Respiratory Failure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
Emergency Nursing Program Foreword
RESOURCE MANUAL NSW HEALTH 2011 Transition to Practice Emergency Nursing Program Foreword The role of emergency nurses requires a broad level of skill and ability to meet the care needs of patients and their families. The Transition to Emergency Nursing Program is designed to support registered nurses new to the practice of emergency nursing. The Emergency Department is a fast-moving environment within which nurses can find themselves faced with a variety of challenges across a day. This program will assist them as they develop their knowledge and skills to meet these often changing care needs within the emergency setting. The program also supports a more consistent approach to transition to emergency nursing and it is anticipated will become the standard for initial entry to practice as an emergency nurse across NSW. This Resource Manual is the core document for the program and is complemented by both the Participant Workbook and the Facilitator’s Manual. Within the Emergency Department participants will be supported by staff to meet the relevant learning objectives during the 3-6 months over which this program extends. The development of the Transition to Emergency Nursing Program has been a lengthy process which reflects the commitment of emergency nurses to their area of practice and I acknowledge and thank them for their enthusiasm and work in enabling the Program to be developed. I am sure that it will have a positive impact for those nurses new to emergency nursing and to the care of patients. 1 Adjunct Professor Debra Thoms Chief Nursing and Midwifery Officer NSW Health NSW Department of Health 73 Miller Street NORTH SYDNEY NSW 2060 Tel. -

Identifying COPD by Crackle Characteristics
BMJ Open Resp Res: first published as 10.1136/bmjresp-2020-000852 on 5 March 2021. Downloaded from Respiratory epidemiology Inspiratory crackles—early and late— revisited: identifying COPD by crackle characteristics Hasse Melbye ,1 Juan Carlos Aviles Solis,1 Cristina Jácome,2 Hans Pasterkamp3 To cite: Melbye H, Aviles ABSTRACT Key messages Solis JC, Jácome C, et al. Background The significance of pulmonary crackles, Inspiratory crackles— by their timing during inspiration, was described by Nath early and late—revisited: and Capel in 1974, with early crackles associated with What is the key question? identifying COPD by bronchial obstruction and late crackles with restrictive ► In the diagnosis of chronic obstructive pulmonary crackle characteristics. defects. Crackles are also described as ‘fine’ or disease (COPD), is it more useful to focus on the tim- BMJ Open Resp Res ‘coarse’. We aimed to evaluate the usefulness of crackle ing of crackles than on the crackle type? 2021;8:e000852. doi:10.1136/ bmjresp-2020-000852 characteristics in the diagnosis of chronic obstructive What is the bottom line? pulmonary disease (COPD). ► Pulmonary crackles are divided into two types, ‘fine’ Methods In a population-based study, lung sounds Received 2 December 2020 and ‘coarse’ and coarse inspiratory crackles are re- Revised 2 February 2021 were recorded at six auscultation sites and classified in garded to be typical of COPD. In bronchial obstruc- Accepted 5 February 2021 participants aged 40 years or older. Inspiratory crackles tion crackles tend to appear early in inspiration, and were classified as ‘early’ or ‘late and into the types’ this characteristic of the crackle might be easier for ‘coarse’ and ‘fine’ by two observers. -

Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients
Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients 1 Hajime Kataoka, MD ABSTRACT 2 Osamu Matsuno, MD PURPOSE The presence of age-related pulmonary crackles (rales) might interfere 1Division of Internal Medicine, with a physician’s clinical management of patients with suspected heart failure. Nishida Hospital, Oita, Japan We examined the characteristics of pulmonary crackles among patients with stage A cardiovascular disease (American College of Cardiology/American Heart 2Division of Respiratory Disease, Oita University Hospital, Oita, Japan Association heart failure staging criteria), stratifi ed by decade, because little is known about these issues in such patients at high risk for congestive heart failure who have no structural heart disease or acute heart failure symptoms. METHODS After exclusion of comorbid pulmonary and other critical diseases, 274 participants, in whom the heart was structurally (based on Doppler echocar- diography) and functionally (B-type natriuretic peptide <80 pg/mL) normal and the lung (X-ray evaluation) was normal, were eligible for the analysis. RESULTS There was a signifi cant difference in the prevalence of crackles among patients in the low (45-64 years; n = 97; 11%; 95% CI, 5%-18%), medium (65-79 years; n = 121; 34%; 95% CI, 27%-40%), and high (80-95 years; n = 56; 70%; 95% CI, 58%-82%) age-groups (P <.001). The risk for audible crackles increased approximately threefold every 10 years after 45 years of age. During a mean fol- low-up of 11 ± 2.3 months (n = 255), the short-term (≤3 months) reproducibility of crackles was 87%. The occurrence of cardiopulmonary disease during follow-up included cardiovascular disease in 5 patients and pulmonary disease in 6. -

Assessing and Managing Lung Disease and Sleep Disordered Breathing in Children with Cerebral Palsy Paediatric Respiratory Review
Paediatric Respiratory Reviews 10 (2009) 18–24 Contents lists available at ScienceDirect Paediatric Respiratory Reviews CME Article Assessing and managing lung disease and sleep disordered breathing in children with cerebral palsy Dominic A. Fitzgerald 1,3,*, Jennifer Follett 2, Peter P. Van Asperen 1,3 1 Department of Respiratory Medicine, University of Sydney, Sydney, New South Wales, Australia 2 Department of Physiotherapy, The Children’s Hospital at Westmead, University of Sydney, Sydney, New South Wales, Australia 3 The Children’s Hospital at Westmead Clinical School, Discipline of Paediatrics & Child Health, University of Sydney, Sydney, New South Wales, Australia EDUCATIONAL AIMS To appreciate the insidious evolution of suppurative lung disease in children with cerebral palsy (CP). To be familiar with the management of excessive oral secretions in children with CP. To understand the range of sleep problems that are more commonly seen in children with CP. To gain an understanding of the use of non-invasive respiratory support for the management of airway clearance and sleep disordered breathing in children with CP. ARTICLE INFO SUMMARY Keywords: The major morbidity and mortality associated with cerebral palsy (CP) relates to respiratory compromise. Cerebral palsy This manifests through repeated pulmonary aspiration, airway colonization with pathogenic bacteria, Pulmonary aspiration the evolution of bronchiectasis and sleep disordered breathing. An accurate assessment involving a Suppurative lung disease multidisciplinary approach and relatively simple interventions for these conditions can lead to Physiotherapy significant improvements in the quality of life of children with CP as well as their parents and carers. This Airway clearance techniques Obstructive sleep apnoea review highlights the more common problems and potential therapies with regard to suppurative lung Sleep disordered breathing disease and sleep disordered breathing in children with CP. -

Problems in Family Practice
problems in Family Practice Coughing in Childhood Hyman Sh ran d , M D Cambridge, M assachusetts Coughing in childhood is a common complaint involving a wide spectrum of underlying causes which require a thorough and rational approach by the physician. Most children who cough have relatively simple self-limiting viral infections, but some may have serious disease. A dry environment, allergic factors, cystic fibrosis, and other major illnesses must always be excluded. A simple clinical approach, and the sensible use of appropriate investigations, is most likely to succeed in finding the cause, which can allow precise management. The cough reflex as part of the defense mechanism of the respiratory tract is initiated by mucosal changes, secretions or foreign material in the pharynx, larynx, tracheobronchial Table 1. Persistent Cough — Causes in Childhood* tree, pleura, or ear. Acting as the “watchdog of the lungs,” the “good” cough prevents harmful agents from Common Uncommon Rare entering the respiratory tract; it also helps bring up irritant material from Environmental Overheating with low humidity the airway. The “bad” cough, on the Allergens other hand, serves no useful purpose Pollution Tobacco smoke and, if persistent, causes fatigue, keeps Upper Respiratory Tract the child (and parents) awake, inter Recurrent viral URI Pertussis Laryngeal stridor feres with feeding, and induces vomit Rhinitis, Pharyngitis Echo 12 Vocal cord palsy Allergic rhinitis Nasal polyp Vascular ring ing. It is best suppressed. Coughs and Prolonged use of nose drops Wax in ear colds constitute almost three quarters Sinusitis of all illness in young children. The Lower Respiratory Tract Asthma Cystic fibrosis Rt. -

Chest Pain in a Patient with Cystic Fibrosis
Copyright ©ERS Journals Ltd 1998 Eur Respir J 1998; 12: 245–247 European Respiratory Journal DOI: 10.1183/09031936.98.12010245 ISSN 0903 - 1936 Printed in UK - all rights reserved CASE FOR DIAGNOSIS Chest pain in a patient with cystic fibrosis D.P. Dunagan*, S.L. Aquino+, M.S. Schechter**, B.K. Rubin**, J.W. Georgitis** Case history A 38 yr old female with a history of cystic fibrosis (CF) presented to an outside emergency department with dysp- noea and right-sided chest pain of approximately 12 h duration. Her history was significant for recurrent pneu- mothoraces and a recent respiratory exacerbation of CF requiring prolonged antibiotic therapy for Pseudomonas aeruginosa. She described the pain as relatively acute in onset, sharp, increased with deep inspiration, without out- ward radiation, and progressive in intensity. There was no history of travel, worsening cough, fever, chills or increase in her chronic expectoration of blood-streaked sputum. An outside chest radiograph was interpreted as demonstrating a "rounded" right lower lobe pneumonia and she was transferred to our institution for further evaluation. Fig. 2. – Computed tomography scan of the chest. Open arrow: multi- On examination, she was thin, afebrile and in minimal ple cysts; closed white arrow: 3.8×5 cm round mass, respiratory distress. There were decreased breath sounds throughout all lung fields, symmetric chest wall excursion with inspiration and bilateral basilar crackles. Subjective right lateral chest discomfort was reported with deep ins- piratory manoeuvres. The remaining physical examination was normal except for clubbing of the upper extremities. Laboratory data revealed an elevated white blood cell count of 19.2×109 cells·L-1 with a normal differential. -

Vitals & Assessment Bingo
Vitals & Assessment Bingo myfreebingocards.com Safety First! Before you print all your bingo cards, please print a test page to check they come out the right size and color. Your bingo cards start on Page 3 of this PDF. If your bingo cards have words then please check the spelling carefully. If you need to make any changes go to mfbc.us/e/dtfgtk Play Once you've checked they are printing correctly, print off your bingo cards and start playing! On the next page you will find the "Bingo Caller's Card" - this is used to call the bingo and keep track of which words have been called. Your bingo cards start on Page 3. Virtual Bingo Please do not try to split this PDF into individual bingo cards to send out to players. We have tools on our site to send out links to individual bingo cards. For help go to myfreebingocards.com/virtual-bingo. Help If you're having trouble printing your bingo cards or using the bingo card generator then please go to https://myfreebingocards.com/faq where you will find solutions to most common problems. Share Pin these bingo cards on Pinterest, share on Facebook, or post this link: mfbc.us/s/dtfgtk Edit and Create To add more words or make changes to this set of bingo cards go to mfbc.us/e/dtfgtk Go to myfreebingocards.com/bingo-card-generator to create a new set of bingo cards. Legal The terms of use for these printable bingo cards can be found at myfreebingocards.com/terms. -

Respiratory System
Respiratory System Course Rationale Anatomy & To pursue a career in health care, proficiency in anatomy and physiology is Physiology vital. Unit XIII Objectives Respiratory Upon completion of this lesson, the student will be able to: System • Describe biological and chemical processes that maintain homeostasis • Analyze forces and the effects of movement, torque, tension, and Essential elasticity on the human body Question • Define and decipher terms pertaining to the respiratory system How long can • Distinguish between the major organs of the respiratory system the body be • Analyze diseases and disorders of the respiratory system without • Label a diagram of the respiratory system oxygen? Engage TEKS Perform the following in front of the class using a paper towel and a hand 130.206 (c) mirror: 1 (A)(B) • Use the paper towel to clean and dry the mirror. 2(A)(D) • Hold the mirror near, but not touching, your mouth. 3 (A)(B)(E) • Exhale onto the mirror two or three times. 5 (B)(C)(D) • Examine the surface of the mirror. 6 (B) What happens to the mirror? 8 (A)(B)(C) Why does the mirror become fogged? 9 (A)(B) 10 (A)(B)(C) Or Prior Student Of all the substances the body must have to survive, oxygen is by far the most Learning critical. Think about the following: Cardiovascular system – • Without food - live a few weeks Pulmonary • Without water - live a few days Circulation • Without oxygen - live 4 – 6 minutes Estimated time 4 - 6 hours Key Points 1. Introduction – Respiratory System A. General Functions *Teacher note: 1. Brings oxygenated air to the alveoli invite a 2. -

Chest Exam Codes Code Description 1 1800 Tachypnea 2 1801 H
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Chest Exam Codes Code Description 1 1800 tachypnea 2 1801 hyperpnea 3 1802 hyperventilation 4 1803 bradypnea 5 1804 Cheyne-Stokes breathing 6 1805 ataxic breathing 7 1806 sighing respiration 8 1807 pursed lip breathing 9 1875 Prolong expiration 10 1808 Dyspneic or dyspnea-short of breath 11 1886 PT on 02 12 1809 chronic cough 13 14 1892 Upper Airway Tightness 15 1889 Respiratory Distress 16 1888 Orthopnea (difficulty breathing while lying down) 17 1885 Chest burning 18 1884 Clavicle deformity/Prominence 19 1882 Rib pain 20 1881 Chest tightness 21 1869 Abnormal Lung exam 22 23 1810 barrel chest 24 1811 funnel chest 25 1855 pectus excavatum 26 1835 Pigeon chest/pectus casrinatum 27 1839 chest wall discomfort/tenderness 28 1812 intercostal retraction 29 1813 tender pectoral muslces 30 1814 tender costal cartilages 31 1848 missing rib 32 1837 slightly protruding xyphoid tip, rib cage 33 1859 Prominent bone, sternum 34 35 1815 (Fatty-like)mass on chest 36 1816 kyphosis 37 1831 scoliosis 38 1872 poor posture 39 1817 increased AP diameter 40 1874 decreased AP diameter 41 pacemaker generator in place/ 1818 defibrillator 42 1819 Hickman catheter in precordium port-a-cath 43 44 1820 Faint/few breath sounds 45 1838 Using accessory muscles to breathe 46 1844 decreased breath sounds 47 1838 small lung volume 48 1821 (fine) rales 49 1822 crackling rales 50 1823 rhonchi 51 1824 wheeze 52 1825 obstructive breathing 53 1826 pleural rub 54 1827 basilar crackles 55 1828 bilateral crackles -
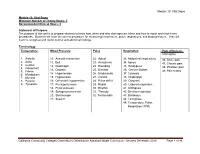
Module 10: Vital Signs
Module 10: Vital Signs Module 10: Vital Signs Minimum Number of Theory Hours: 3 Recommended Clinical Hours: 6 Statement of Purpose: The purpose of this unit is to prepare students to know how, when and why vital signs are taken and how to report and chart these procedures. Students will learn the correct procedure for measuring temperature, pulse, respirations, and blood pressure. They will learn to recognize and report normal and abnormal findings. Terminology: Temperature: Blood Pressure Pulse Respiration Pain (effects on Vital signs) 1. Afebrile 10. Aneroid manometer 22. Apical 33. Abdominal respirations 46. Acute pain 2. Axilla 11. Bell 23. Arrhythmia 34. Apnea 47. Chronic pain 3. Celsius 12. Diaphragm 24. Bounding 35. Bradypnea 4. Fahrenheit 48. Phantom pain 13. Diastolic 25. Brachial 36. Cheyne-Stokes 5. Febrile 49. Pain scales 6. Metabolism 14. Hypertension 26. Bradycardia 37. Cyanosis 7. Mucosa 15. Hypotension 27. Carotid 38. Diaphragm 8. Pyrexia 16. Orthostatic hypotension 28. Pulse deficit 39. Dyspnea 9. Tympanic 17. Pre-hypertension 29. Radial 40. Labored respiration 18. Pulse pressure 30. Rhythm 41. Orthopnea 19. Sphygmomanometer 31. Thready 42. Shallow respiration 20. Stethoscope 32. Tachycardia 43. Stertorous 21. Systolic 44. Tachypnea 45. Temperature, Pulse, Respiration (TPR) Patient, patient/resident, and client are synonymous terms Californiareferring to Community the person Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 46 receiving care Module 10: Vital Signs Patient, resident, and client are synonymous terms referring to the person receiving care Performance Standards (Objectives): Upon completion of three (3) hours of class plus homework assignments and six (6) hours of clinical experience, the student will be able to: 1. -

Chest Auscultation: Presence/Absence and Equality of Normal/Abnormal and Adventitious Breath Sounds and Heart Sounds A
Northwest Community EMS System Continuing Education: January 2012 RESPIRATORY ASSESSMENT Independent Study Materials Connie J. Mattera, M.S., R.N., EMT-P COGNITIVE OBJECTIVES Upon completion of the class, independent study materials and post-test question bank, each participant will independently do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Integrate complex knowledge of pulmonary anatomy, physiology, & pathophysiology to sequence the steps of an organized physical exam using four maneuvers of assessment (inspection, palpation, percussion, and auscultation) and appropriate technique for patients of all ages. (National EMS Education Standards) 2. Integrate assessment findings in pts who present w/ respiratory distress to form an accurate field impression. This includes developing a list of differential diagnoses using higher order thinking and critical reasoning. (National EMS Education Standards) 3. Describe the signs and symptoms of compromised ventilations/inadequate gas exchange. 4. Recognize the three immediate life-threatening thoracic injuries that must be detected and resuscitated during the “B” portion of the primary assessment. 5. Explain the difference between pulse oximetry and capnography monitoring and the type of information that can be obtained from each of them. 6. Compare and contrast those patients who need supplemental oxygen and those that would be harmed by hyperoxia, giving an explanation of the risks associated with each. 7. Select the correct oxygen delivery device and liter flow to support ventilations and oxygenation in a patient with ventilatory distress, impaired gas exchange or ineffective breathing patterns including those patients who benefit from CPAP. 8. Explain the components to obtain when assessing a patient history using SAMPLE and OPQRST.