Vision Screening Training
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jaeger Eye Chart
Jaeger Eye Chart DIRECTIONS FOR USE The Jaeger eye chart (or Jaeger card) is used to test and document near visual acuity at a normal reading distance. Refractive errors and conditions that cause blurry reading vision include astigmatism, hyperopia (farsightedness) and presbyopia (loss of near focusing ability after age 40). If you typically wear eyeglasses or contact lenses full-time, you should wear them during the test. 1. Hold the test card 14 inches from the eyes. Use a tape measure to verify this distance. 2. The card should be illuminated with lighting typical of that used for comfortable reading. 3. Testing usually is performed with both eyes open; but if a significant difference between the two eyes is suspected, cover one eye and test each eye separately. 4. Go to the smallest block of text you feel you can see without squinting, and read that passage aloud. 5. Then try reading the next smaller block of text. (Remember: no squinting!) 6. Continue reading successively smaller blocks of print until you reach a size that is not legible. 7. Record the “J” value of the smallest block of text you can read (example: “J1”). DISCLAIMER: Eye charts measure only visual acuity, which is just one component of good vision. They cannot determine if your eyes are “working overtime” (needing to focus more than normal, which can lead to headaches and eye strain). Nor can they determine if your eyes work properly as a team for clear, comfortable binocular vision and accurate depth perception. Eye charts also cannot detect serious eye problems such as glaucoma or early diabetic retinopathy that could lead to serious vision impairment and even blindness. -

Strabismus, Amblyopia & Leukocoria
Strabismus, Amblyopia & Leukocoria [ Color index: Important | Notes: F1, F2 | Extra ] EDITING FILE Objectives: ➢ Not given. Done by: Jwaher Alharbi, Farrah Mendoza. Revised by: Rawan Aldhuwayhi Resources: Slides + Notes + 434 team. NOTE: F1& F2 doctors are different, the doctor who gave F2 said she is in the exam committee so focus on her notes Amblyopia ● Definition Decrease in visual acuity of one eye without the presence of an organic cause that explains that decrease in visual acuity. He never complaints of anything and his family never noticed any abnormalities ● Incidence The most common cause of visual loss under 20 years of life (2-4% of the general population) ● How? Cortical ignorance of one eye. This will end up having a lazy eye ● binocular vision It is achieved by the use of the two eyes together so that separate and slightly dissimilar images arising in each eye are appreciated as a single image by the process of fusion. It’s importance 1. Stereopsis 2. Larger field If there is no coordination between the two eyes the person will have double vision and confusion so as a compensatory mechanism for double vision the brain will cause suppression. The visual pathway is a plastic system that continues to develop during childhood until around 6-9 years of age. During this time, the wiring between the retina and visual cortex is still developing. Any visual problem during this critical period, such as a refractive error or strabismus can mess up this developmental wiring, resulting in permanent visual loss that can't be fixed by any corrective means when they are older Why fusion may fail ? 1. -

Updates on Myopia
Updates on Myopia A Clinical Perspective Marcus Ang Tien Y. Wong Editors Updates on Myopia Marcus Ang • Tien Y. Wong Editors Updates on Myopia A Clinical Perspective Editors Marcus Ang Tien Y. Wong Singapore National Eye Center Singapore National Eye Center Duke-NUS Medical School Duke-NUS Medical School National University of Singapore National University of Singapore Singapore Singapore This book is an open access publication. ISBN 978-981-13-8490-5 ISBN 978-981-13-8491-2 (eBook) https://doi.org/10.1007/978-981-13-8491-2 © The Editor(s) (if applicable) and The Author(s) 2020, corrected publication 2020 Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifc statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

AAO 2018 2019 BCSC Sectio
The American Academy of Ophthalmology is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. The American Academy of Ophthalmology designates this enduring material for a maximum of 15 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. CME expiration date: June 1, 2021. AMA PRA Category 1 Credits™ may be claimed only once between June 1, 2018, and the expiration date. BCSC® volumes are designed to increase the physician’s ophthalmic knowledge through study and review. Users of this activity are encouraged to read the text and then answer the study questions provided at the back of the book. To claim AMA PRA Category 1 Credits™ upon completion of this activity, learners must demonstrate appropriate knowledge and participation in the activity by taking the posttest for Section 3 and achieving a score of 80% or higher. For further details, please see the instructions for requesting CME credit at the back of the book. The Academy provides this material for educational purposes only. It is not intended to represent the only or best method or procedure in every case, nor to replace a physician’s own judgment or give specic advice for case management. Including all indications, contraindications, side eects, and alternative agents for each drug or treatment is beyond the scope of this material. All information and recommendations should be veried, prior to use, with current information included in the manufacturers’ package inserts or other independent sources, and considered in light of the patient’s condition and history. -
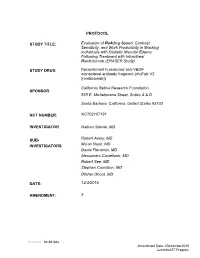
PROTOCOL STUDY TITLE: Evaluation of Reading Speed
PROTOCOL STUDY TITLE: Evaluation of ReAding Speed, Contrast Sensitivity, and Work Productivity in Working Individuals with Diabetic Macular Edema Following Treatment with Intravitreal Ranibizumab (ERASER Study) STUDY DRUG Recombinant humanized anti-VEGF monoclonal antibody fragment (rhuFab V2 [ranibizumab]) California Retina Research Foundation SPONSOR 525 E. Micheltorena Street, Suites A & D Santa Barbara, California, United States 93103 NCT NUMBER: NCT02107131 INVESTIGATOR Nathan Steinle, MD SUB- Robert Avery, MD INVESTIGATORS Ma’an Nasir, MD Dante Pieramici, MD Alessandro Castellarin, MD Robert See, MD Stephen Couvillion, MD Dilsher Dhoot, MD DATE: 12/4/2015 AMENDMENT: 3 Protocol: ML29184s Amendment Date: 4December2015 Lucentis IST Program 1. BACKGROUND 1.1 PATHOPHYSIOLOGY Diabetic retinopathy is the leading cause of blindness associated with retinal vascular disease. Macular edema is a major cause of central vision loss in patients presenting with diabetic retinopathy. The prevalence of diabetic macular edema after 15 years of known diabetes is approximately 20% in patients with type 1 diabetes mellitus (DM), 25% in patients with type 2 DM who are taking insulin, and 14% in patients with type 2 DM who do not take insulin. Breakdown of endothelial tight junctions and loss of the blood-retinal barrier between the retinal pigment epithelium and choriocapillaris junction lead to exudation of blood, fluid, and lipid leading to thickening of the retina. When these changes involves or threatens the fovea, there is a higher risk of central vision loss. Functional and eventual structural changes in the blood-retinal barrier as well as reduced retinal blood flow leads to the development of hypoxia. These changes may result in upregulation and release of vascular endothelial growth factor (VEGF), a 45 kD glycoprotein. -

Care of the Patient with Accommodative and Vergence Dysfunction
OPTOMETRIC CLINICAL PRACTICE GUIDELINE Care of the Patient with Accommodative and Vergence Dysfunction OPTOMETRY: THE PRIMARY EYE CARE PROFESSION Doctors of optometry are independent primary health care providers who examine, diagnose, treat, and manage diseases and disorders of the visual system, the eye, and associated structures as well as diagnose related systemic conditions. Optometrists provide more than two-thirds of the primary eye care services in the United States. They are more widely distributed geographically than other eye care providers and are readily accessible for the delivery of eye and vision care services. There are approximately 36,000 full-time-equivalent doctors of optometry currently in practice in the United States. Optometrists practice in more than 6,500 communities across the United States, serving as the sole primary eye care providers in more than 3,500 communities. The mission of the profession of optometry is to fulfill the vision and eye care needs of the public through clinical care, research, and education, all of which enhance the quality of life. OPTOMETRIC CLINICAL PRACTICE GUIDELINE CARE OF THE PATIENT WITH ACCOMMODATIVE AND VERGENCE DYSFUNCTION Reference Guide for Clinicians Prepared by the American Optometric Association Consensus Panel on Care of the Patient with Accommodative and Vergence Dysfunction: Jeffrey S. Cooper, M.S., O.D., Principal Author Carole R. Burns, O.D. Susan A. Cotter, O.D. Kent M. Daum, O.D., Ph.D. John R. Griffin, M.S., O.D. Mitchell M. Scheiman, O.D. Revised by: Jeffrey S. Cooper, M.S., O.D. December 2010 Reviewed by the AOA Clinical Guidelines Coordinating Committee: David A. -

Screening for Visual Impairment in Children Ages 1–5 Years: Update for the USPSTF
Screening for Visual Impairment in Children Ages 1–5 Years: Update for the USPSTF AUTHORS: Roger Chou, MD,a,b,c Tracy Dana, MLS,a and abstract Christina Bougatsos, BSa CONTEXT: Screening could identify preschool-aged children with vi- aOregon Evidence-Based Practice Center and Departments of bMedicine and cMedical Informatics and Clinical Epidemiology, sion problems at a critical period of visual development and lead to Oregon Health & Science University, Portland, Oregon treatments that could improve vision. KEY WORDS OBJECTIVE: To determine the effectiveness of screening preschool- impaired visual acuity, vision screening, vision tests, preschool aged children for impaired visual acuity on health outcomes. children, refractive errors, amblyopia, amblyogenic risk factors, random dot E stereoacuity test, MTI photoscreener, patching, METHODS: We searched Medline from 1950 to July 2009 and the Co- systematic review chrane Library through the third quarter of 2009, reviewed reference ABBREVIATIONS lists, and consulted experts. We selected randomized trials and con- USPSTF—US Preventive Services Task Force trolled observational studies on preschool vision screening and treat- logMAR—logarithmic minimal angle of resolution ALSPAC—Avon Longitudinal Study of Parents and Children ments, and studies of diagnostic accuracy of screening tests. One in- RR—relative risk vestigator abstracted relevant data, and a second investigator CI—confidence interval checked data abstraction and quality assessments. VIP—Vision in Preschoolers PLR—positive likelihood ratio RESULTS: Direct evidence on the effectiveness of preschool vision NLR—negative likelihood ratio screening for improving visual acuity or other clinical outcomes re- MTI—Medical Technology and Innovations OR—odds ratio mains limited and does not adequately address whether screening is D—diopter(s) more effective than no screening. -

Ocular Rotations and the Hirschberg Test
Pacific University CommonKnowledge College of Optometry Theses, Dissertations and Capstone Projects 3-1-1977 Ocular rotations and the Hirschberg test A John Carter Pacific University Recommended Citation Carter, A John, "Ocular rotations and the Hirschberg test" (1977). College of Optometry. 448. https://commons.pacificu.edu/opt/448 This Thesis is brought to you for free and open access by the Theses, Dissertations and Capstone Projects at CommonKnowledge. It has been accepted for inclusion in College of Optometry by an authorized administrator of CommonKnowledge. For more information, please contact [email protected]. Ocular rotations and the Hirschberg test Abstract The Hirschberg test is an objective means of determining the angle of strabismus by noting the distance the corneal reflex of a light source is from the center of the entrance pupil. A scale factor is used in converting the amount the reflex distance is in millimeters ot prism diopters. Recent studies have demonstrated this factor to be 22 prism diopters for each millimeter. This study notes how axial length would effect this scale factor. Using ultrasound axial lengths of thirty eyes were measured and compared to the results of a Hirschberg simulation. A small effect results from this comparison. The mean values of scale factor determination noted twenty-three prism diopters per millimeter. Degree Type Thesis Degree Name Master of Science in Vision Science Committee Chair Niles Roth Subject Categories Optometry This thesis is available at CommonKnowledge: https://commons.pacificu.edu/opt/448 Copyright and terms of use If you have downloaded this document directly from the web or from CommonKnowledge, see the “Rights” section on the previous page for the terms of use. -

Strabismus: a Decision Making Approach
Strabismus A Decision Making Approach Gunter K. von Noorden, M.D. Eugene M. Helveston, M.D. Strabismus: A Decision Making Approach Gunter K. von Noorden, M.D. Emeritus Professor of Ophthalmology and Pediatrics Baylor College of Medicine Houston, Texas Eugene M. Helveston, M.D. Emeritus Professor of Ophthalmology Indiana University School of Medicine Indianapolis, Indiana Published originally in English under the title: Strabismus: A Decision Making Approach. By Gunter K. von Noorden and Eugene M. Helveston Published in 1994 by Mosby-Year Book, Inc., St. Louis, MO Copyright held by Gunter K. von Noorden and Eugene M. Helveston All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without prior written permission from the authors. Copyright © 2010 Table of Contents Foreword Preface 1.01 Equipment for Examination of the Patient with Strabismus 1.02 History 1.03 Inspection of Patient 1.04 Sequence of Motility Examination 1.05 Does This Baby See? 1.06 Visual Acuity – Methods of Examination 1.07 Visual Acuity Testing in Infants 1.08 Primary versus Secondary Deviation 1.09 Evaluation of Monocular Movements – Ductions 1.10 Evaluation of Binocular Movements – Versions 1.11 Unilaterally Reduced Vision Associated with Orthotropia 1.12 Unilateral Decrease of Visual Acuity Associated with Heterotropia 1.13 Decentered Corneal Light Reflex 1.14 Strabismus – Generic Classification 1.15 Is Latent Strabismus -

New-Onset-Right-Hypertropia.Pdf
New-Onset Right Hypertropia: A Sequela of Inflammatory Orbital Pseudotumor I. Case Hx: A 45 year old African American male presents as a walk-in with a new vertical deviation of his right eye. He reports slow onset over the past six months, gradually worsening. He notes constant vertical diplopia. He denies eye pain. His comprehensive eye exam six months earlier was unremarkable. No vertical deviation was noted. A mild prescription was released for distance and near. Medical conditions include carpal tunnel, osteoarthritis, and poorly controlled Type 2 diabetes mellitus with a fluctuating HbA1c. He has a history of Bell’s Palsy affecting the right side of his face, but the condition has been resolved for fifteen years without recurrence. The patient is currently taking metformin and tramadol for joint pain. II. Pertinent findings: The patient was afebrile without nausea or fatigue. No recent illnesses were noted. Clinical examination indicated a vertical hypertropia OD greater than 40 prism diopters. Pupils were normal. EOMs indicated incomplete depression OD in downgaze and slight abduction limitations OD. CVFs were full to finger counting OD, OS. Hertel exophthalmometry was 30 OD, 25 OS. Color vision was normal. On slit lamp exam, 2-3+ periorbital edema OD was noted without tenderness. There was 2+ conjunctival chemosis with trace injection OD. No follicles or papillae were noted. The patient’s left eye was completely uninvolved. No anterior chamber reaction was noted OD,OS, and IOP was 23 mmHg OD, 18 mmHg OS. Upon dilated examination, all posterior health was unremarkable. No nerve edema or abnormalities were noted OD or OS. -

The Paediatric Ophthalmic Examination Examination of a Child’S Eye Can Be Challenging and Traumatic but Could Save the Child’S Sight Or Even His Life
The paediatric ophthalmic examination Examination of a child’s eye can be challenging and traumatic but could save the child’s sight or even his life. A du Bruyn,1 MB ChB, Dip (Ophth), FC (Ophth); D Parbhoo,2 MB ChB, FC (Ophth) 1Consultant Ophthalmologist, St Aidan’s Hospital, University of KwaZulu-Natal, Durban, South Africa 2Consultant Ophthalmologist, Parklands Hospital and Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa Correspondence to: A du Bruyn ([email protected]) Twenty-ve thousand children in South • proptosis • 1 - 2 years: A child should be able to Africa are blind, mainly because of • ptosis pick up hundreds and thousands with congenital cataracts, congenital glaucoma, • epiphora ease (dierent size sweets can be used). malignant tumours (retinoblastoma), • buphthalmos or microphthalmos Teller’s and Cardi acuity cards can be retinopathy of prematurity, inammation • red eyes used. and injuries. Strabismus, amblyopia and • cloudy cornea • 2 - 3 years: At this age they can name refractive errors cause many more children • pupil abnormalities pictures and any of the picture charts to have reduced vision. Unfortunately, half • leucocoria. can be used (Kay pictures, Allen’s picture of these children who go blind will die cards, Bailey-Hall). Hundreds and within 2 years, mainly due to accidents. Visual assessment thousands may still be useful. Visual milestones • 3 - 5 years: Matching optotypes (use Fiy per cent of childhood blindness can be A child’s vision is developing and to establish the illiterate E chart, Landolt’s C test, prevented by early detection and treatment, visual acuity in a child is challenging for Sheridan- Gardener’s test, Lea charts). -

20-OPHTHALMOLOGY Cataract-Ds Brushfield-Down Synd Christmas
20-OPHTHALMOLOGY cataract-ds BrushfielD-Down synd christmas tree-myotonic dystrophy coronaRY-pubeRtY cuneiform-cortical(polyopia) cupuliform-post subcapsular(max vision loss) Elschnig pearl, ring of Soemmering-after(post capsule) experimenTal-Tyr def glassworker-infrared radiation grey(soft), yellow, amber, red(cataracta rubra), brown(cataracta brunescence), black(cat nigrans)(GYARBB)-nuclear(hard) heat-ionising radiation Membranous-HallerMan Streiff synd morgagnian-hypermature senile oildrop(revers)-galactossemia(G1PUT def) post cortical/bread crumb/polychromatic lustre/rainbow-complicated post polar-PHPV(persistent hyperplastic prim vitreous) radiational-post subcapsular riders-zonular/lamellar(vitD def, hypoparathy) roseTTe(ant cortex)-Trauma, concussion shield-atopic dermatitis snowstorm/flake-juvenile DM(aldose reductase def, T1>T2, sorbitol accumulat) star-electrocution sunflower/flower of petal-Wilson ds, chalcosis, penetrating trauma syndermatotic-atopic ds total-cong rubella zonular-galactossemia(galactokinase def) stage of cataract lamellar separation incipient/intumescence(freq change of glass) immature mature hypermature Aim4aiims.inmorgagnian sclerotic lens layer ant capsule ant epithelium lens fibre[66%H2O, 34%prot-aLp(Largest), Bet(most aBundant), γ(crystalline, soluble)] nucleus embryonic(0-3mthIUL) fetal(3-8mthIUL)-Y shape(suture) infantile(8mthIUL-puberty) adult(>puberty) cortex post capsule thinnest-post pole>ant pole thickest, most active cell-equator vitA absent in lens vitC tpt in lens by myoinositol H2O tpt in lens