The Main Symptoms of Pulmonary Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
Emergency Nursing Program Foreword
RESOURCE MANUAL NSW HEALTH 2011 Transition to Practice Emergency Nursing Program Foreword The role of emergency nurses requires a broad level of skill and ability to meet the care needs of patients and their families. The Transition to Emergency Nursing Program is designed to support registered nurses new to the practice of emergency nursing. The Emergency Department is a fast-moving environment within which nurses can find themselves faced with a variety of challenges across a day. This program will assist them as they develop their knowledge and skills to meet these often changing care needs within the emergency setting. The program also supports a more consistent approach to transition to emergency nursing and it is anticipated will become the standard for initial entry to practice as an emergency nurse across NSW. This Resource Manual is the core document for the program and is complemented by both the Participant Workbook and the Facilitator’s Manual. Within the Emergency Department participants will be supported by staff to meet the relevant learning objectives during the 3-6 months over which this program extends. The development of the Transition to Emergency Nursing Program has been a lengthy process which reflects the commitment of emergency nurses to their area of practice and I acknowledge and thank them for their enthusiasm and work in enabling the Program to be developed. I am sure that it will have a positive impact for those nurses new to emergency nursing and to the care of patients. 1 Adjunct Professor Debra Thoms Chief Nursing and Midwifery Officer NSW Health NSW Department of Health 73 Miller Street NORTH SYDNEY NSW 2060 Tel. -

Vitals & Assessment Bingo
Vitals & Assessment Bingo myfreebingocards.com Safety First! Before you print all your bingo cards, please print a test page to check they come out the right size and color. Your bingo cards start on Page 3 of this PDF. If your bingo cards have words then please check the spelling carefully. If you need to make any changes go to mfbc.us/e/dtfgtk Play Once you've checked they are printing correctly, print off your bingo cards and start playing! On the next page you will find the "Bingo Caller's Card" - this is used to call the bingo and keep track of which words have been called. Your bingo cards start on Page 3. Virtual Bingo Please do not try to split this PDF into individual bingo cards to send out to players. We have tools on our site to send out links to individual bingo cards. For help go to myfreebingocards.com/virtual-bingo. Help If you're having trouble printing your bingo cards or using the bingo card generator then please go to https://myfreebingocards.com/faq where you will find solutions to most common problems. Share Pin these bingo cards on Pinterest, share on Facebook, or post this link: mfbc.us/s/dtfgtk Edit and Create To add more words or make changes to this set of bingo cards go to mfbc.us/e/dtfgtk Go to myfreebingocards.com/bingo-card-generator to create a new set of bingo cards. Legal The terms of use for these printable bingo cards can be found at myfreebingocards.com/terms. -

Respiratory Failure
Respiratory Failure Phuong Vo, MD,* Virginia S. Kharasch, MD† *Division of Pediatric Pulmonary and Allergy, Boston Medical Center, Boston, MA †Division of Respiratory Diseases, Boston Children’s Hospital, Boston, MA Practice Gap The primary cause of cardiopulmonary arrest in children is unrecognized respiratory failure. Clinicians must recognize respiratory failure in its early stage of presentation and know the appropriate clinical interventions. Objectives After completing this article, readers should be able to: 1. Recognize the clinical parameters of respiratory failure. 2. Describe the respiratory developmental differences between children and adults. 3. List the clinical causes of respiratory failure. 4. Review the pathophysiologic mechanisms of respiratory failure. 5. Evaluate and diagnose respiratory failure. 6. Discuss the various clinical interventions for respiratory failure. WHAT IS RESPIRATORY FAILURE? Respiratory failure is a condition in which the respiratory system fails in oxy- genation or carbon dioxide elimination or both. There are 2 types of impaired gas exchange: (1) hypoxemic respiratory failure, which is a result of lung failure, and (2) hypercapnic respiratory failure, which is a result of respiratory pump failure (Figure 1). (1)(2) In hypoxemic respiratory failure, ventilation-perfusion (V_ =Q)_ mismatch results in the decrease of PaO2) to below 60 mm Hg with normal or low PaCO2. _ = _ (1) In hypercapnic respiratory failure, V Q mismatch results in the increase of AUTHOR DISCLOSURE Drs Vo and Kharasch fi PaCO2 to above 50 mm Hg. Either hypoxemic or hypercapnic respiratory failure have disclosed no nancial relationships can be acute or chronic. Acute respiratory failure develops in minutes to hours, relevant to this article. -

Respiratory System
Respiratory System Course Rationale Anatomy & To pursue a career in health care, proficiency in anatomy and physiology is Physiology vital. Unit XIII Objectives Respiratory Upon completion of this lesson, the student will be able to: System • Describe biological and chemical processes that maintain homeostasis • Analyze forces and the effects of movement, torque, tension, and Essential elasticity on the human body Question • Define and decipher terms pertaining to the respiratory system How long can • Distinguish between the major organs of the respiratory system the body be • Analyze diseases and disorders of the respiratory system without • Label a diagram of the respiratory system oxygen? Engage TEKS Perform the following in front of the class using a paper towel and a hand 130.206 (c) mirror: 1 (A)(B) • Use the paper towel to clean and dry the mirror. 2(A)(D) • Hold the mirror near, but not touching, your mouth. 3 (A)(B)(E) • Exhale onto the mirror two or three times. 5 (B)(C)(D) • Examine the surface of the mirror. 6 (B) What happens to the mirror? 8 (A)(B)(C) Why does the mirror become fogged? 9 (A)(B) 10 (A)(B)(C) Or Prior Student Of all the substances the body must have to survive, oxygen is by far the most Learning critical. Think about the following: Cardiovascular system – • Without food - live a few weeks Pulmonary • Without water - live a few days Circulation • Without oxygen - live 4 – 6 minutes Estimated time 4 - 6 hours Key Points 1. Introduction – Respiratory System A. General Functions *Teacher note: 1. Brings oxygenated air to the alveoli invite a 2. -

Chest Exam Codes Code Description 1 1800 Tachypnea 2 1801 H
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Chest Exam Codes Code Description 1 1800 tachypnea 2 1801 hyperpnea 3 1802 hyperventilation 4 1803 bradypnea 5 1804 Cheyne-Stokes breathing 6 1805 ataxic breathing 7 1806 sighing respiration 8 1807 pursed lip breathing 9 1875 Prolong expiration 10 1808 Dyspneic or dyspnea-short of breath 11 1886 PT on 02 12 1809 chronic cough 13 14 1892 Upper Airway Tightness 15 1889 Respiratory Distress 16 1888 Orthopnea (difficulty breathing while lying down) 17 1885 Chest burning 18 1884 Clavicle deformity/Prominence 19 1882 Rib pain 20 1881 Chest tightness 21 1869 Abnormal Lung exam 22 23 1810 barrel chest 24 1811 funnel chest 25 1855 pectus excavatum 26 1835 Pigeon chest/pectus casrinatum 27 1839 chest wall discomfort/tenderness 28 1812 intercostal retraction 29 1813 tender pectoral muslces 30 1814 tender costal cartilages 31 1848 missing rib 32 1837 slightly protruding xyphoid tip, rib cage 33 1859 Prominent bone, sternum 34 35 1815 (Fatty-like)mass on chest 36 1816 kyphosis 37 1831 scoliosis 38 1872 poor posture 39 1817 increased AP diameter 40 1874 decreased AP diameter 41 pacemaker generator in place/ 1818 defibrillator 42 1819 Hickman catheter in precordium port-a-cath 43 44 1820 Faint/few breath sounds 45 1838 Using accessory muscles to breathe 46 1844 decreased breath sounds 47 1838 small lung volume 48 1821 (fine) rales 49 1822 crackling rales 50 1823 rhonchi 51 1824 wheeze 52 1825 obstructive breathing 53 1826 pleural rub 54 1827 basilar crackles 55 1828 bilateral crackles -
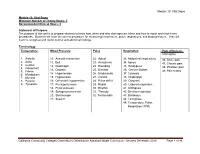
Module 10: Vital Signs
Module 10: Vital Signs Module 10: Vital Signs Minimum Number of Theory Hours: 3 Recommended Clinical Hours: 6 Statement of Purpose: The purpose of this unit is to prepare students to know how, when and why vital signs are taken and how to report and chart these procedures. Students will learn the correct procedure for measuring temperature, pulse, respirations, and blood pressure. They will learn to recognize and report normal and abnormal findings. Terminology: Temperature: Blood Pressure Pulse Respiration Pain (effects on Vital signs) 1. Afebrile 10. Aneroid manometer 22. Apical 33. Abdominal respirations 46. Acute pain 2. Axilla 11. Bell 23. Arrhythmia 34. Apnea 47. Chronic pain 3. Celsius 12. Diaphragm 24. Bounding 35. Bradypnea 4. Fahrenheit 48. Phantom pain 13. Diastolic 25. Brachial 36. Cheyne-Stokes 5. Febrile 49. Pain scales 6. Metabolism 14. Hypertension 26. Bradycardia 37. Cyanosis 7. Mucosa 15. Hypotension 27. Carotid 38. Diaphragm 8. Pyrexia 16. Orthostatic hypotension 28. Pulse deficit 39. Dyspnea 9. Tympanic 17. Pre-hypertension 29. Radial 40. Labored respiration 18. Pulse pressure 30. Rhythm 41. Orthopnea 19. Sphygmomanometer 31. Thready 42. Shallow respiration 20. Stethoscope 32. Tachycardia 43. Stertorous 21. Systolic 44. Tachypnea 45. Temperature, Pulse, Respiration (TPR) Patient, patient/resident, and client are synonymous terms Californiareferring to Community the person Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 46 receiving care Module 10: Vital Signs Patient, resident, and client are synonymous terms referring to the person receiving care Performance Standards (Objectives): Upon completion of three (3) hours of class plus homework assignments and six (6) hours of clinical experience, the student will be able to: 1. -

Chest Auscultation: Presence/Absence and Equality of Normal/Abnormal and Adventitious Breath Sounds and Heart Sounds A
Northwest Community EMS System Continuing Education: January 2012 RESPIRATORY ASSESSMENT Independent Study Materials Connie J. Mattera, M.S., R.N., EMT-P COGNITIVE OBJECTIVES Upon completion of the class, independent study materials and post-test question bank, each participant will independently do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Integrate complex knowledge of pulmonary anatomy, physiology, & pathophysiology to sequence the steps of an organized physical exam using four maneuvers of assessment (inspection, palpation, percussion, and auscultation) and appropriate technique for patients of all ages. (National EMS Education Standards) 2. Integrate assessment findings in pts who present w/ respiratory distress to form an accurate field impression. This includes developing a list of differential diagnoses using higher order thinking and critical reasoning. (National EMS Education Standards) 3. Describe the signs and symptoms of compromised ventilations/inadequate gas exchange. 4. Recognize the three immediate life-threatening thoracic injuries that must be detected and resuscitated during the “B” portion of the primary assessment. 5. Explain the difference between pulse oximetry and capnography monitoring and the type of information that can be obtained from each of them. 6. Compare and contrast those patients who need supplemental oxygen and those that would be harmed by hyperoxia, giving an explanation of the risks associated with each. 7. Select the correct oxygen delivery device and liter flow to support ventilations and oxygenation in a patient with ventilatory distress, impaired gas exchange or ineffective breathing patterns including those patients who benefit from CPAP. 8. Explain the components to obtain when assessing a patient history using SAMPLE and OPQRST. -

Respiratory Distress
Respiratory Distress National Pediatric Nighttime Curriculum Written by Liane Campbell, MD Lucile Packard Children’s Hospital, Stanford University Learning Objectives Review the initial assessment of patient in respiratory distress Review management of specific causes of respiratory distress Upper airway obstruction Lower airway obstruction Lung tissue disease Disordered control of breathing During a busy night, you get the following page: FYI: Sally, a 2 year old with PNA had a desat to 88% while on 4L NC. What do you do next? What initial management steps would you take? How do you initially assess a patient in respiratory distress? Initial Assesment Rapid assessment Quickly determine severity of respiratory condition and stabilize child Respiratory distress can quickly lead to cardiac compromise Airway Support or open airway with jaw thrust Suction and position patient Breathing Provide high concentration oxygen Bag mask ventilation Prepare for intubation Administer medication ie albuterol, epinephrine Circulation Establish vascular access: IV/IO History and Physical Exam History Physical Exam Trauma Mental status Change in voice Position of comfort Onset of symptoms Nasal flaring Associated symptoms Accessory muscle use Exposures Respiratory rate and Underlying medical pattern conditions Auscultation for abnormal breath sounds What initial studies would you get for a patient in respiratory distress? Initial studies Pulse oximetry May be difficult in agitated patient May be falsely decreased in very anemic -

1. Thoracic: Pertaining to Chest 2
1. Thoracic: Pertaining to chest 2. Anosmia: Without smell 3. Anoxia: Receiving almost no oxygen 4. Aphonia: Condition of being unable to produce sounds 5. Apnea: Not breathing 6. Asphyxia: Lack of oxygen that can produce unconsciousness or death 7. Tachypnea: Very fast breathing 8. Bradypnea: Very slow breathing 9. Bronchiectasis: Dilated bronchus 10. Bronchospasm: Involuntary smooth muscles spasm of bronchus 11. Cyanosis: Bluish tint to skin 12. Dysphonia: Not producing sounds or producing abnormal sounds 13. Dyspnea: Labored breathing 14. Eupnea: Normal breathing/respiratory rate 15. Hemoptysis: Blood stained septum 16. Hemothorax: Blood in the thoracic cavity 17. Hypercapnia: Excessive carbon dioxide in the body 18. Hyperpnea: Taking deep breaths 19. Hypopnea: Shallow breaths 20. Hypoxemia: Too little oxygen in blood stream 21. Orthopnea: Dyspnea worsened by laying flat 22. Pansinusitis: Inflammation of all the sinuses 23. Pleurodynia: Pleural pain 24. Pyothorax: Pus in the chest cavity 25. Mycothorax: Fungus in the chest cavity 26. Laryngostenosis: Narrowing in the larynx 27. Pertussis: Cough 28. Rhinomycosis: Fungus in the nose cavity 29. Bronchiectasis: Abnormal enlargement of the bronchi 30. Bronchogenic carcinoma: Malignant tumor originating in the bronchi Associated with the history of smoking 31. Atelecasis: Incomplete dilation of the aveoli Failure in new born lungs 32. Cystic Fibrosis: Hereditary malfunctioning of the endocrine (book says exocrine) glands 33. Mycoplasma pneumonia: Fungus formation 34. Pneumothorax: Collection of air or gas in the pleural cavity, which may result in collapse of the lung 35. Ausculation: Listening to sounds within body by using stethoscope 36. Pathogenic: Pertaining to microscopic organisms, such as bacteria, capable of causing disease 37. -

Module 12: Emergency Procedures California Community Colleges
Module 12: Emergency Procedures Module 12: Emergency Procedures Minimum Number of Theory Hours: 2 Recommended Clinical Hours: 1 Statement of Purpose: The purpose of this unit is to introduce the student to the concepts and procedures related to emergency procedures, signs and symptoms of distress, and the role of the Nurse Assistant in Long Term Care (LTC) in the response to immediate and temporary intervention in emergency situations. Terminology: 1. Abdominal thrusts 19. Emergency Medical Services (EMS) 2. Advance directive 20. Heimlich maneuver 3. Agitation 21. Hemiplegia 4. Airway 22. Hemorrhage 5. Aphasia 23. Hyperventilation 6. Aspirate 24. Hypoglycemia 7. Automated External Device (AED) 25. Hypoventilation 8. Barrier device 26. Hypoxia 9. Bradypnea 27. Pallor 10. Breathing 28. Pocket mask 11. Cardiac arrest 29. Recovery position 12. Cardiopulmonary Resuscitation (CPR) 30. Respiratory arrest 13. Compressions, Airway, Breathing (CAB)-formerly (ABC) 31. Respiratory distress 14. Cyanosis 32. Stat 15. Defibrillator 33. Syncope 16. Diaphoresis 34. Tachypnea 17. Do Not Resuscitate (DNR) 35. Unconscious 18. Dyspnea Patient, resident, and client are synonymous terms referring to the person receiving care California Community Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 24 Module 12: Emergency Procedures Performance Standards (Objectives): 1. Define key terminology. 2. Identify common signs and symptoms of conditions associated with patient/resident distress and describe the Nurse Assistant’s role and responsibility in preventing and/or responding. 3. Describe the immediate interventions in a medical emergency. 4. List the causes and signs of choking and discuss the use of abdominal thrusts for relief of obstructed airway. -

Vital Signs and Pain Scale
CSI 101 Skills Lab # 2 Vital Signs Notes (updated: 6/2018) Vital Signs and Pain Scale: Five Components of Vital Signs: 1. Temperature: Normal Ranges (36.5o– 37.2oC or 97.8o – 99oF) 2. Pulse Rate: 60-100/min 3. Respirations Rate: 12-20/min 4. Blood Pressure: 120/80 mmHg 5. Pain Assessment: Numerical, Descriptive & Visual Temperature: Orally: 37oC Tympanic: 37oC Rectally: 37.5oC Skin: 37oC Axillary: 36.5oC Healthy individual body temperature deviates from 36.5-37.2o C. Cells, tissues and organs function best at these temperatures. Normal body temperature is 37o C or 98.6oF. The bodies temperature is regulated by the anterior hypothalamus (protecting from hyperthermia) and posterior hypothalamus (protecting from hypothermia). Factors Influencing Body Temperature: Hypothermia (< 95oF): decrease metabolic rate, inadequate clothing, cold environment, drug / alcohol consumption, inactivity, aging. Hyperthermia (>100oF): increase metabolic rate, inappropriate clothing, hot environment, inability to perspire, medications, infectious process, exercise. Increased body metabolism and metabolic activity accompany elevations in body temperature and may be as high as 10 –13 percent for each 1oC. Increased metabolic demand results in a increase in oxygen consumption. Pulse and respirations: increase in pulse 10-15 beats/min. with each 1oC. Respiratory rate is increased due to the increase in oxygen demand. Pulse: Infant: 120-160/min Toddler: 90-140/min Adult: 60-100/min To calculate Maximum Heart Rate: 220 – age = _______ (Ex: 220 – 26 = 194) Pulse sites: Temporal, Carotid, Brachial, Radial, femoral and Apical (for infants). Pulse rate: count for 15 seconds and multiply by 4. When pulse feels irregular, take for entire minute.