Producing Enterobacteriaceae in the Routine Laboratory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Review(S) Clinical Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 200327 MEDICAL REVIEW(S) CLINICAL REVIEW Application Type NDA Application Number(s) 200327 Priority or Standard Standard Submit Date(s) December 29, 2009 Received Date(s) December 30, 2009 PDUFA Goal Date October 30, 2010 Division / Office Division of Anti-Infective and Ophthalmology Products Office of Antimicrobial Products Reviewer Name(s) Ariel Ramirez Porcalla, MD, MPH Neil Rellosa, MD Review Completion October 29, 2010 Date Established Name Ceftaroline fosamil for injection (Proposed) Trade Name Teflaro Therapeutic Class Cephalosporin; ß-lactams Applicant Cerexa, Inc. Forest Laboratories, Inc. Formulation(s) 400 mg/vial and 600 mg/vial Intravenous Dosing Regimen 600 mg every 12 hours by IV infusion Indication(s) Acute Bacterial Skin and Skin Structure Infection (ABSSSI); Community-acquired Bacterial Pneumonia (CABP) Intended Population(s) Adults ≥ 18 years of age Template Version: March 6, 2009 Reference ID: 2857265 Clinical Review Ariel Ramirez Porcalla, MD, MPH Neil Rellosa, MD NDA 200327: Teflaro (ceftaroline fosamil) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 9 1.1 Recommendation on Regulatory Action ........................................................... 10 1.2 Risk Benefit Assessment.................................................................................. 10 1.3 Recommendations for Postmarketing Risk Evaluation and Mitigation Strategies ........................................................................................................................ -

Severe Sepsis Tipsheet
Severe Sepsis Tipsheet SEVERE SEPSIS A, B, and C of the following must be met within 6 hours of each other. A. Documentation of a suspected infection. There may be reference to “possible infection,” “suspect infection,” “rule out infection,” or similar documentation. B. TWO or more manifestations of systemic infection according to the Systemic Inflammatory Response Syndrome (SIRS) criteria, which are: • Temperature > 38.3 C or < 36.0 C (> 100.9 F or < 96.8 F) • Heart rate (pulse) > 90 • Respiration > 20 per minute • White blood cell count > 12,000 or < 4,000 or > 10% bands C. Organ dysfunction, evidenced by any one of the following: • Systolic blood pressure (SBP) < 90 mmHg, or mean arterial pressure < 65 mmHg, or a systolic blood pressure decrease of more than 40 mmHg. Physician/APN/PA documentation must be present in the medical record indicating a > 40 mmHg decrease in SBP has occurred and is related to infection, severe sepsis or septic shock and not other causes. • Acute respiratory failure as evidenced by a new need for invasive or non-invasive mechanical ventilation. To use acute respiratory failure as a sign of organ dysfunction there must be: • Documentation of acute respiratory failure AND • Documentation the patient is on mechanical ventilation • Invasive mechanical ventilation requires an endotracheal or tracheostomy tube. Non-invasive mechanical ventilation may be referred to as BiPAP or CPAP. • New need for mechanical ventilation indicates the patient was not using the same type of mechanical ventilation prior to the current acute respiratory failure. • Use the time at which there is documentation the patient has both acute respiratory failure and is on mechanical ventilation. -

Below Are the CLSI Breakpoints for Selected Bacteria. Please Use Your Clinical Judgement When Assessing Breakpoints
Below are the CLSI breakpoints for selected bacteria. Please use your clinical judgement when assessing breakpoints. The lowest number does NOT equal most potent antimicrobial. Contact Antimicrobial Stewardship for drug selection and dosing questions. Table 1: 2014 MIC Interpretive Standards for Enterobacteriaceae (includes E.coli, Klebsiella, Enterobacter, Citrobacter, Serratia and Proteus spp) Antimicrobial Agent MIC Interpretive Criteria (g/mL) Enterobacteriaceae S I R Ampicillin ≤ 8 16 ≥ 32 Ampicillin-sulbactam ≤ 8/4 16/8 ≥ 32/16 Aztreonam ≤ 4 8 ≥ 16 Cefazolin (blood) ≤ 2 4 ≥ 8 Cefazolin** (uncomplicated UTI only) ≤ 16 ≥ 32 Cefepime* ≤ 2 4-8* ≥ 16 Cefotetan ≤ 16 32 ≥ 64 Ceftaroline ≤ 0.5 1 ≥ 2 Ceftazidime ≤ 4 8 ≥ 16 Ceftriaxone ≤ 1 2 ≥ 4 Cefpodoxime ≤ 2 4 ≥ 8 Ciprofloxacin ≤ 1 2 ≥ 4 Ertapenem ≤ 0.5 1 ≥ 2 Fosfomycin ≤ 64 128 ≥256 Gentamicin ≤ 4 8 ≥ 16 Imipenem ≤ 1 2 ≥ 4 Levofloxacin ≤ 2 4 ≥ 8 Meropenem ≤ 1 2 ≥ 4 Piperacillin-tazobactam ≤ 16/4 32/4 – 64/4 ≥ 128/4 Trimethoprim-sulfamethoxazole ≤ 2/38 --- ≥ 4/76 *Susceptibile dose-dependent – see chart below **Cefazolin can predict results for cefaclor, cefdinir, cefpodoxime, cefprozil, cefuroxime axetil, cephalexin and loracarbef for uncomplicated UTIs due to E.coli, K.pneumoniae, and P.mirabilis. Cefpodoxime, cefinidir, and cefuroxime axetil may be tested individually because some isolated may be susceptible to these agents while testing resistant to cefazolin. Cefepime dosing for Enterobacteriaceae ( E.coli, Klebsiella, Enterobacter, Citrobacter, Serratia & Proteus spp) Susceptible Susceptible –dose-dependent (SDD) Resistant MIC </= 2 4 8 >/= 16 Based on dose of: 1g q12h 1g every 8h or 2g every 8 h Do not give 2g q12 Total dose 2g 3-4g 6g NA Table 2: 2014 MIC Interpretive Standards for Pseudomonas aeruginosa and Acinetobacter spp. -

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -

Antibiotic Temocillin Be A
P0840 Could the ‘old’ antibiotic temocillin be a ‘new’ treatment for acute bacterial cholangitis? A retrospective study of 156 cases Sylvain Chawki1, Marion Duprilot1, Gary Taieb1, Veronique Leflon1, Marie-Hélène Nicolas-Chanoine1, Bruno Fantin1, Victoire De Lastours*1 1 Hôpital Beaujon, Assistance Publique Hôpitaux de Paris, Clichy, France Background: Acute cholangitis is a potentially severe infection requiring rapid active antimicrobial therapy. Thus, emergence of multidrug resistant strains of Enterobacteriaceae is a rising global public-health issue. To spare carbapenems, alternative therapies are needed. Temocillin is a narrow-spectrum betalactam targeting almost specifically Enterobacteriaceae, including most isolates resistant to third generation cephalosporin (3GC) and some carbapenemase-producers. Temocillin biliary concentrations may reach several times the blood concentrations. We assessed whether temocillin may represent an alternative treatment for bacterial cholangitis. Materials/methods: In this retrospective monocentric study, all patients from November 2015 to December 2017 admitted for acute cholangitis with a positive culture (blood or bile) were included. Demographic characteristics, severity, treatment and outcome of each episode were collected. Susceptibility to antibiotics, including temocillin, was determined phenotypically. Episodes of cholangitis were considered susceptible to temocillin if all pathogens found were temocillin-susceptible. Results: 137 patients (77/137 male; 56%; median age 67 [60-75]) who suffered 156 episodes of bacterial cholangitis were included (19 patients had 2 separate episodes during the study period). The median Charlson score was 4 [2-8]; 66/137 (48%) were immunocompromised, 54/137 (39%) had a history episode of acute cholangitis. 118/156 (75.6%) episodes were healthcare-associated, 28/156 (18%) required intensive care and 12 (7.7%) were fatal. -

Management of Penicillin and Beta-Lactam Allergy
Management of Penicillin and Beta-Lactam Allergy (NB Provincial Health Authorities Anti-Infective Stewardship Committee, September 2017) Key Points • Beta-lactams are generally safe; allergic and adverse drug reactions are over diagnosed and over reported • Nonpruritic, nonurticarial rashes occur in up to 10% of patients receiving penicillins. These rashes are usually not allergic and are not a contraindication to the use of a different beta-lactam • The frequently cited risk of 8 to 10% cross-reactivity between penicillins and cephalosporins is an overestimate based on studies from the 1970’s that are now considered flawed • Expect new intolerances (i.e. any allergy or adverse reaction reported in a drug allergy field) to be reported after 0.5 to 4% of all antimicrobial courses depending on the gender and specific antimicrobial. Expect a higher incidence of new intolerances in patients with three or more prior medication intolerances1 • For type-1 immediate hypersensitivity reactions (IgE-mediated), cross-reactivity among penicillins (table 1) is expected due to similar core structure and/or major/minor antigenic determinants, use not recommended without desensitization • For type-1 immediate hypersensitivity reactions, cross-reactivity between penicillins (table 1) and cephalosporins is due to similarities in the side chains; risk of cross-reactivity will only be significant between penicillins and cephalosporins with similar side chains • Only type-1 immediate hypersensitivity to a penicillin manifesting as anaphylaxis, bronchospasm, -

Antibiotic Use for Sepsis in Neonates and Children: 2016 Evidence Update
Antibiotic Use for Sepsis in Neonates and Children: 2016 Evidence Update Aline Fuchsa, Julia Bielickia,b, Shrey Mathurb, Mike Sharlandb, Johannes N. Van Den Ankera,c a Paediatric Pharmacology and Pharmacometrics, University Children's Hospital Basel, Basel, Switzerland b Paediatric Infectious Disease Research Group, Institute for Infection and Immunity, St George's University of London, London, United Kingdom c Division of Clinical Pharmacology, Children’s National Health System, Washington, DC, USA WHO-Reviews 1 TABLE OF CONTENTS 1. INTRODUCTION ............................................................................................................................... 3 1.1. Aims ......................................................................................................................................... 3 1.2. Background ............................................................................................................................. 3 1.2.1. Definition and diagnosis ................................................................................................. 3 Neonatal Sepsis ............................................................................................................................... 3 Paediatric Sepsis ............................................................................................................................. 4 Community versus hospital acquired sepsis .................................................................................. 5 1.2.2. Microbiology .................................................................................................................. -
Comparative Activity of Newer Antibiotics Against Gram-Negative Bacilli
CONTRIBUTION • Comparative activity of newer antibiotics against gram-negative bacilli CYNTHIA C. KNAPP, MS AND JOHN A. WASHINGTON, MD • The in vitro activities of cefoperazone, cefotaxime, ceftriaxone, ceftazidime, azlocillin, mezlocillin, piperacillin, ticarcillin/clavulanate, aztreonam, imipenem, and ciprofloxacin were concurrently deter- mined against over 1,000 isolates of gram-negative bacilli from clinical specimens of patients at the Cleve- land Clinic. Cephalosporins, penicillins, and aztreonam were active against species of Enterobacteriaceae other than Citrobacter freundii, Enterobacter aerogenes, and Enterobacter cloacae. Ceftazidime was the most active cephalosporin against Pseudomonas aeruginosa. Against the Enterobacteriaceae, the rank order of activity of penicillins was ticarcillin/clavulanate > piperacillin > mezlocillin > azlocillin. Against P. aer- uginosa, the rank order of activity of penicillins was piperacillin > ticarcillin/clavulanate > azlocillin > mezlocillin. Aztreonam was less active v P. aeruginosa than ceftazidime, cefoperazone, or piperacillin. The most active antimicrobials against all isolates tested were imipenem and ciprofloxacin. • INDEX TERMS: ANTIBIOTICS, LACTAM; GRAM-NEGATIVE BACTERIA • CLEVE CLIN J MED 1989; 56:161-166 HE RECENT introduction of ciprofloxacin for and penicillins, as well as the monobactam, aztreonam, clinical use follows closely a period of active re- and the carbapenem, imipenem.1-3 search in and development of expanded spec- We compared the susceptibility of more than 1,000 trum p-lactam antibiotics, including cephalo- clinical bacterial isolates to four expanded spectrum Tsporins, penicillins, monobactams, and carbapenems. cephalosporins (cefoperazone, cefotaxime, ceftriaxone, Although numerous published studies compare the ac- and ceftazidime), four expanded spectrum penicillins tivity of ciprofloxacin with other quinolones, only a (azlocillin, mezlocillin, piperacillin, and ticarcil- limited number of studies compare the activity of ci- lin/clavulanate), aztreonam, imipenem, and ciproflox- acin. -

Ertapenem Or Ticarcillin/Clavulanate for the Treatment of Intra-Abdominal Infections Or Acute Pelvic Infections in Pediatric Patients
The American Journal of Surgery 194 (2007) 367–374 Clinical surgery–American Ertapenem or ticarcillin/clavulanate for the treatment of intra-abdominal infections or acute pelvic infections in pediatric patients Albert E. Yellin, M.D.a,*, Jeffrey Johnson, M.D.b, Iliana Higareda, M.D.c, Blaise L. Congeni, M.D.d, Antonio C. Arrieta, M.D.e, Doreen Fernsler, B.S.f, Joseph West, Ph.D.f, Richard Gesser, M.D.f aDepartment of Surgery, Keck School of Medicine of the University of Southern California, 1200 N State St, Rm 9610, Los Angeles, CA 90033, USA bDepartment of Pediatrics, Keck School of Medicine of the University of Southern California, 1240 N Mission Rd, L902, Los Angeles, CA 90089-9300, USA cHospital Civil de Guadalajara, Hospital 278, 4420 El Retiro St, Guadalajara, Jalisco Mexico dAkron Children’s Hospital, Division of Infectious Diseases, Locust Professional Bldg, 300 Locust St, Ste 4, Akron, OH 44308-1062, USA eChildren’s Hospital of Orange County, Pediatric Infectious Diseases, 455 South Main Street, Orange, CA 92868, USA fMerck Research Laboratories, Merck & Co., Inc., 126 East Lincoln Avenue, Rahway, NJ 07065, USA Manuscript received June 20, 2006; revised manuscript January 20, 2007 Abstract Background: Ertapenem, a group I carbapenem antibiotic, has been shown to be safe and effective in treating adults with complicated intra-abdominal (cIAI) or acute pelvic infection (API). This study evaluated ertapenem for treating these infections in children. Methods: In an open-label study, children aged 2 to 17 years with cIAI or API were randomized 3:1 to receive ertapenem or ticarcillin/clavulanate. -

Chemistry Classification Pharmacokinetics Clinical Uses And
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2014, 6(11):28-58 ISSN : 0975-7384 Review Article CODEN(USA) : JCPRC5 Chemistry, classification, pharmacokinetics, clinical uses and analysis of beta lactam antibiotics: A review Mamdouh S. Masoud a, Alaa E. Ali b* and Nessma M. Nasr c aChemistry Department, Faculty of Science, Alexandria University, Alexandria, Egypt bChemistry Department, Faculty of Science, Damanhour University, Damanhour, Egypt cStudents’ Hospital, Alexandria University, Alexandria, Egypt _____________________________________________________________________________________________ ABSTRACT This review attempts to pinpoint the importance of betalactam antibiotics, which encompass penicillins, cephalosporins, cephamycins, carbapenems and monobactams from its chemistry, classification, pharmacokinetics, clinical uses and analysis. β- lactam antibiotics have been used for treatment of bacterial infections. Most antibacterials are chemically semisynthetic modifications of various natural compounds and classified on the basis of chemical /biosynthetic origin into natural, semisynthetic, and synthetic. Also, this classification system is based on biological activity; that antibacterials are divided into two broad groups according to their biological effect on microorganisms, bactericidal agents kill bacteria, and bacteriostatic agents slow down bacterial growth. Keywords: Beta lactam Antibiotics, Classification, Pharmacokinetics, Clinical uses, Analysis. _____________________________________________________________________________________________ -

A Thesis Entitled an Oral Dosage Form of Ceftriaxone Sodium Using Enteric
A Thesis entitled An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy Option _________________________________________ Jerry Nesamony, Ph.D., Committee Chair _________________________________________ Sai Hanuman Sagar Boddu, Ph.D, Committee Member _________________________________________ Youssef Sari, Ph.D., Committee Member _________________________________________ Patricia R. Komuniecki, PhD, Dean College of Graduate Studies The University of Toledo May 2015 Copyright 2015, Darshan Narendra Lalwani This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy option The University of Toledo May 2015 Purpose: Ceftriaxone (CTZ) is a broad spectrum semisynthetic, third generation cephalosporin antibiotic. It is an acid labile drug belonging to class III of biopharmaceutical classification system (BCS). It can be solvated quickly but suffers from the drawback of poor oral bioavailability owing to its limited permeability through -
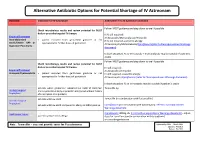
Shortage of Aztreonam Guidance Document.Pdf
Alternative Antibiotic Options for Potential Shortage of IV Aztreonam Guidance Indication for IV Aztreonam Alternative if no IV Aztreonam available Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy If IV still required: Empirical Treatment IV Amoxicillin/Metronidazole/Temocillin Intra-abdominal • patient excluded from gentamicin guidance or not If IV still required + pencillin allergy: sepsis/Severe HAP or appropriate for further doses of gentamicin IV Vancomycin/Metronidazole/Ciprofloxacin(refer to Fluoroquinolones Warnings Aspiration Pneumonia document) In both situations IV co-trimoxazole + metronidazole may be suitable if patient is stable Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy IV still required: Empirical Treatment IV Amoxicillin /Temocillin Urosepsis/Pyelonephritis • patient excluded from gentamicin guidance or not IV still required + pencillin allergy: appropriate for further doses of gentamicin IV Vancomycin /Ciprofloxacin (refer to Fluoroquinolones Warnings document) In both situations IV co-trimoxazole may be suitable if patient is stable patients where gentamicin indicated but eGFR 15-30ml/min Temocillin 1g Urology Surgical and no penicillin allergy or penicillin allergy but without history Prophylaxis of anaphylaxis or angiodema patients with low eGFR Temocillin (in combination with flucloxacillin) Vascular Surgical Prophylaxis patients with low eGFR and penicillin allergy or MRSA positive Ciprofloxacin (in combination with vancomycin): refer to Fluoroquinolones Warnings document Neutropenic Sepsis Ciprofloxacin 400mg tds (refer to Fluoroquinolones Warnings document)– adjust patients with pencillin allergy dose for renal function (in combination with teicoplanin) or consider gentamicin Note: Temocillin – does not provide cover for Pseudomonas Approved by AMG: March 2016 Updated: Feb 2019 Review: Feb 2022 .