NURSING CARE PLAN for Ineffective Airway Clearance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identifying COPD by Crackle Characteristics
BMJ Open Resp Res: first published as 10.1136/bmjresp-2020-000852 on 5 March 2021. Downloaded from Respiratory epidemiology Inspiratory crackles—early and late— revisited: identifying COPD by crackle characteristics Hasse Melbye ,1 Juan Carlos Aviles Solis,1 Cristina Jácome,2 Hans Pasterkamp3 To cite: Melbye H, Aviles ABSTRACT Key messages Solis JC, Jácome C, et al. Background The significance of pulmonary crackles, Inspiratory crackles— by their timing during inspiration, was described by Nath early and late—revisited: and Capel in 1974, with early crackles associated with What is the key question? identifying COPD by bronchial obstruction and late crackles with restrictive ► In the diagnosis of chronic obstructive pulmonary crackle characteristics. defects. Crackles are also described as ‘fine’ or disease (COPD), is it more useful to focus on the tim- BMJ Open Resp Res ‘coarse’. We aimed to evaluate the usefulness of crackle ing of crackles than on the crackle type? 2021;8:e000852. doi:10.1136/ bmjresp-2020-000852 characteristics in the diagnosis of chronic obstructive What is the bottom line? pulmonary disease (COPD). ► Pulmonary crackles are divided into two types, ‘fine’ Methods In a population-based study, lung sounds Received 2 December 2020 and ‘coarse’ and coarse inspiratory crackles are re- Revised 2 February 2021 were recorded at six auscultation sites and classified in garded to be typical of COPD. In bronchial obstruc- Accepted 5 February 2021 participants aged 40 years or older. Inspiratory crackles tion crackles tend to appear early in inspiration, and were classified as ‘early’ or ‘late and into the types’ this characteristic of the crackle might be easier for ‘coarse’ and ‘fine’ by two observers. -

Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients
Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients 1 Hajime Kataoka, MD ABSTRACT 2 Osamu Matsuno, MD PURPOSE The presence of age-related pulmonary crackles (rales) might interfere 1Division of Internal Medicine, with a physician’s clinical management of patients with suspected heart failure. Nishida Hospital, Oita, Japan We examined the characteristics of pulmonary crackles among patients with stage A cardiovascular disease (American College of Cardiology/American Heart 2Division of Respiratory Disease, Oita University Hospital, Oita, Japan Association heart failure staging criteria), stratifi ed by decade, because little is known about these issues in such patients at high risk for congestive heart failure who have no structural heart disease or acute heart failure symptoms. METHODS After exclusion of comorbid pulmonary and other critical diseases, 274 participants, in whom the heart was structurally (based on Doppler echocar- diography) and functionally (B-type natriuretic peptide <80 pg/mL) normal and the lung (X-ray evaluation) was normal, were eligible for the analysis. RESULTS There was a signifi cant difference in the prevalence of crackles among patients in the low (45-64 years; n = 97; 11%; 95% CI, 5%-18%), medium (65-79 years; n = 121; 34%; 95% CI, 27%-40%), and high (80-95 years; n = 56; 70%; 95% CI, 58%-82%) age-groups (P <.001). The risk for audible crackles increased approximately threefold every 10 years after 45 years of age. During a mean fol- low-up of 11 ± 2.3 months (n = 255), the short-term (≤3 months) reproducibility of crackles was 87%. The occurrence of cardiopulmonary disease during follow-up included cardiovascular disease in 5 patients and pulmonary disease in 6. -

Assessing and Managing Lung Disease and Sleep Disordered Breathing in Children with Cerebral Palsy Paediatric Respiratory Review
Paediatric Respiratory Reviews 10 (2009) 18–24 Contents lists available at ScienceDirect Paediatric Respiratory Reviews CME Article Assessing and managing lung disease and sleep disordered breathing in children with cerebral palsy Dominic A. Fitzgerald 1,3,*, Jennifer Follett 2, Peter P. Van Asperen 1,3 1 Department of Respiratory Medicine, University of Sydney, Sydney, New South Wales, Australia 2 Department of Physiotherapy, The Children’s Hospital at Westmead, University of Sydney, Sydney, New South Wales, Australia 3 The Children’s Hospital at Westmead Clinical School, Discipline of Paediatrics & Child Health, University of Sydney, Sydney, New South Wales, Australia EDUCATIONAL AIMS To appreciate the insidious evolution of suppurative lung disease in children with cerebral palsy (CP). To be familiar with the management of excessive oral secretions in children with CP. To understand the range of sleep problems that are more commonly seen in children with CP. To gain an understanding of the use of non-invasive respiratory support for the management of airway clearance and sleep disordered breathing in children with CP. ARTICLE INFO SUMMARY Keywords: The major morbidity and mortality associated with cerebral palsy (CP) relates to respiratory compromise. Cerebral palsy This manifests through repeated pulmonary aspiration, airway colonization with pathogenic bacteria, Pulmonary aspiration the evolution of bronchiectasis and sleep disordered breathing. An accurate assessment involving a Suppurative lung disease multidisciplinary approach and relatively simple interventions for these conditions can lead to Physiotherapy significant improvements in the quality of life of children with CP as well as their parents and carers. This Airway clearance techniques Obstructive sleep apnoea review highlights the more common problems and potential therapies with regard to suppurative lung Sleep disordered breathing disease and sleep disordered breathing in children with CP. -

Problems in Family Practice
problems in Family Practice Coughing in Childhood Hyman Sh ran d , M D Cambridge, M assachusetts Coughing in childhood is a common complaint involving a wide spectrum of underlying causes which require a thorough and rational approach by the physician. Most children who cough have relatively simple self-limiting viral infections, but some may have serious disease. A dry environment, allergic factors, cystic fibrosis, and other major illnesses must always be excluded. A simple clinical approach, and the sensible use of appropriate investigations, is most likely to succeed in finding the cause, which can allow precise management. The cough reflex as part of the defense mechanism of the respiratory tract is initiated by mucosal changes, secretions or foreign material in the pharynx, larynx, tracheobronchial Table 1. Persistent Cough — Causes in Childhood* tree, pleura, or ear. Acting as the “watchdog of the lungs,” the “good” cough prevents harmful agents from Common Uncommon Rare entering the respiratory tract; it also helps bring up irritant material from Environmental Overheating with low humidity the airway. The “bad” cough, on the Allergens other hand, serves no useful purpose Pollution Tobacco smoke and, if persistent, causes fatigue, keeps Upper Respiratory Tract the child (and parents) awake, inter Recurrent viral URI Pertussis Laryngeal stridor feres with feeding, and induces vomit Rhinitis, Pharyngitis Echo 12 Vocal cord palsy Allergic rhinitis Nasal polyp Vascular ring ing. It is best suppressed. Coughs and Prolonged use of nose drops Wax in ear colds constitute almost three quarters Sinusitis of all illness in young children. The Lower Respiratory Tract Asthma Cystic fibrosis Rt. -
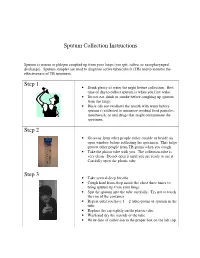
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Chest Pain in a Patient with Cystic Fibrosis
Copyright ©ERS Journals Ltd 1998 Eur Respir J 1998; 12: 245–247 European Respiratory Journal DOI: 10.1183/09031936.98.12010245 ISSN 0903 - 1936 Printed in UK - all rights reserved CASE FOR DIAGNOSIS Chest pain in a patient with cystic fibrosis D.P. Dunagan*, S.L. Aquino+, M.S. Schechter**, B.K. Rubin**, J.W. Georgitis** Case history A 38 yr old female with a history of cystic fibrosis (CF) presented to an outside emergency department with dysp- noea and right-sided chest pain of approximately 12 h duration. Her history was significant for recurrent pneu- mothoraces and a recent respiratory exacerbation of CF requiring prolonged antibiotic therapy for Pseudomonas aeruginosa. She described the pain as relatively acute in onset, sharp, increased with deep inspiration, without out- ward radiation, and progressive in intensity. There was no history of travel, worsening cough, fever, chills or increase in her chronic expectoration of blood-streaked sputum. An outside chest radiograph was interpreted as demonstrating a "rounded" right lower lobe pneumonia and she was transferred to our institution for further evaluation. Fig. 2. – Computed tomography scan of the chest. Open arrow: multi- On examination, she was thin, afebrile and in minimal ple cysts; closed white arrow: 3.8×5 cm round mass, respiratory distress. There were decreased breath sounds throughout all lung fields, symmetric chest wall excursion with inspiration and bilateral basilar crackles. Subjective right lateral chest discomfort was reported with deep ins- piratory manoeuvres. The remaining physical examination was normal except for clubbing of the upper extremities. Laboratory data revealed an elevated white blood cell count of 19.2×109 cells·L-1 with a normal differential. -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

Respiratory Failure
Respiratory Failure Phuong Vo, MD,* Virginia S. Kharasch, MD† *Division of Pediatric Pulmonary and Allergy, Boston Medical Center, Boston, MA †Division of Respiratory Diseases, Boston Children’s Hospital, Boston, MA Practice Gap The primary cause of cardiopulmonary arrest in children is unrecognized respiratory failure. Clinicians must recognize respiratory failure in its early stage of presentation and know the appropriate clinical interventions. Objectives After completing this article, readers should be able to: 1. Recognize the clinical parameters of respiratory failure. 2. Describe the respiratory developmental differences between children and adults. 3. List the clinical causes of respiratory failure. 4. Review the pathophysiologic mechanisms of respiratory failure. 5. Evaluate and diagnose respiratory failure. 6. Discuss the various clinical interventions for respiratory failure. WHAT IS RESPIRATORY FAILURE? Respiratory failure is a condition in which the respiratory system fails in oxy- genation or carbon dioxide elimination or both. There are 2 types of impaired gas exchange: (1) hypoxemic respiratory failure, which is a result of lung failure, and (2) hypercapnic respiratory failure, which is a result of respiratory pump failure (Figure 1). (1)(2) In hypoxemic respiratory failure, ventilation-perfusion (V_ =Q)_ mismatch results in the decrease of PaO2) to below 60 mm Hg with normal or low PaCO2. _ = _ (1) In hypercapnic respiratory failure, V Q mismatch results in the increase of AUTHOR DISCLOSURE Drs Vo and Kharasch fi PaCO2 to above 50 mm Hg. Either hypoxemic or hypercapnic respiratory failure have disclosed no nancial relationships can be acute or chronic. Acute respiratory failure develops in minutes to hours, relevant to this article. -

Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Fall 12-18-2015 Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT Christopher C. Schultz University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Other Medical Specialties Commons Recommended Citation Schultz, Christopher C., "Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT" (2015). Theses & Dissertations. 54. https://digitalcommons.unmc.edu/etd/54 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. EVALUATION OF UPPER AIRWAY CHANGES FOLLOWING SURGICAL REMOVAL OF THE ADENOIDS USING 3-D CONE BEAM CT By Christopher C. Schultz, D.D.S A THESIS Presented to the Faculty of The Graduate College in the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Master of Science Medical Sciences Interdepartmental Area Oral Biology University of Nebraska Medical Center Omaha, Nebraska December, 2015 Advisory Committee: Sundaralingam Premaraj, BDS, MS, PhD, FRCD(C) Sheela Premaraj, BDS, PhD Peter J. Giannini, DDS, MS Stanton D. Harn, PhD i ACKNOWLEDGEMENTS I would like to express my thanks and gratitude to the members of my thesis committee: Dr. Sundaralingam Premaraj, Dr. Sheela Premaraj, Dr. Peter Giannini, and Dr. Stanton Harn. Your advice and assistance has been vital for the completion of the project. -

What Is Acute Respiratory Distress Syndrome?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What is Acute Respiratory Distress Syndrome? Acute Respiratory Distress Syndrome (ARDS) is a life-threatening illness in which the lungs are severely inflamed. Swelling throughout the lungs cause tiny blood vessels to leak fluid and the air sacs (alveoli) collapse or fill with fluid, preventing the lungs from working well. Patients with ARDS have problems getting enough oxygen into their blood so they must be given extra oxygen and will usually need a ventilator to breathe. Despite intensive treatment, about 40% of people with ARDS die from lung failure. Who gets ARDS? How is ARDS treated? It is estimated that ARDS affects about 150,000 Currently, there is no specific treatment for ARDS. Americans each year. ARDS can occur in many situations. Treatment consists of two goals: ARDS can affect people who have known lung disease or ■ treat any medical problem that led to the lung injury, other serious illnesses. A person can develop ARDS even and if he or she has not had lung disease or a lung problem in ■ support the person’s breathing (usually with a the past. ventilator) until the lungs heal. Most people with ARDS What causes ARDS? are treated in the hospital’s intensive care unit (ICU). The causes of ARDS are not well understood. Either Therapies commonly used for ARDS include: direct or indirect injuries can cause ARDS. Direct ■ Breathing support from a mechanical ventilator. injuries include: pneumonia, inhaling stomach contents ■ CLIP AND COPY AND CLIP Medicines to keep the person calm and comfortable (aspiration), breathing in harmful fumes or smoke, and while on the ventilator so that they can rest and injury to the chest that causes bruising of the lungs. -

What Is Acute Bronchitis?
What is acute bronchitis? FACT SHEET prepared by The Asthma and Respiratory Foundation NZ Acute bronchitis is an infection of the large bronchi (airways) in the lungs. The airways swell and thick mucus builds up inside them. It is often caused by the same viruses that cause the common cold. A minority of cases are caused by bacteria. How do I know that I have acute bronchitis? Acute bronchitis may accompany or closely follow a cold or influenza or may occur on its own. The major symptom of acute bronchitis is a productive cough that may bring up yellow or green sputum (phlegm). This cough can last several weeks. Some people may have shortness of breath and a wheeze. There may be other symptoms associated with the viral cause such as a runny nose, sore throat, fever, muscle aches and pains, sore eyes or headache, particularly early in the illness. Chest pain is not usually associated with bronchitis. Who gets acute bronchitis? Anyone can get acute bronchitis. It is more common in winter, especially during influenza outbreaks. Tobacco smoke and other air pollutants appear to worsen symptoms and may prolong the cough. People with a chronic lung disease can also get acute bronchitis, but may need different treatment. How is acute bronchitis treated? Most cases will go away after a few days or a week though the cough may linger for several weeks or months. This indicates that the airways are taking a longer time to heal. As most cases of acute bronchitis are caused by virus’s, antibiotics are usually not effective.