Better Health in the Borders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Galashiels and Selkirk Almanac and Directory for 1898
UMBRELLAS Re-Covered in One Hour from 1/9 Upwards. All Kinds of Repairs Promptly Executed at J. R. FULTON'S Umbrella Ware- house, 51 HIGH STREET, Galashiels. *%\ TWENTIETH YEAR OF ISSUE. j?St masr Ok Galasbiels and Selkirk %•* Almanac and Directorp IFOIR, X898 Contains a Variety of Useful information, County Lists for Roxburgh and Selkirk, Local Institutions, and a Complete Trade Directory. Price, - - One Penny. PUBLISHED BY JOH3ST ZMZCQ-CTiEiE] INT, Proprietor of the "Scottish Border Record," LETTERPRESS and LITHOGRAPHIC PRINTER, 25 Channel Street, Galashiels. ADVERTISEMENT. NEW MODEL OF THE People's Cottage Piano —^~~t» fj i «y <kj»~ — PATERSON & SONS would draw Special Attention to this New Model, which is undoubtedly the Cheapest and Best Cottage Piano ever offered, and not only A CHEAP PIANO, but a Thoroughly Reliable Instrument, with P. & Sons' Guakantee. On the Hire System at 21s per Month till paid up. Descriptive Price-Lists on Application, or sent Free by Post. A Large Selection of Slightly-used Instruments returned from Hire will be Sold at Great Reductions. Sole Agents for the Steinway and Bechstein Pianofortes, the two Greatest Makers of the present century. Catalogues on Application. PATEESON <Sc SONS, Musicsellers to the Queen, 27 George Street, EDINBURGH. PATERSON & SONS' Tuners visit the Principal Districts of Scotland Quarterly, and can give every information as to the Purchase or Exchanne of Pianofortes. Orders left with John McQueen, "Border Record" Office, Galashiels, shall receive prompt attention. A life V'C WELLINGTON KNIFE POLISH. 1 *™ KKL f W % Prepared for Oakey's Knife-Boards and all Patent Knife- UfgWa^^""Kmm ^"it— I U Clea-iing Machines. -
![[Name of Public Authority]](https://docslib.b-cdn.net/cover/8285/name-of-public-authority-308285.webp)
[Name of Public Authority]
SCOTTISH FIRE AND RESCUE SERVICE GUIDE TO INFORMATION AVAILABLE THROUGH THE MODEL PUBLICATION SCHEME 2013 The Freedom of Information (Scotland) Act 2002 (the Act) requires Scottish public authorities to produce and maintain a publication scheme. Authorities are under a legal obligation to: publish the classes of information that they make routinely available tell the public how to access the information and what it might cost. The Scottish Fire and Rescue Service has adopted the Model Publication Scheme 2013 produced by the Scottish Information Commissioner. The scheme has the Commissioner’s approval until 31 May 2017. You can see this scheme on our website or by contacting us at the address below. The purpose of this Guide to Information is to: allow you to see what information is available (and what is not available) in relation to each class. state what charges may be applied. explain how you can find the information easily. provide contact details for enquiries and to get help with accessing the information. explain how to request information we hold that has not been published. Availability and formats The information we publish through the model scheme is, wherever possible, available on our website. We offer alternative arrangements for people who do not want to, or cannot, access the information online or by inspection at our premises. For example, we can usually arrange to send information to you in paper copy (although there may be a charge for this). Exempt information We will publish the information we hold that falls within the classes of information below. If a document contains information that is exempt under Scotland’s freedom of information laws (for example sensitive personal information or a trade secret), we may remove or redact the information before publication but we will explain why. -

Scottish Borders & the English Lake District
scotland.nordicvisitor.com SCOTTISH BORDERS & THE ENGLISH LAKE DISTRICT ITINERARY DAY 1 DAY 1: EDINBURGH, CAPITAL OF SCOTLAND Welcome to Edinburgh. For an easy and comfortable way to get from Edinburgh Airport to your hotel in the city centre, we are happy to arrange a private transfer for you (optional, at additional cost). After settling in, go out and explore the city. Edinburgh has a long and storied history, so there’s no shortage of UNESCO World Heritage Sites, museums and landmarks to visit. A stroll along the bustling Princes Street, with views over the gardens to the Edinburgh Castle, also makes a nice introduction to the city centre. Spend the night in Edinburgh. Attractions: Edinburgh DAY 2 DAY 2: CROSSING THE BORDER TO ENGLAND‘S LAKE DISTRICT Head for the scenic Scottish Borders area today with its charming old villages and gently rolling hills. On the way you can visit Glenkinchie Distillery and taste its 12-year-old single malt whisky, which was named Best Lowland Single Malt in the 2013 World Whiskies Awards. For a great photo opportunity, don‘t miss a stop at the scenic Scott‘s View, one of the best known lookouts in the southern Scotland! Another suggestion is to visit the area‘s historical abbeys. Perhaps the most famous is the St Mary’s Abbey, also called Melrose Abbey, a partly ruined monastery of the Cistercian order, the first of its kind in Scotland. The ruins make for a hauntingly beautiful sight, especially with moody clouds hanging low overhead. We also recommend a visit to Abbotsford House, the ancestral home of Sir Walter Scott, the famous 19th century novelist and poet, beautifully located on the banks of the River Tweed. -

HMICS Effective Practice Submission
HMICS Effective Practice submission Title Strathclyde Police and Grampian Police Body Worn Video Force Details CI John Laing, Strathclyde Police, CI Nick Topping, Grampian Police What was the problem / Targeting violence and anti-social behaviour is a national operational priority of the issue Scottish Policing Assessment 2011/15 which contributes to the Scottish Government National Outcome “we live our lives safe from crime disorder and danger. It is also a force and local policing priority which features in local authority single outcome agreements and community planning partnership strategies. Renfrewshire was chosen for this initiative as it has a particularly high level of violence and anti-social behaviour and has a number areas of deprivation including Ferguslie Park (ranked 2 in the SIMD 2009) . Its geography also includes rural areas that are not served by fixed site cctv systems and a number of cycle tracks where mobile cctv is ineffective. Northfield/Mastrick in Grampian were similarly chosen for high levels of violence as well as being one of the most socially deprived in the force area. Public space CCTV plays a significant role in the prevention, detection and prosecution of crime (A national strategy for CCTV in Scotland 2011). Research into a previous National pilot of BWV by the Home Office Police and Crime Standards Directorate (Guidance for the Police use of Body Worn Video Devices - July 2007) highlighted some early results in terms of crime reduction and increased public reassurance as well as reductions in paperwork and court attendance from increased guilty pleas associated with the use of this technology. -

NHS Grampian Community Pharmacist Locum Information Pack
NHS Grampian Community Pharmacist Locum Information Pack NHS Grampian Community Pharmacist Locum Information Pack Contents Page No 1. The Pharmacy and Medicines Directorate (P&MD) ......................................... 3 2. Controlled Drug Accountable Officers Team .................................................... 3 3. To Register as a Locum ................................................................................... 3 4. NHS Mail Account ............................................................................................ 3 5. PCR Login ........................................................................................................ 3 6. Community Pharmacy Website ........................................................................ 4 7. Community Pharmacy Services and Associated Patient Group Directions (PGDs)........................................................................................................................ 4 8. Locally Negotiated Services ............................................................................. 8 9. Palliative Care Network .................................................................................. 10 10. Special Preparations and Unlicensed Medicines ........................................... 10 11. Storage of vaccines & refrigerated products .................................................. 11 12. Central Stores - Order Forms ......................................................................... 11 13. Translation Tools .......................................................................................... -
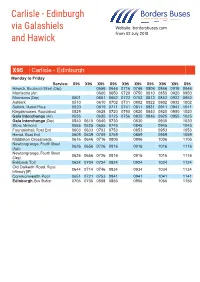
Carlisle - Edinburgh Via Galashiels Website: Bordersbuses.Com and Hawick from 02 July 2018
Carlisle - Edinburgh via Galashiels Website: bordersbuses.com and Hawick From 02 July 2018 X95 Carlisle - Edinburgh Monday to Friday Service: X95 X95 X95 X95 X95 X95 X95 X95 X95 X95 Hawick, Buccleuch Street (Dep) 0556 0646 0716 0746 0806 0846 0916 0946 Morrisons (Arr) 0600 0650 0720 0750 0810 0850 0920 0950 Morrisons (Dep) 0501 0601 0652 0722 0752 0812 0852 0922 0952 Ashkirk 0510 0610 0702 0731 0802 0822 0902 0932 1002 Selkirk, Market Place 0520 0619 0711 0741 0811 0831 0911 0941 1011 Kingsknowes, Roundabout 0529 0628 0720 0750 0820 0840 0920 0950 1020 Gala Interchange (Arr) 0535 0635 0725 0756 0825 0846 0925 0955 1025 Gala Interchange (Dep) 0540 0610 0640 0730 0830 0930 1030 Stow, Memorial 0555 0625 0655 0745 0845 0945 1045 Fountainhall, Road End 0603 0633 0703 0753 0853 0953 1053 Heriot, Road End 0609 0639 0709 0759 0859 0959 1059 Middleton Crossroads 0616 0646 0716 0806 0906 1006 1106 Newtongrange, Fourth Street 0626 0656 0726 0816 0916 1016 1116 (App) Newtongrange, Fourth Street 0626 0656 0726 0816 0916 1016 1116 (Dep) Eskbank Toll 0634 0704 0734 0824 0924 1024 1124 Old Dalkeith Road, Royal 0644 0714 0746 0834 0934 1034 1134 Infirmary [IF] Commonwealth Pool 0651 0721 0753 0841 0941 1041 1141 Edinburgh, Bus Station 0706 0736 0808 0856 0956 1056 1156 X95 Carlisle - Edinburgh Monday to Friday Service:Service: X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 HawickCarlisle, Buccleuch, English St, Street The Courts(Dep) [A] 0855 05560955 0646 07161055 0746 08061155 0846 09161255 0946 MorrisonsKingstown (Arr) Road , -

Galashiels/Coldstream-Newcastle/Metrocentre
Effective From: 04 September 2006 Service GALASHIELS/COLDSTREAM-NEWCASTLE/METROCENTRE 710 Via Galashiels,Darnick,Melrose,Newton St.Boswells,St.Boswells,Kelso,Coldstream,Cornhill,Branxton,Crookham,Milfield,Wooler,Powburn,Glanton,Whittingham,Bridge of Aln,Longframlington,Longhorsley,Morpeth,North Road,Gosforth High Street,North Road,Claremont Road,Queen Victoria Road,St.Thomas' Street.(Certain journeys continue to Metrocentre Coach Park) Wednesday And Satuday Only 710 710 710 W S W * z Coldstream .................................... 0915 0915 ... Wooler........................................... 0945 0945 1625 Powburn......................................... 0955 0955 1635 Glanton.......................................... 1000 1000 ... Whittingham .................................. 1005 1005 ... Longframlington............................. 1020 1020 1655 Longhorsley.................................... 1030 1030 1705 Morpeth ......................................... 1040 1040 ... Northumberland County Hall ......... 1045 1045 ... Gosforth High Street....................... ... 1100 ... Newcastle St.Thomas Street (M)...... 1105 1105 1728 Metrocentre Coach Park ................. ... 1125 ... Operated by: Glen Valley Tours Explanation of codes: : Commences from Galashiels at 0810,via Kelso at 0855. z: Commences from Kelso at 0855 *: Operated by Munros of Jedburgh Certain journeys are secured on your behalf by Northumberland County Council. Effective From: 04 September 2006 Service METROCENTRE/NEWCASTLE-KELSO/GALASHIELS 710 ( Certain journeys -

Compassionate Inverclyde – from the Outcomes Achieved to the Policy Fit, Leadership Considerations and the Approach to Community Engagement
Introduction This report offers insights on various aspects of Compassionate Inverclyde – from the outcomes achieved to the policy fit, leadership considerations and the approach to community engagement. REALISING OUTCOMES AND VALUE Illustrates how the outcomes experienced can be mapped to many local and national outcomes, notably Scotland’s new national performance framework published in 2018 and derivative health and wellbeing outcomes and indicators. It considers the contribution that specific initiatives such as Back Home Boxes and Compassionate Inverclyde as a whole might reasonably be expected to make to specific indicators for readmissions to hospital, delayed discharge from hospital, and the time spent at home or in a homely setting in the last six months of life. This section also notes that the qualities evident in Compassionate Inverclyde are those which have been found to have the most influence on an initiative’s eventual social value. REFLECTIONS ON LEADERSHIP Pulls together reflections on leadership, whether understood as a personal attribute, responsibility or practice, including considerations of the key elements of the multiple leadership philosophies that Compassionate Inverclyde embodies. It presents guiding principles for effective Board engagement and governance and the desired qualities for a Compassionate Community leader. POLICY IN ACTION Some readers will be interested in what Compassionate Inverclyde tells us about the current Scottish policy context. Although it is important to emphasise that Compassionate Inverclyde was not, and is not policy-driven, this section considers the parallels between Compassionate Inverclyde’s community-derived ambitions and Scotland’s national purpose and values. COMMUNITY ENGAGEMENT Provides information about how the practical ideas for kindness and compassionate citizenship taken forward by Compassionate Inverclyde were generated. -
Pocketbook for You, in Any Print Style: Including Updated and Filtered Data, However You Want It
Hello Since 1994, Media UK - www.mediauk.com - has contained a full media directory. We now contain media news from over 50 sources, RAJAR and playlist information, the industry's widest selection of radio jobs, and much more - and it's all free. From our directory, we're proud to be able to produce a new edition of the Radio Pocket Book. We've based this on the Radio Authority version that was available when we launched 17 years ago. We hope you find it useful. Enjoy this return of an old favourite: and set mediauk.com on your browser favourites list. James Cridland Managing Director Media UK First published in Great Britain in September 2011 Copyright © 1994-2011 Not At All Bad Ltd. All Rights Reserved. mediauk.com/terms This edition produced October 18, 2011 Set in Book Antiqua Printed on dead trees Published by Not At All Bad Ltd (t/a Media UK) Registered in England, No 6312072 Registered Office (not for correspondence): 96a Curtain Road, London EC2A 3AA 020 7100 1811 [email protected] @mediauk www.mediauk.com Foreword In 1975, when I was 13, I wrote to the IBA to ask for a copy of their latest publication grandly titled Transmitting stations: a Pocket Guide. The year before I had listened with excitement to the launch of our local commercial station, Liverpool's Radio City, and wanted to find out what other stations I might be able to pick up. In those days the Guide covered TV as well as radio, which could only manage to fill two pages – but then there were only 19 “ILR” stations. -

The Snoot, Roberton, Hawick
The Snoot, Roberton, Hawick Viewing is essential to appreciate this substantial detached two storey property located in a rural location with lovely surrounding views. The building itself has much historical significance. Built as a presbyterian church in 1843, the building was then used as a youth hostel. In recent years it was home to acclaimed guitarist John Renbourn. In need of renovation, the property offers an abundance of possibilities and currently offers ground floor accommodation with a mezzanine level, and small garden to the side. • LARGE LIVING SPACE • OPEN PLAN KITCHEN DINING AREA • SHOWER ROOM • WC • MEZZANINE LEVEL • GARDEN • STUNNING VIEWS • EPC RATING G • OFFERS IN THE REGION OF £85,000 28 High Street, Hawick TD9 9BY T. 0800 1300 353 F. 01450 378 525 E. [email protected] The Town Known for many years as The Queen of the Borders, and situated at the confluence of the Rivers Slitrig and Teviot, Hawick is the largest of the Border towns. Frequent winners of national floral awards, and famous world-wide for its quality knitwear, Hawick is part of The Cashmere Trail and is the major centre for the industry in the Borders. There is a large range of major supermarkets in Sainsburys and Morrisons, a very recently re-built Lidl, an Aldi in construction, and a large Iceland and Farmfoods. A Homebase and Argos are also beneficial to the town, along with a large leisure centre facility for families and kids alike, with many other sports facilities throughout the town. Hawick boasts the award winning Wilton Lodge Park which lies on the River Teviot, and is currently enjoying a £3 million pound regeneration, which includes a new cafeteria and footbridge, together with a new external 3G sports pitch and tennis courts. -

Woodland Building Plot, Timberholme, Bedrule, Near Denholm
Hastings Property Shop 28 The Square Kelso TD5 7HH Telephone 01573 225999 Illustration WOODLAND BUILDING PLOT, TIMBERHOLME, BEDRULE, NEAR DENHOLM A Generous Woodland Plot with Full Planning Consent for Stylish House and Garage in Tucked Away Location Near The Village of Denholm in the Scottish Borders OFFERS AROUND £85,000 www.hastingslegal.co.uk BUILDING PLOT, TIMBERHOLME, BEDRULE, NEAR DENHOLM Prime location building plot extending to approximately ½ an acre with PRICE AND MARKETING POLICY full planning consent for a detached house and garage providing an ideal Offers around £85,000 are invited and should be submitted to the Selling opportunity for a buyer looking to self build in an attractive rural yet Agents, Hastings Property Shop, 28 The Square, Kelso, TD5 7HH, 01573 accessible location. This generous plot lies in a woodland setting on outskirts 225999, Fax 01573 229888. The seller reserves the right to sell at any time of Bedrule in a unique sheltered setting with stunning countryside. and interested parties will be expected to provide the Selling Agents with advice on the source of funds with suitable confirmation of their ability to LOCATION finance the purchase. The plot enjoys a sheltered location in the lee of Ruberslaw approximately a mile south of Bedrule and 3 miles from the much sought after village of Denholm located off the road from Bedrule to Bonchester Bridge. The area is renowned for its beauty with open countryside and excellent walking country on your doorstep. Denholm Village lies a few miles away and has good facilities including a much acclaimed primary school, a superb 18 hole golf course at Minto, good local shops and services and secondary schooling, main supermarkets and larger shops and facilities nearby at Hawick or Jedburgh about 8 miles distant. -

Scottish Borders Child Poverty Index 2019
Scottish Borders Child Poverty Index 2019 May 2020 E.R. Murray for Scottish Borders Council (experimental statistics) Contents SB CPI: Purpose and Scoring ................................................................................................................ 2 Scottish Borders Child Poverty Index 2019 Scores .............................................................................. 6 Comparing Scottish Borders Child Poverty Index 2018 to SIMD 2016 ................................................ 7 Scottish Borders Child Poverty Level Change over Time and by Locality ............................................ 9 Appendix 1: SB CPI 2018 Result for each Data Zone by Best Fit Primary School / Secondary School Catchment .......................................................................................................................................... 10 Berwickshire ................................................................................................................................... 10 Cheviot ........................................................................................................................................... 12 Eildon.............................................................................................................................................. 13 Teviot and Liddesdale .................................................................................................................... 16 Tweeddale .....................................................................................................................................