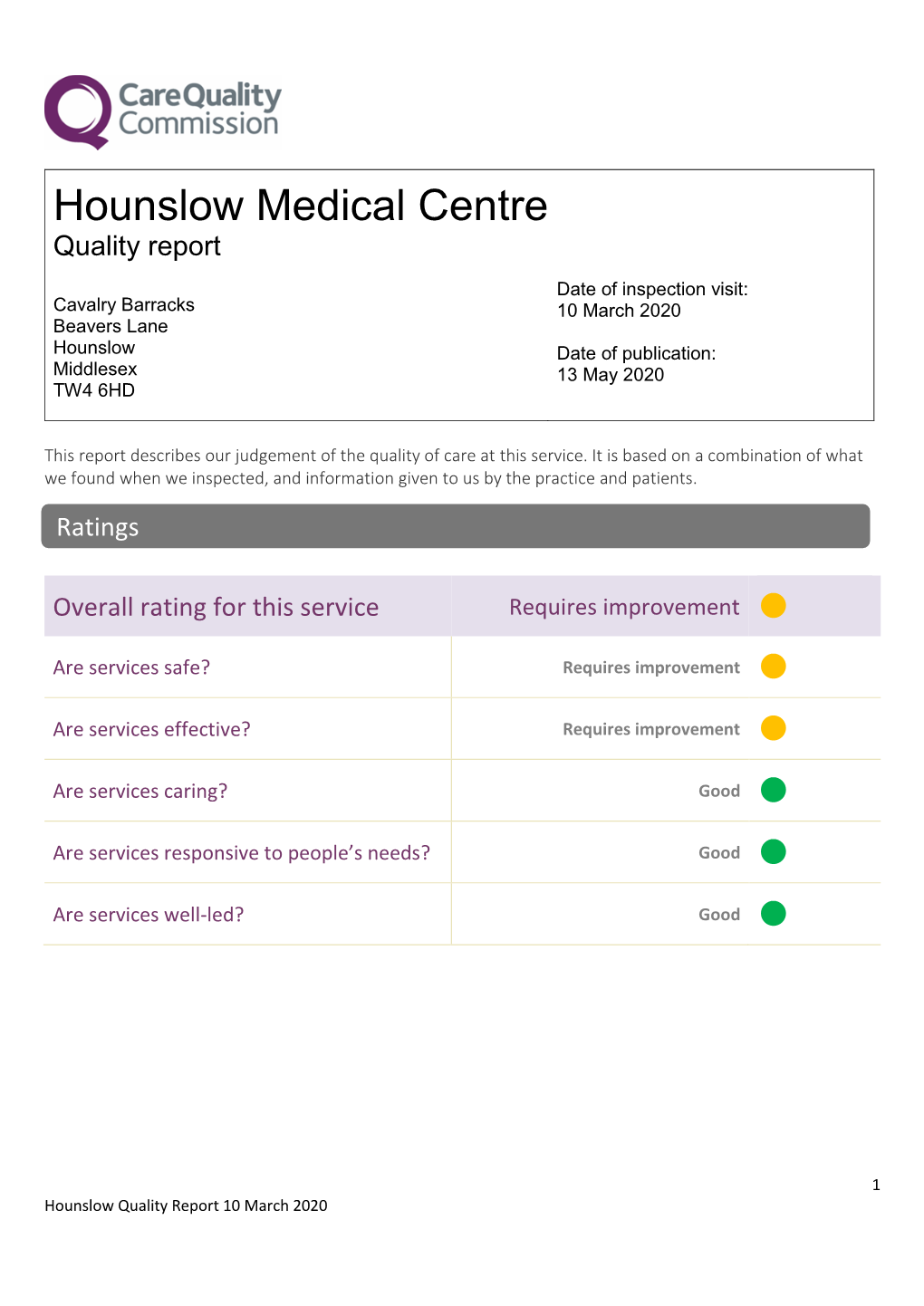
Hounslow Medical Centre: Requires Improvement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

History of the Aldershot Branch, Rsa
HISTORY OF THE ALDERSHOT BRANCH, RSA Edition 2, June 2020 The author acknowledges with grateful thanks the considerable help received in compiling the military history content of this update. Paul Vickers, Chairman, Friends of the Aldershot Military Museum, generously provided much detailed information on Aldershot Garrison aspects. The story of the formation of C Troop was drawn from the research work of branch member, David Mullineaux, written up in the Royal Signals Institution Journal of Spring 2010. Branch Committee Member, Neville Lyons not only provided the lists of events and talks but also proof read the whole document and made valued suggestions on presentation. Historical Background There has been a strong link between Aldershot and the evolution of modern Army signalling ever since the establishment of the first Royal Engineers Telegraph Troop there in 1871. As the technology developed, so did the number of units both in Aldershot and worldwide with the result that at the end of the Great War there were 70,000 men serving in the Royal Engineers Signal Service. This led in 1920 to the formation of the Royal Corps of Signals which has maintained a continuous link with the Town and Garrison of Aldershot to this day. The full story of this evolutionary process is set out in a further new paper entitled “Aldershot: the Cradle of Army Signalling.” The technical and organisational details given there are separate from the history of the Association branch but there is a connection between the two stories which was particularly close in the early years of Royal Signals because of the units and individuals involved. -

JK 2019 Event Programme (Rev 4
WELCOME! OUR START TIMES Name Day 1 Day 2 Day 3 JAN KJELLSTRÖM INTERNATIONAL FESTIVAL 2019 EVENT PROGRAMME (incorporating World Ranking Event Bulletin 2) 19th - 22nd APRIL WELCOME! The South Central Orienteering Association welcomes competitors from across the UK and around the world to the 52nd Jan Kjellström International Festival of Orienteering in the South of England. Date Format Location Postcode OS Grid Ref. Friday 19/04/2019 Sprint Race Aldershot Garrison GU11 2JL SU869525 TrailO TempO Aldershot Garrison GU11 2JL SU869525 Saturday 20/04/2019 Middle Distance Windmill Hill GU16 6ST SU908586 TrailO PreO Mytchett (East) (off B3012 road) SU922562 Sunday 21/04/2019 Long Distance Cold Ash RG18 9XP SU519737 Monday 22/04/2019 Relays Minley GU17 9UF SU827577 JK 2019 Event Programme (Rev 4. 6th April 2019) Page 1 General Information General Information Emergency phone number +44 7597 055256 Hospitals The nearest hospitals with Accident and Emergency departments are: Journey for serious injury Miles (min) Journey for minor injury Miles (min) Day 1 to Frimley Park Hospital 5 miles Day 1 to Frimley Park Hospital 5 miles (9 mins) GU16 7UJ (9 mins) Day 2 to Frimley Park Hospital 3.4 miles Day 2 to Frimley Park Hospital 3.4 miles (12 mins) GU16 7UJ (12 mins) Woking Walk in Centre (8am-8pm) 10.6 miles ( 25 mins) GU22 7HS Day 3 to Royal Berkshire 23 miles Day 3 to W Berks Community Hospital 5.7 miles Hospital Craven Road, (35 mins) (8am-10pm) RG18 3AS (15 mins) Reading, Berkshire, RG1 5AN Day 4 to Frimley Park Hospital 4.3 miles Day 4 to Frimley Park Hospital 4.3 miles (10 mins) GU16 7UJ (10mins) Bracknell Urgent Care Centre (8am- 13 miles (20 mins) 8pm) RG12 9TR First Aid First Aid is provided on all days by The Response Group. -

List of British Army Garrisons and Installations in the UK and Abroad
'''''''''''''''' '''''''''' ''''''''''''''''''''''''' Army Personnel Centre '''''''''' ''''''''''' ''''''''' Kentigern House 65 Brown Street GLASGOW G2 8EX Ref: FOI2018/03121 E-mail: [email protected] ''''''' ''''''''''''''''''''''' ''''' '''''' ''''''''''''''' '''''' 20 March 2018 '''''''''''''''''''''''''''''''''''''''''''''''''''''''''' Dear ''''''' '''''' Thank you for your email of 28 February requesting the following information: Could you provide the list of British Army Garrisons/Installations in the UK and abroad besides London District which have Garrison Sergeant Majors? I am treating your correspondence as a request for information under the Freedom of Information Act 2000 (FOIA). The information you require is shown at Annex A. If you have any queries regarding the content of this letter, please contact this office in the first instance. If you wish to complain about the handling of your request, or the content of this response, you can request an independent internal review by contacting the Information Rights Compliance team, Ground Floor, MOD Main Building, Whitehall, SW1A 2HB (e-mail CIO- [email protected]). Please note that any request for an internal review should be made within 40 working days of the date of this response. If you remain dissatisfied following an internal review, you may raise your complaint directly to the Information Commissioner under the provisions of Section 50 of the Freedom of Information Act. Please note that the Information Commissioner will not normally investigate your case until the MOD internal review process has been completed. The Information Commissioner can be contacted at: Information Commissioner’s Office, Wycliffe House, Water Lane, Wilmslow, Cheshire, SK9 5AF. Further details of the role and powers of the Information Commissioner can be found on the Commissioner's website at https://ico.org.uk/. -

Hampshire Link
HAMPSHIRE LINK JANUARY 1, 2015 CHARITY NO 219279 ‘Improvised’ then … commemorated now Hopefully, during 2014, the centenary of the outbreak of the First World War was commemorated nationally and locally in a measured and tasteful manner. In Hampshire branches staged concerts and special events, held memorial services and laid wreaths and crosses in memory of men from their own towns and villages who had laid down their lives during The Great War. In Aldershot, the home of the British Army, there were two significant events, both bringing together the garrison and the community and both focussing on football. Shahid Azeem, Chairman of Aldershot Town Football Club, described the Peace and Goodwill Concert staged at the ESS Ground on December 4 as, “a bringing together of the military town and the civilian town to commemorate the spontaneous game of football played at Christmas in 1914.” A dramatisation of the game, now referred to as ‘The Truce Game’, formed just part of a remarkable evening of ca rols and readings that proved to be a true union of the town and it’s Army. Thirteen days later an even larger crowd lined the terraces of Aldershot Town’s ground to witness a remarkable football match that spoke volumes for the present day relationship between the two major combatants of the First World War. The ‘Game of Truce’ Commemorative Match pitched the British Army XI against a side representing the German Armed Forces. It proved to be an exciting, highly competitive, evenly matched game; hugely enjoyed by everyone in the 2,547 crowd. -

Rushmoor Connections Issue 76 the Newsletter of Rushmoor Voluntary Services
Spring 2018 Rushmoor Connections Issue 76 The Newsletter of Rushmoor Voluntary Services Now that the clocks have moved forward and the evenings are drawing out, we look forward to some positive things happening in Rushmoor: SATURDAY, 14TH APRIL 2018—10.00 A.M. Curly Bridge/Moor Road area— Rushmoor Spring Clean. Come and help us get the Brook and the surrounding area ready for people to enjoy in the better weather. Lots of litter picking! Meet at: Curly Bridge at the top of Cheyne Way, Farnborough GU14 8RZ ALL WELCOME Rowhill Nature Reserve Birds, Bugs and Roundabouts, by Professor Simon Leather Thursday, 10th May 2018 7.30 p.m. to 9.00 p.m. The Field Centre, Cranmore Lane, Aldershot GU11 3BD Free to members, £2 non-members Page 2 R.V.S News Rushmoor Voluntary Services Staff Greg Alexander Chief Executive Sue Hathaway Development Officer Viv Walker Administrative Support Manager Terry Snuggs Volunteer Centre Co-ordinator Hazel Chant Lead Project Support Worker Suzie Wright Project Support Worker and RVS Admin. Pam Hammond RVS Home Help Operations Co-ordinator Sue Chadwick RVS Home Help Administration Co-ordinator Rachel Thomas Transport Organiser, Rushmoor & Hart Caroline Colwill Transport Scheduler/Administrator Tracy Bowden Service Manager - Community Access Project Mike Frost Community Mental Health Worker (part time) Dial-A-Ride Drivers Age Concern Driver, Thursday and Peter Hyde Friday Lunch Club Nick Molloy David Buckler Fleet Link Tony Thomas Paul Roberts During the recent bouts of snow, we were not able to run our Dial-a-Ride and Fleet Link transport services and our Home Help service was at a reduced level. -

Soldiers, Migrants and Citizens – the NEPALESE in BRITAIN
Soldiers, Migrants and Citizens – THE NEPALESE IN BRITAIN A RUNNYMEDE COMMUNITY STUDY BY JESSICA MAI SIMS SOLDIERS, MIGRANTS AND CITIZENS – THE NEPALESE IN BRITAIN About Runnymede Community Studies In reflecting on the changing nature of ethnic diversity in Britain, it becomes increasingly clear that we have to move beyond binary notions of white and non-white to explain the ways in which racisms operate, identities are formed and people live out their lives. The societies in which we live are becoming more diverse and will continue to diversify as migration patterns change, and the impacts of globalization are reflected in labour markets as well as in transnational movement of capital. This series of community studies aims to promote understanding of the diversity within and between different ethnic groups. Our intention is to build up a collection of studies which focus on communities; their demography, links to civil society, and key political and social issues. We hope that over time this will provide a rich resource for understanding how diversity is lived and experienced away from the necessarily crude ethnic monitoring form, in a vital and dynamic multi- ethnic society. To find out more about the Runnymede Community Studies series, please visit: www.runnymedetrust.org ISBN-13: 978-1-906732-09-7 (online only) EAN: 9781906732097 (online only) Published by Runnymede in August 2008 in electronic version only, this document is copyright © 2008 the Runnymede Trust. Reproduction of this report by printing, photocopying or electronic means for non-commercial purposes is permitted. Otherwise, it is not permitted to store or transmit the electronic version of this report, nor to print, scan or photocopy any paper version for dissemination or commercial use, without the prior permission of the publisher. -

Raoc Apprentice College Junior Leaders Regiment Raoc & Rct
RAOC ENLISTED BOYS’ & BOYS’ SCHOOL RAOC JUNIOR LEADERS BATTALION RAOC & REME RAOC APPRENTICE COLLEGE JUNIOR LEADERS REGIMENT RAOC & RCT Contents Page • Introduction and Welcome – From the Chairman, Editor and Committee members • Warning Order - Next Reunion (3rd Bi-Annual Reunion) in 2010 • Membership Update – Membership: From strength to strength • Items for Sale – Ex-Boys' Association Wall Shields - CD of the Edinburgh Tattoo of Aug 1961 • General Information – REME Association – National Archives (RCT) – eBay Treasures! • General Information – Combat Stress – An article on this Charitable Organisation • Newsletter Article – Paul Bunker former RAOC Junior Leader and SAS soldier, KIA in 1982 • Old Codgers’ Photo Gallery - Lost Pals – Last Post – Christmas Message - Admin Team Introduction and Welcome Dear Members, A very warm welcome from our Founder and Chairman Paul Jones, all your Association Committee Members who work behind the lines, George Tether, Bill Chamberlain, Dave McCarthy, Brian Wild, Allan Jones and lastly, me the Editor of the Ex-Boys’ Association Newsletter, Adrian Hayward-Wills, to the Twelfth Ex-Boys' Association and Winter Edition Newsletter for 2009. We hope that this Twelfth Newsletter finds you well and looking forward to Christmas and to reading articles on The Junior Drum Major and his Mace and an interesting article submitted by Ex-Boy and Association Member, Peter Roberts on his experience as a Bugler on the BBC show talent show know as “Top Town”. And lastly, an article on former RAOC Junior Leader, Paul Bunker, who was KIA in the Falklands War of 1982, as an SAS Corporal. As you know, it is our intention to produce two Newsletters (Summer and Winter) per annum, with a publication in June and December of each year. -

Dear Review Officer, I'm Writing a Follow Up, from My Email I Sent You
From: Stephen Dawson Sent: 20 February 2011 21:22 To: Reviews@ Subject: The Review Officer (Rushmoor) Dear Review Officer, I'm writing a follow up, from my email i sent you on the 13th of February, about Aldershot Garrison( North Camp), which is currently in St Marks ward Farnborough. And how i think it should form a new Aldershot Ward, which would link Aldershot Garrison to its Home Town of Aldershot. Aldershot Town Centre is the main place for Aldershot Garrison R & R, sharing its Leisure and Recreation facilities with Military & Civilian's. From Pubs, Clubs & Cinema to Restaurant's & Shopping. And the Military is the reason for Aldershot Town centres existence, as the Home Town of The British Army. Aldershot Town Centre is also where the Garrisons Home Coming Parades and Anniversaries Parades are held. Some links about some of the parades are below. http://www.gethampshire.co.uk/news/s/2072882_homecoming_parade_for_aldershot_ troops http://www.gethampshire.co.uk/news/s/2062007 crowds welcome soldiers home to _aldershot http://www.gethampshire.co.uk/news/s/36931_parade_celebrates_anniversary Aldershot still has a Military Pub, evidence of Military presence and Business's in Town Centre. link to website below; http://www.airborne-forces.com/traf.html The Garrison Church is in Wellington Ward. Aldershot Centre for Health has a whole floor dedicated to the Military. I have attached a file of where i think a Aldershot Garrison Ward should be, which the boundary is coloured blue. Lychford Road is the top boundary going down Government House Road, then following Farnborough Airport boundary. Then bottom boundary following Alisions Road, which will be the boundary between Aldershot Garrison and Aldershot Urban extension. -

The Army Schoolmaster and the Development of Elementary Education in the Army, 1812-1920
THE ARMY SCHOOLMASTER AND THE DEVELOPMENT OF ELEMENTARY EDUCATION IN THE ARMY, 1812-1920 by ELAINE ANN SMITH Submitted in accordance with the requirements for the Doctor of Philosophy, Institute of Education, University of London 1 ABSTRACT THE ARMY SCHOOLMASTER AND THE DEVELOPMENT OF ELEMENTARY EDUCATION IN THE ARMY, 1812-1920 It may appear to be somewhat incongruous that the Army, whose primary funct i on has been to prepare for war, shou 1d have been one of the earliest advocates of organized elementary education. Yet its i mpo rtance is someth i ng the Army has long recogn i zed. Soon after the Restoration in 1660, and perhaps even before, some regiments engaged masters to instruct their soldiers and also their offspring. Over the next 150 years an increasing number of command i ng offi cers appoi nted a su i tab 1e NCO to act as schoolmaster to the regiment, before the reforms of 1812 compelled them to do so. In 1846 civilians also became eligible to enlist as Army schoolmasters. Together they became members of the Corps of Army Schoolmasters which survived for nearly three-quarters of a century. This the sis con sid e r s the r ole 0 f the Army s c h0 0 1rna s t e r , his training and conditions of service, with particular reference to the period 1812 to 1920. Although not a comparative study it notes, where relevant, developments in the field of civilian elementary education. It does not consider the Army schoolmi stress, who taught the infants, except when her work impinges upon that of the schoolmaster; this subject has been the focus of another study. -

Surrey Heath Functional Economic Area Analysis
Surrey Heath Functional Economic Area Analysis Draft Report Client: Surrey Heath Borough Council October 2014 Berkshire House 252-256 Kings Road, Reading RG1 4HP T: 0118 938 0940 M: 07881 348 244 E: [email protected] Wessex Economics Ltd Berkshire House 252-256 Kings Road Reading RG1 4HP T: 0118 938 0940 Contact: [email protected] Table of Contents Executive Summary.............................................................................................................................................................................1 1. About this Report .......................................................................................................................................................................... 4 2. The Geography of Surrey Heath and the Blackwater Valley ......................................................................................................... 8 3. Employment in Surrey Heath and the Blackwater Valley ........................................................................................................... 14 4. The Functional Commercial Property Market Area .................................................................................................................... 17 5. The Functional Labour Market Area ........................................................................................................................................... 22 6. Industry Clusters ........................................................................................................................................................................ -

Physical Culture in the Evolution of the British Army, 1860-1920 James Dunbar Campbell
The University of Maine DigitalCommons@UMaine Electronic Theses and Dissertations Fogler Library 2003 "The ra my isn't all work": Physical culture in the evolution of the British army, 1860-1920 James Dunbar Campbell Follow this and additional works at: http://digitalcommons.library.umaine.edu/etd Part of the Military History Commons Recommended Citation Campbell, James Dunbar, ""The ra my isn't all work": Physical culture in the evolution of the British army, 1860-1920" (2003). Electronic Theses and Dissertations. 185. http://digitalcommons.library.umaine.edu/etd/185 This Open-Access Dissertation is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of DigitalCommons@UMaine. "THE ARMY lSh1'1'ALL \VOKK": PHYSICAL CULTURE IN THE EVOLUTION OF THE BRITlSH ARMY, 1860-1920 BY James Dunbar Campbell B.A. Colby College, 1986 M.A. Un~versityof Malne, 1997 A THESIS Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy (Individualized in British History) The Graduate School The University of Maine December, 2003 Advisory Committee: William J. Baker, Professor of History, Advisor Richard Blanke. Professor of History Janet TeBl-ake, Assistant Professor of Ili,s!ory Robert LVhulen. Lecturer in Enylish Da\,id klclxan. t'rol'csso~. ot f listorq. Ki17z.i C'c*llczc 1.o1icl01~ "THE ARMY ISN'T ALL WORK": PHYSICAL CULTURE IN THE EVOLUTION OF THE BRITISH ARMY, 1860-1920 By James D. Campbell Thesis Advisor: Dr. William J. Baker An Abstract of the Thesis Presented in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy (Individualized in British History) December, 2003 Between the Crimean War and the end of WWI the British Army underwent a dramatic change from being an anachronistic and frequently ineffective organization to being perhaps the most professional and highly trained army in the world. -

NAAFI Fund Award List Round 1 March 2021
Grants awarded under the NAAFI Fund 2020/21 March 2021 66 grants totalling £711,707 For publication Name Project Title Grant Amount Project Description Scotland Funding will be used to provide and outdoor, calisthenics training facility, promoting mental and physical wellbeing 39 Engineer Regiment OUTDOOR TRAINING FACILITY £20,000 to the entire military community. The Unit will purchase 16 new mountain bikes and protective equipment for use by all military, MOD civil servants and their families based at Royal Marines 45 Commando Royal Marines 45 Commando RM welfare bikes £15,200 Condor. Funding will be used to provide wellness rooms in four locations in Scotland and NI to give Army Welfare ARMY WELFARE SERVICE NORTH ARMY WELFARE SERVICE Workers a safe and calm area to relax and mentally AREA WELLNESS ROOMS £5,000 process the complex caseloads that they handle. Funding will be used to re-purpose a disused space into a multi-use welfare compound set in a wildflower meadow with grass cut islands for picnics, games and activities for families and soldiers. The 'eco' compound has single access and provides a secure fenced off area allowing children to experience the outdoors freely and HQ 51Bde & HQ Scotland Garrison Activity Compound £10,000 safely. RAF Lossiemouth will promote a greener environment and give more people the opportunity to cycle. By operating a bike bank where individuals can formally hire bikes to commute, explore and exercise, the vision is to Exercise and explore through encourage increased uptake of physical activity whilst RAF Lossiemouth cycling. £13,600 reducing negative impact on the environment.