Hap-Vap-Guidelines-2016.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antibacterial Drug Usage Analysis
Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology Drug Use Review Date: April 5, 2012 To: Edward Cox, M.D. Director Office of Antimicrobial Products Through: Gerald Dal Pan, M.D., MHS Director Office of Surveillance and Epidemiology Laura Governale, Pharm.D., MBA Deputy Director for Drug Use Division of Epidemiology II Office of Surveillance and Epidemiology Hina Mehta, Pharm.D. Drug Use Data Analysis Team Leader Division of Epidemiology II Office of Surveillance and Epidemiology From: Tracy Pham, Pharm.D. Drug Use Data Analyst Division of Epidemiology II Office of Surveillance and Epidemiology Drug Name(s): Systemic Antibacterial Drug Products Application Type/Number: Multiple Applicant/sponsor: Multiple OSE RCM #: 2012-544 **This document contains proprietary drug use data obtained by FDA under contract. The drug use data/information in this document has been cleared for public release.** 1 EXECUTIVE SUMMARY The Division of Epidemiology II is providing an update of the drug utilization data in terms of number of kilograms or international units of selected systemic antibacterial drug products sold from manufacturers to various retail and non-retail channels of distribution for years 2010-2011 as a surrogate for nationwide antibacterial drug use in humans. Propriety drug use databases licensed by the FDA were used to conduct this analysis. Data findings are as follows: During years 2010 and 2011, the majority of kilograms of selected systemic antibacterial drug products sold were to outpatient retail pharmacy settings. Approximately 3.28 million kilograms of selected systemic antibacterial drug products were sold during year 2010, and around 3.29 million kilograms were sold during year 2011. -

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -

Antibiotic Temocillin Be A
P0840 Could the ‘old’ antibiotic temocillin be a ‘new’ treatment for acute bacterial cholangitis? A retrospective study of 156 cases Sylvain Chawki1, Marion Duprilot1, Gary Taieb1, Veronique Leflon1, Marie-Hélène Nicolas-Chanoine1, Bruno Fantin1, Victoire De Lastours*1 1 Hôpital Beaujon, Assistance Publique Hôpitaux de Paris, Clichy, France Background: Acute cholangitis is a potentially severe infection requiring rapid active antimicrobial therapy. Thus, emergence of multidrug resistant strains of Enterobacteriaceae is a rising global public-health issue. To spare carbapenems, alternative therapies are needed. Temocillin is a narrow-spectrum betalactam targeting almost specifically Enterobacteriaceae, including most isolates resistant to third generation cephalosporin (3GC) and some carbapenemase-producers. Temocillin biliary concentrations may reach several times the blood concentrations. We assessed whether temocillin may represent an alternative treatment for bacterial cholangitis. Materials/methods: In this retrospective monocentric study, all patients from November 2015 to December 2017 admitted for acute cholangitis with a positive culture (blood or bile) were included. Demographic characteristics, severity, treatment and outcome of each episode were collected. Susceptibility to antibiotics, including temocillin, was determined phenotypically. Episodes of cholangitis were considered susceptible to temocillin if all pathogens found were temocillin-susceptible. Results: 137 patients (77/137 male; 56%; median age 67 [60-75]) who suffered 156 episodes of bacterial cholangitis were included (19 patients had 2 separate episodes during the study period). The median Charlson score was 4 [2-8]; 66/137 (48%) were immunocompromised, 54/137 (39%) had a history episode of acute cholangitis. 118/156 (75.6%) episodes were healthcare-associated, 28/156 (18%) required intensive care and 12 (7.7%) were fatal. -

Evaluation of Pharmacodynamic Interactions Between Telavancin
Infect Dis Ther DOI 10.1007/s40121-016-0121-2 ORIGINAL RESEARCH Evaluation of Pharmacodynamic Interactions Between Telavancin and Aztreonam or Piperacillin/ Tazobactam Against Pseudomonas aeruginosa, Escherichia coli and Methicillin-Resistant Staphylococcus aureus Juwon Yim . Jordan R. Smith . Katie E. Barber . Jessica A. Hallesy . Michael J. Rybak Received: May 2, 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT Methods: In vitro one-compartment PK/PD models were run over 96 h simulating TLV Introduction: In clinical trials comparing 10 mg/kg every 48 h, ATM 500 mg every 8 h telavancin (TLV) with vancomycin for and PTZ continuous infusion 13.5 g over 24 h treatment of hospital-acquired pneumonia, alone and in combination against P. aeruginosa, TLV demonstrated lower clinical cure rates E. coli and methicillin-resistant S. aureus than vancomycin in patients who had mixed (MRSA). The efficacy of antimicrobials was gram-positive and -negative infections and were evaluated by plotting time-kill curves and concomitantly treated with either aztreonam calculating the reduction in log10 cfu/ml over (ATM) or piperacillin/tazobactam (PTZ). Here, 96 h. we investigated therapeutic interactions Results: Against both MRSA strains, TLV was between TLV and ATM or PTZ in an in vitro rapidly bactericidal at 4 h and maintained its pharmacokinetic/pharmacodynamic (PK/PD) activity over 96 h with no observed antagonism model under simulated reduced renal function by either ATM or PTZ. PTZ maintained conditions. bacteriostatic and bactericidal activities against Enhanced content To view enhanced content for this E. coli ATCC 25922 and clinical strain R1022 at article go to http://www.medengine.com/Redeem/ 96 h, whereas both strains regrew as soon as 22E4F0603737CC9F. -

Ceftaroline in Complicated Skin and Skin-Structure Infections
Infection and Drug Resistance Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Ceftaroline in complicated skin and skin-structure infections Paul O Hernandez1 Abstract: Ceftaroline is an advanced-generation cephalosporin antibiotic recently approved by Sergio Lema2 the US Food and Drug Administration for the treatment of complicated skin and skin-structure Stephen K Tyring3 infections (cSSSIs). This intravenous broad-spectrum antibiotic exerts potent bactericidal activity Natalia Mendoza2,4 by inhibiting bacterial cell wall synthesis. A high affinity for the penicillin-binding protein 2a (PBP2a) of methicillin-resistant Staphylococcus aureus (MRSA) makes the drug especially 1University of Texas School of Medicine at San Antonio, beneficial to patients with MRSA cSSSIs. Ceftaroline has proved in multiple well-conducted San Antonio, TX, 2Woodhull clinical trials to have an excellent safety and efficacy profile. In adjusted doses it is also recom- Medical and Mental Health Center, mended for patients with renal or hepatic impairment. Furthermore, the clinical effectiveness Brooklyn, NY, 3Department of Dermatology, University of Texas and high cure rate demonstrated by ceftaroline in cSSSIs, including those caused by MRSA Health Science Center at Houston, and other multidrug-resistant strains, warrants its consideration as a first-line treatment option 4 Houston, TX, USA; Department of for cSSSIs. This article reviews ceftaroline and its pharmacology, efficacy, and safety data to Dermatology, El -

Chemistry Classification Pharmacokinetics Clinical Uses And
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2014, 6(11):28-58 ISSN : 0975-7384 Review Article CODEN(USA) : JCPRC5 Chemistry, classification, pharmacokinetics, clinical uses and analysis of beta lactam antibiotics: A review Mamdouh S. Masoud a, Alaa E. Ali b* and Nessma M. Nasr c aChemistry Department, Faculty of Science, Alexandria University, Alexandria, Egypt bChemistry Department, Faculty of Science, Damanhour University, Damanhour, Egypt cStudents’ Hospital, Alexandria University, Alexandria, Egypt _____________________________________________________________________________________________ ABSTRACT This review attempts to pinpoint the importance of betalactam antibiotics, which encompass penicillins, cephalosporins, cephamycins, carbapenems and monobactams from its chemistry, classification, pharmacokinetics, clinical uses and analysis. β- lactam antibiotics have been used for treatment of bacterial infections. Most antibacterials are chemically semisynthetic modifications of various natural compounds and classified on the basis of chemical /biosynthetic origin into natural, semisynthetic, and synthetic. Also, this classification system is based on biological activity; that antibacterials are divided into two broad groups according to their biological effect on microorganisms, bactericidal agents kill bacteria, and bacteriostatic agents slow down bacterial growth. Keywords: Beta lactam Antibiotics, Classification, Pharmacokinetics, Clinical uses, Analysis. _____________________________________________________________________________________________ -

Real-World Use of Telavancin in the Treatment of Osteomyelitis
Diagnostic Microbiology and Infectious Disease 95 (2019) 185–190 Contents lists available at ScienceDirect Diagnostic Microbiology and Infectious Disease journal homepage: www.elsevier.com/locate/diagmicrobio Real-world use of telavancin in the treatment of osteomyelitis Louis D. Saravolatz a,⁎, Kerry O. Cleveland b, Khalid Rikabi c, Ali Hassoun d, Joseph Reilly e, Leonard B. Johnson a, Cedric Spak f, Sharon Valenti a, Susan Szpunar a a Ascension-St John Hospital and Wayne State University School of Medicine, Grosse Pointe Woods, Michigan, USA b University of Tennessee, Mephis Tennessee, USA c Geographic Medicine Services of Biloxi, Biloxi, Mississippi, USA d Alabama Infectious Diseases Center, Huntsville, Alabama, USA e AtlantiCare Regional Medical Center, Pomona, NJ, USA f North Texas Disease Consultants, Dallas, Texas, USA article info abstract Article history: This is a retrospective analysis of patients with osteomyelitis who received telavancin at some time during their Received 30 November 2018 treatment course. The primary outcome was the percent of patients cured or improved at the end of telavancin Received in revised form 17 May 2019 therapy (EOTT). The secondary outcome was the percent of patients cured or improved three months after dis- Accepted 18 May 2019 continuation of telavancin therapy. There were 32 cases of osteomyelitis with methicillin-resistant Staphylococ- Available online 28 May 2019 cus aureus identified in 17 (56.7%), methicillin-sensitive Staphylococcus aureus 2(6.6%), coagulase negative Keywords: staphylococci 6 (20.0%) and other pathogens, 5 (16.7%). At EOTT, 87.5% of patients had their osteomyelitis Telavancin cured and 94.6% had the infection cured at three months after telavancin was completed. -

A Thesis Entitled an Oral Dosage Form of Ceftriaxone Sodium Using Enteric
A Thesis entitled An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy Option _________________________________________ Jerry Nesamony, Ph.D., Committee Chair _________________________________________ Sai Hanuman Sagar Boddu, Ph.D, Committee Member _________________________________________ Youssef Sari, Ph.D., Committee Member _________________________________________ Patricia R. Komuniecki, PhD, Dean College of Graduate Studies The University of Toledo May 2015 Copyright 2015, Darshan Narendra Lalwani This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy option The University of Toledo May 2015 Purpose: Ceftriaxone (CTZ) is a broad spectrum semisynthetic, third generation cephalosporin antibiotic. It is an acid labile drug belonging to class III of biopharmaceutical classification system (BCS). It can be solvated quickly but suffers from the drawback of poor oral bioavailability owing to its limited permeability through -

Full Prescribing Information for Prolong Aptt for up to 120 Hours, and May Prolong PT and INR for up ORBACTIV
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------WARNINGS AND PRECAUTIONS----------------------- These highlights do not include all the information needed to use • Coagulation test interference: ORBACTIV has been shown to artificially ORBACTIV safely and effectively. See full prescribing information for prolong aPTT for up to 120 hours, and may prolong PT and INR for up ORBACTIV. to 12 hours and ACT for up to 24 hours. For patients who require aPTT monitoring within 120 hours of ORBACTIV dosing, consider a ORBACTIV® (oritavancin) for injection, for intravenous use non-phospholipid dependent coagulation test such as a Factor Xa Initial U.S. Approval: 2014 (chromogenic) assay or an alternative anticoagulant not requiring aPTT. (5.1, 7.2) ----------------------------INDICATIONS AND USAGE--------------------------- • Serious hypersensitivity reactions, including anaphylaxis, have been ORBACTIV is a lipoglycopeptide antibacterial drug indicated for the reported with the use of oritavancin products, including ORBACTIV. treatment of adult patients with acute bacterial skin and skin structure Discontinue infusion if signs of acute hypersensitivity occur. Carefully infections caused or suspected to be caused by susceptible isolates of monitor patients with known hypersensitivity to glycopeptides. (5.2) designated Gram-positive microorganisms. (1.1) • Infusion Related Reactions: Administer ORBACTIV over 3 hours to minimize infusion. Infusion related reactions have been reported with To reduce the development of drug-resistant bacteria and maintain the the glycopeptide class of antimicrobial agents, including oritavancin effectiveness of ORBACTIV and other antibacterial drugs, ORBACTIV products (e.g. ORBACTIV). Stopping or slowing the infusion may result should be used only to treat or prevent infections that are proven or strongly in cessation of these reactions. -

Telavancin Activity Tested Against Gram-Positive Clinical Isolates
TN004-14 ECCMID 14_JMI 11_12 EU lc14_Layout 1 24/04/2014 17:44 Page 1 Poster P1579 Contact information: Rodrigo E. Mendes , PhD Telavancin Activity Tested Against Gram-Positive Clinical Isolates From European Hospitals (2011 –2013) JMI Laboratories 345 Beaver Kreek Ctr, Ste A Using A Revised Broth Microdilution Testing Method: Redefining the Baseline Activity for Telavancin North Liberty, Iowa 52317 USA Phone: 319-665-3370 Fax: 319-665-3371 Rodrigo E. Mendes*, David J. Farrell, Jennifer M. Streit , Ronald N. Jones E-mail: [email protected] JMI Laboratories, North Liberty, Iowa, USA Table 1. Antimicrobial activity and MIC distribution for telavancin when tested against 11 ,601 contemporary (2011 –2013) clinical isolates from European and adjacent countries , as part of the international telavancin surveillance programme • This revised reference method for telavancin resembles those utilised for other lipoglycopeptide Table 2. Antimicrobial activity of telavancin and comparator agents tested against Gram-positive clinical isolates from European and ABSTRACT MIC (mg/L) Number (cumulative %) inhibited at telavancin MIC (mg/L) b agents, such as dalbavancin and oritavancin .5,6 adjacent countries , as part of the 2011 –2013 international telavancin surveillance programme a Organism (no. tested) 50% 90% ≤0.015 0.03 0.06 0.12 0.25 0.5 1 >1 a MIC (mg/L ) %Susceptible/%Intermediate/Resistant b Objectives : To reassess the activity of telavancin when tested against clinical isolates recovered from • The susceptibility testing methods for these agents also incorporate P-80, which was shown to be Organism (no. tested)/ MSSA (4108) 0.03 0.06 157 (3.8) 2514 (65.0) 1430 (99.8) 7 (100.0) Antimicrobial agent Range 50% 90% CLSI EUCAST hospitalised patients in European and adjacent countries. -
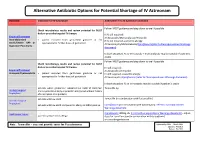
Shortage of Aztreonam Guidance Document.Pdf
Alternative Antibiotic Options for Potential Shortage of IV Aztreonam Guidance Indication for IV Aztreonam Alternative if no IV Aztreonam available Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy If IV still required: Empirical Treatment IV Amoxicillin/Metronidazole/Temocillin Intra-abdominal • patient excluded from gentamicin guidance or not If IV still required + pencillin allergy: sepsis/Severe HAP or appropriate for further doses of gentamicin IV Vancomycin/Metronidazole/Ciprofloxacin(refer to Fluoroquinolones Warnings Aspiration Pneumonia document) In both situations IV co-trimoxazole + metronidazole may be suitable if patient is stable Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy IV still required: Empirical Treatment IV Amoxicillin /Temocillin Urosepsis/Pyelonephritis • patient excluded from gentamicin guidance or not IV still required + pencillin allergy: appropriate for further doses of gentamicin IV Vancomycin /Ciprofloxacin (refer to Fluoroquinolones Warnings document) In both situations IV co-trimoxazole may be suitable if patient is stable patients where gentamicin indicated but eGFR 15-30ml/min Temocillin 1g Urology Surgical and no penicillin allergy or penicillin allergy but without history Prophylaxis of anaphylaxis or angiodema patients with low eGFR Temocillin (in combination with flucloxacillin) Vascular Surgical Prophylaxis patients with low eGFR and penicillin allergy or MRSA positive Ciprofloxacin (in combination with vancomycin): refer to Fluoroquinolones Warnings document Neutropenic Sepsis Ciprofloxacin 400mg tds (refer to Fluoroquinolones Warnings document)– adjust patients with pencillin allergy dose for renal function (in combination with teicoplanin) or consider gentamicin Note: Temocillin – does not provide cover for Pseudomonas Approved by AMG: March 2016 Updated: Feb 2019 Review: Feb 2022 . -

Telavancin Hydrochloride ASHP INJECTABLE DRUG INFORMATION
1472 TELAVANCIN HYDROCHLORIDE ASHP INJECTABLE DRUG INFORMATION Telavancin Hydrochloride AHFS 8:12.28.16 Products is recommended.2831 For doses outside this range, dilution to a concentration of 0.6 to 8 mg/mL is recommended.2831 The manu- Telavancin hydrochloride is available as a lyophilized powder facturer recommends dilution in dextrose 5%; sodium chloride in single-use vials containing telavancin 250 and 750 mg as the 0.9%; or Ringer’s injection, lactated.2831 hydrochloride.2831 Also present are hydroxypropyl-beta-cyclo- dextrin, mannitol, and sodium hydroxide and hydrochloric acid to adjust pH.2831 Stability Intact vials of telavancin hydrochloride should be stored under The 250-mg vial should be reconstituted with 15 mL and the refrigeration.2831 The reconstituted drug in the vial and the 750-mg vial with 45 mL of dextrose 5%, sterile water for injection, diluted solution in the infusion bag should be used within 12 or sodium chloride 0.9% and mixed thoroughly to yield a telavancin hours if stored at room temperature or 7 days if stored under concentration of 15 mg/mL.2831 To minimize foaming during recon- refrigeration.2831 3097 The total time for the reconstituted drug stitution, allow the vacuum of the vial to draw the diluent from the in the vial and the diluted solution in the infusion bag together syringe into the vial; do not forcefully inject the diluent.2831 Any vial should not exceed 12 hours at room temperature or 7 days that does not have a vacuum should be discarded.2831 Dissolution under refrigeration.2831 3097 may