphere Humanitarian Charter and Minimum Standards in Humanitarian Response. Eight assessments and databases were located in Haiti, and covered a median of 3.5 of the 6 health system building blocks, 4.5 of the 14 Sphere standards, and 2 of the 9 Health Cluster indicators. -

Public Opinion Survey of Residents of Ukraine
Public Opinion Survey of Residents of Ukraine December 13-27, 2018 Methodology • The survey was conducted by Rating Group Ukraine on behalf of the International Republican Institute’s Center for Insights in Survey Research. • The survey was conducted throughout Ukraine (except for the occupied territories of Crimea and Donbas) from December 13- 27, 2018, through face-to-face interviews at respondents’ homes. • The sample consisted of 2,400 permanent residents of Ukraine aged 18 and older and eligible to vote. It is representative of the general population by gender, age, region, and settlement size. The distribution of population by regions and settlements is based on statistical data of the Central Election Commission from the 2014 parliamentary elections, and the distribution of population by age and gender is based on data from the State Statistics Committee of Ukraine from January 1, 2018. • A multi-stage probability sampling method was used with the random route and “last birthday” methods for respondent selection. • Stage One: The territory of Ukraine was split into 25 administrative regions (24 regions of Ukraine and Kyiv). The survey was conducted throughout all regions of Ukraine, with the exception of the occupied territories of Crimea and Donbas. • Stage Two: The selection of settlements was based on towns and villages. Towns were grouped into subtypes according to their size: • Cities with populations of more than 1 million • Cities with populations of between 500,000-999,000 • Cities with populations of between 100,000-499,000 • Cities with populations of between 50,000-99,000 • Cities with populations of up to 50,000 • Villages Cities and villages were selected by the PPS method (probability proportional to size). -

Humanitarian Needs Overview Iraq Issued November 2019
HUMANITARIAN HUMANITARIAN PROGRAMME CYCLE 2020 NEEDS OVERVIEW ISSUED NOVEMBER 2019 IRAQ 1 HUMANITARIAN NEEDS OVERVIEW 2020 About Get the latest updates This document has been consolidated by OCHA on behalf of the Humanitarian OCHA coordinates humanitarian action to ensure Country Team and partners. It provides a shared understanding of the crisis, crisis-affected people receive the assistance and protection they need. It works to overcome obstacles including the most pressing humanitarian needs and the estimated number of that impede humanitarian assistance from reaching people who need assistance. It represents a consolidated evidence base and helps people affected by crises, and provides leadership in inform joint strategic response planning. mobilizing assistance and resources on behalf of the The designations employed and the presentation of material in the report do not imply humanitarian system. the expression of any opinion whatsoever on the part of the Secretariat of the United www.unocha.org/iraq Nations concerning the legal status of any country, territory, city or area or of its www.twitter.com/ochairaq authorities, or concerning the delimitation of its frontiers or boundaries. PHOTO ON COVER Meeting with women displaced by flooding in April 2019, Maysan, © A Lazau-Ratz, OCHA Humanitarian Response aims to be the central website for Information Management tools and services, enabling information exchange between clusters and IASC members operating within a protracted or sudden onset crisis. www.humanitarianresponse.info/iraq Humanitarian InSight supports decision-makers by giving them access to key humanitarian data. It provides the latest verified information on needs and delivery of the humanitarian response as well as financial contributions. -

Russia's Use of Force Against the Ukrainian Navy
INSIGHTi Russia’s Use of Force Against the Ukrainian Navy December 3, 2018 Naval Incident Escalates Tensions On November 25, 2018, Russian coast guard vessels in the Black Sea forcibly prevented two small Ukrainian armored artillery boats and a tugboat from transiting the Kerch Strait en route to the Ukrainian port of Berdyansk, on the Sea of Azov, according to official Ukrainian and Russian reports (see Figure 1). After ramming the tugboat and blockading all three boats for hours, the Russian vessels reportedly fired on them as they sought to leave the area, injuring six sailors. The Ukrainian boats and their 24 crew members were detained and taken to Kerch, in the Russian-occupied Ukrainian region of Crimea. The sailors were arrested and placed in pretrial detention on charges of illegally crossing what Russia refers to as its state border (i.e., the territorial waters around occupied Crimea). Observers generally viewed the incident as a major escalation of tensions between Russia and Ukraine. Russia Tightens Control In May 2018, Russian President Vladimir Putin opened a new 12-mile-long bridge linking Russia to Crimea over the Kerch Strait, the waterway connecting the Black Sea to the Sea of Azov. The bridge was designed to accommodate an existing shipping lane, but it imposes new limits on the size of ships that transit the strait. Observers note that since the bridge’s opening, Russia has stepped up its interference with commercial traffic traveling to and from Ukrainian ports in Mariupol and Berdyansk, which export steel, grain, and coal. Russian authorities reportedly have imposed delays at the bridge and conducted inspections of vessels. -

UKL) #461 Compiled by Dominique Arel Chair of Ukrainian Studies, U of Ottawa 3 December 2013
The Ukraine List (UKL) #461 compiled by Dominique Arel Chair of Ukrainian Studies, U of Ottawa www.ukrainianstudies.uottawa.ca 3 December 2013 1-New York Times: Ukrainian Government Survives Confidence Vote 2-Washington Post: Ukraine Doesn’t Need Another Revolution 3-Financial Times: EU Should Punish Officials Complicit in Violence 4-Serhiy Kudelia: Ukraine’s Perfect Storm: How Far Will It Go? (Ponars) 5-Anders Aslund: Euro Revolution in Ukraine 6-Anna Abakunova: Mobilisation from Above in Dnipropetrovsk 7-Anton Shekhovtsov: On the Provocation near the Presidential Administration 8-Andreas Umland: Time to Abolish the Elected Presidency 9-Oleh Kotsyuba, Ukraine's Battle for Europe (New York Times) 10-Ivan Katchanovski: On Violence (FB) 11-The Economist: Day of the Gangster Pygmy 12-Statement by Foreign Ministers Sikorski and Bildt of Poland and Sweden 13-Washington Post: Freedom House on Targeted Sanctions 14-Foreign Policy: Anders Aslund, The Basket Case **Mychailo Wynnyckyj’s EuroMaidan Diary** 15-2 December: The Thug Speaks 16-1 December: Ukraine’s Revolution 17-30 November: It’s Getting Ugly **Thanks to Anna Abakunova, Anders Aslund, David Johnson, Mikhailo Minakov, Andreas Umland, Mychailo Wynnyckyj, and Roman Zurba** #1 Ukrainian Government Survives Confidence Vote By David Herszenhorn New York Times, 3 December 2013 KIEV, Ukraine — As protesters continued their siege of government buildings and occupation of a landmark plaza in this rattled capital, President Viktor F. Yanukovich survived a no-confidence vote on Tuesday after some lawmakers demanded the resignation of the government. The measure failed as members of the majority Party of Regions stood by Mr.