Annual Report January – December 2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Code Under Name Girls Boys Total Girls Boys Total 010290001
P|D|LL|S G8 G10 Code Under Name Girls Boys Total Girls Boys Total 010290001 Maiwakhola Gaunpalika Patidanda Ma Vi 15 22 37 25 17 42 010360002 Meringden Gaunpalika Singha Devi Adharbhut Vidyalaya 8 2 10 0 0 0 010370001 Mikwakhola Gaunpalika Sanwa Ma V 27 26 53 50 19 69 010160009 Phaktanglung Rural Municipality Saraswati Chyaribook Ma V 28 10 38 33 22 55 010060001 Phungling Nagarpalika Siddhakali Ma V 11 14 25 23 8 31 010320004 Phungling Nagarpalika Bhanu Jana Ma V 88 77 165 120 130 250 010320012 Phungling Nagarpalika Birendra Ma V 19 18 37 18 30 48 010020003 Sidingba Gaunpalika Angepa Adharbhut Vidyalaya 5 6 11 0 0 0 030410009 Deumai Nagarpalika Janta Adharbhut Vidyalaya 19 13 32 0 0 0 030100003 Phakphokthum Gaunpalika Janaki Ma V 13 5 18 23 9 32 030230002 Phakphokthum Gaunpalika Singhadevi Adharbhut Vidyalaya 7 7 14 0 0 0 030230004 Phakphokthum Gaunpalika Jalpa Ma V 17 25 42 25 23 48 030330008 Phakphokthum Gaunpalika Khambang Ma V 5 4 9 1 2 3 030030001 Ilam Municipality Amar Secondary School 26 14 40 62 48 110 030030005 Ilam Municipality Barbote Basic School 9 9 18 0 0 0 030030011 Ilam Municipality Shree Saptamai Gurukul Sanskrit Vidyashram Secondary School 0 17 17 1 12 13 030130001 Ilam Municipality Purna Smarak Secondary School 16 15 31 22 20 42 030150001 Ilam Municipality Adarsha Secondary School 50 60 110 57 41 98 030460003 Ilam Municipality Bal Kanya Ma V 30 20 50 23 17 40 030460006 Ilam Municipality Maheshwor Adharbhut Vidyalaya 12 15 27 0 0 0 030070014 Mai Nagarpalika Kankai Ma V 50 44 94 99 67 166 030190004 Maijogmai Gaunpalika -

Nepal Human Rights Year Book 2021 (ENGLISH EDITION) (This Report Covers the Period - January to December 2020)
Nepal Human Rights Year Book 2021 (ENGLISH EDITION) (This Report Covers the Period - January to December 2020) Editor-In-Chief Shree Ram Bajagain Editor Aarya Adhikari Editorial Team Govinda Prasad Tripathee Ramesh Prasad Timalsina Data Analyst Anuj KC Cover/Graphic Designer Gita Mali For Human Rights and Social Justice Informal Sector Service Centre (INSEC) Nagarjun Municipality-10, Syuchatar, Kathmandu POBox : 2726, Kathmandu, Nepal Tel: +977-1-5218770 Fax:+977-1-5218251 E-mail: [email protected] Website: www.insec.org.np; www.inseconline.org All materials published in this book may be used with due acknowledgement. First Edition 1000 Copies February 19, 2021 © Informal Sector Service Centre (INSEC) ISBN: 978-9937-9239-5-8 Printed at Dream Graphic Press Kathmandu Contents Acknowledgement Acronyms and Abbreviations Foreword CHAPTERS Chapter 1 Situation of Human Rights in 2020: Overall Assessment Accountability Towards Commitment 1 Review of the Social and Political Issues Raised in the Last 29 Years of Nepal Human Rights Year Book 25 Chapter 2 State and Human Rights Chapter 2.1 Judiciary 37 Chapter 2.2 Executive 47 Chapter 2.3 Legislature 57 Chapter 3 Study Report 3.1 Status of Implementation of the Labor Act at Tea Gardens of Province 1 69 3.2 Witchcraft, an Evil Practice: Continuation of Violence against Women 73 3.3 Natural Disasters in Sindhupalchok and Their Effects on Economic and Social Rights 78 3.4 Problems and Challenges of Sugarcane Farmers 82 3.5 Child Marriage and Violations of Child Rights in Karnali Province 88 36 Socio-economic -

44214-024: Building Climate Resilience of Watersheds In
Building Climate Resilience of Watersheds in Mountain Eco-Regions (RRP NEP 44214) Environmental Assessment and Review Framework ADB TA 7883-NEP July 2013 Nepal: Building Climate Resilience of Watersheds in Mountain Eco-Regions Prepared by Department of Soil Conservation and Watershed Management for the Asian Development Bank CURRENCY EQUIVALENTS (as of 1 December 2012) Currency unit – Nepalese Rupee (NR) NR1.00 = $0.0115 $1.00 = NR 86.9 ABBREVIATIONS ADB – Asian Development Bank CDG – Community Development Group CFUG – Community Forest User Group CPC – Consultation, Participation and Communications (Plan) DAGs – disadvantaged groups DDR – Due Diligence Reports DFO – District Forestry Office DSCO – District Soil Conservation Office DSCWM – Department of Soil Conservation and Watershed Management DSO – DSCO Safeguard Officer DSS – District Safeguard Specialist EARF – Environmental Assessment and Review Framework EIA – Environmental Impact Assessment GESI – Gender Empowerment and Social Inclusion (Plan) GON – Government of Nepal GPP – Grievance Point Person IEE – Initial Environmental Examination MoFSC – Ministry of Forests and Soil Conservation NAPA – National Adaptation Program of Action NES – National Environmental Specialist PIC – Project Implementation Consultant PMU – Project Management Unit REA – Rapid Environmental Assessment R/LAP – Resettlement and Land Acquisition Plan SPCR – Strategic Program for Climate Resilience SEU – Social and Environmental Unit SWMC – Sub-watershed Management Committee VDC – Village Development Committee VDT – Village Development Team WEIGHTS AND MEASURES cm – centimeter cu m – cubic meters Ha hectare km – kilometer L – liter m – meter masl – meters above sea level sq m square meter NOTE (i) In this report, "$" refers to US dollars. This environmental assessment and review framework is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. -
CECI Nepal's Newsletter
INSIDE THIS ISSUE: CECI Nepal AGM 1 Celebration of Open Data Day 4 National Advocacy Campaign 6 Creating Jobs 7 Uniterra Towards Fostering 12 CECI Nepal’s Partnership Partner Organization Workshop 13 Newsletter Volunteer’s Blog: Status of 14 Women in Nepal SUSASAN in Media 15 January-April 2019 1 VOLUME , ISSUE 2 VOLUME , ISSUE Dear Friends, MESSAGE Welcome to the CECI Nepal’s Newsletter “REFLECT”! I am delighted to present you the latest edition of CECI Nepal’s newslet- ter “REFLECT”. In this edition, you will get a glimpse of our major activi- FROM THE ties carried out between January to April, 2019. In this quarter, we are almost at the end of Livelihood Promotion for Earthquake aected Population in Nepal (PUNARNIRMAN) project and COUNTRY wrapping up its activities. The most exciting part of PUNARNIRMAN project is the local government has shown their willingness to support further and beneciaries are linked to the local institutions. At the same DIRECTOR time, we are looking forward to the year ahead as we build on our com- mitment to capacity building of CSOs for good governance, gender equal- ity and social inclusion. I would like to thank all our partners, including government agencies, Australian Government Department of Foreign Aairs and Trade (DFAT), Global Aairs Canada (GAC), INGOs and civil society organizations for their continued cooperation and invaluable work with us. Everyday, I see the team moving forward with their full commitment in achieving CECI’s mission and I would like to oer my sincere thanks to the CECI Nepal team and volunteers for their support and dedication. -

COVID19 Reporting of Naukunda RM, Rasuwa.Pdf
स्थानिय तहको विवरण प्रदेश जिल्ला स्थानिय तहको नाम Bagmati Rasuwa Naukunda Rural Mun सूचना प्रविधि अधिकृत पद नाम सम्पर्क नं. वडा ठेगाना कैफियत सूचना प्रविधि अधिकृतसुमित कुमार संग्रौला 9823290882 ६ गोसाईकुण्ड गाउँपालिका जिम्मेवार पदाधिकारीहरू क्र.स. पद नाम सम्पर्क नं. वडा ठेगाना कैफियत 1 प्रमुख प्रशासकीय अधिकृतनवदीप राई 9807365365 १३ विराटनगर, मोरङ 2 सामजिक विकास/ स्वास्थ्यअण प्रसाद शाखा पौडेल प्रमुख 9818162060 ५ शुभ-कालिका गाउँपालिका, रसुवा 3 सूचना अधिकारी डबल बहादुर वि.के 9804669795 ५ धनगढी उपमहानगरपालिका, कालिका 4 अन्य नितेश कुमार यादव 9816810792 ६ पिपरा गाउँपालिका, महोत्तरी 5 6 n विपद व्यवस्थापनमा सहयोगी संस्थाहरू क्र.स. प्रकार नाम सम्पर्क नं. वडा ठेगाना कैफियत 1 2 3 4 5 6 7 8 9 n ारेाइन केको ववरण ID ारेाइन केको नाम वडा ठेगाना केन्द्रको सम्पर्क व्यक्तिसम्पर्क नं. भवनको प्रकार बनाउने निकाय वारेटाइन केको मता Geo Location (Lat, Long) Q1 गौतम बुद्ध मा.वि क्वारेन्टाइन स्थल ३ फाम्चेत नितेश कुमार यादव 9816810792 विध्यालय अन्य (वेड संया) 10 28.006129636870693,85.27118702477858 Q2 Q3 Q4 Q5 Q6 Q7 Q8 Q9 Q10 Q11 Qn भारत लगायत विदेशबाट आएका व्यक्तिहरूको विवरण अधारभूत विवरण ारेाइन/अताल रफर वा घर पठाईएको ववरण विदेशबाट आएको हो भने मात्र कैिफयत ID नाम, थर लिङ्ग उमेर (वर्ष) वडा ठेगाना सम्पर्क नं. -

Kanchanpur District
District Transport Master Plan (DTMP) For Kanchanpur District ------------------------------------------------------------------------------------------------------------------------------------------------ Government of Nepal District Transport Master Plan (DTMP) of Kanchanpur District Ministry of Federal Affairs and Local Development Department of Local Infrastructure Development and Agricultural Roads (DOLIDAR) District Development Committee, Kanchanpur Volume I Final Report January. 2016 Prepared by: Project Research and Engineering Associates for the District Development Committee (DDC) and District Technical Office (DTO), with Technical Assistance from the Department of Local Infrastructure and Agricultural Roads (DOLIDAR), Ministry of Federal Affairs and Local Development and grant supported by DFID through Rural Access Programme (RAP3). District Transport Master Plan (DTMP) For Kanchanpur District ------------------------------------------------------------------------------------------------------------------------------------------------ ------------------------------------------------------------------------------------------------------------------------------------------------ Project Research and Engineering Associates 1 District Transport Master Plan (DTMP) For Kanchanpur District ------------------------------------------------------------------------------------------------------------------------------------------------ Project Research and Engineering Associates Lagankhel, Lalitpur Phone: 5539607 Email: [email protected] -

Feasibility Study of Kailash Sacred Landscape
Kailash Sacred Landscape Conservation Initiative Feasability Assessment Report - Nepal Central Department of Botany Tribhuvan University, Kirtipur, Nepal June 2010 Contributors, Advisors, Consultants Core group contributors • Chaudhary, Ram P., Professor, Central Department of Botany, Tribhuvan University; National Coordinator, KSLCI-Nepal • Shrestha, Krishna K., Head, Central Department of Botany • Jha, Pramod K., Professor, Central Department of Botany • Bhatta, Kuber P., Consultant, Kailash Sacred Landscape Project, Nepal Contributors • Acharya, M., Department of Forest, Ministry of Forests and Soil Conservation (MFSC) • Bajracharya, B., International Centre for Integrated Mountain Development (ICIMOD) • Basnet, G., Independent Consultant, Environmental Anthropologist • Basnet, T., Tribhuvan University • Belbase, N., Legal expert • Bhatta, S., Department of National Park and Wildlife Conservation • Bhusal, Y. R. Secretary, Ministry of Forest and Soil Conservation • Das, A. N., Ministry of Forest and Soil Conservation • Ghimire, S. K., Tribhuvan University • Joshi, S. P., Ministry of Forest and Soil Conservation • Khanal, S., Independent Contributor • Maharjan, R., Department of Forest • Paudel, K. C., Department of Plant Resources • Rajbhandari, K.R., Expert, Plant Biodiversity • Rimal, S., Ministry of Forest and Soil Conservation • Sah, R.N., Department of Forest • Sharma, K., Department of Hydrology • Shrestha, S. M., Department of Forest • Siwakoti, M., Tribhuvan University • Upadhyaya, M.P., National Agricultural Research Council -
Forests and Watershed Profile of Local Level (744) Structure of Nepal
Forests and Watershed Profile of Local Level (744) Structure of Nepal Volumes: Volume I : Forest & Watershed Profile of Province 1 Volume II : Forest & Watershed Profile of Province 2 Volume III : Forest & Watershed Profile of Province 3 Volume IV : Forest & Watershed Profile of Province 4 Volume V : Forest & Watershed Profile of Province 5 Volume VI : Forest & Watershed Profile of Province 6 Volume VII : Forest & Watershed Profile of Province 7 Government of Nepal Ministry of Forests and Soil Conservation Department of Forest Research and Survey Kathmandu July 2017 © Department of Forest Research and Survey, 2017 Any reproduction of this publication in full or in part should mention the title and credit DFRS. Citation: DFRS, 2017. Forests and Watershed Profile of Local Level (744) Structure of Nepal. Department of Forest Research and Survey (DFRS). Kathmandu, Nepal Prepared by: Coordinator : Dr. Deepak Kumar Kharal, DG, DFRS Member : Dr. Prem Poudel, Under-secretary, DSCWM Member : Rabindra Maharjan, Under-secretary, DoF Member : Shiva Khanal, Under-secretary, DFRS Member : Raj Kumar Rimal, AFO, DoF Member Secretary : Amul Kumar Acharya, ARO, DFRS Published by: Department of Forest Research and Survey P. O. Box 3339, Babarmahal Kathmandu, Nepal Tel: 977-1-4233510 Fax: 977-1-4220159 Email: [email protected] Web: www.dfrs.gov.np Cover map: Front cover: Map of Forest Cover of Nepal FOREWORD Forest of Nepal has been a long standing key natural resource supporting nation's economy in many ways. Forests resources have significant contribution to ecosystem balance and livelihood of large portion of population in Nepal. Sustainable management of forest resources is essential to support overall development goals. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

Peace Events in Sixteen Project Communities (28 Events Comprising Peace Rally, Cultural Progam,Speech Competition, Interaction, Sports and Revolving Fund)
ssi 2017 Peace Events in Sixteen Project Communities (28 events comprising Peace Rally, Cultural Progam,Speech Competition, Interaction, Sports and Revolving Fund) From Combatants to Peacemakers Program Submitted to THE DEMOCRACY AND GOVERNANCE OFFICE THE UNITED STATES AGENCY FOR INTERNATIONAL DEVELOPMENT (USAID) MISSION Maharajgunj, Kathmandu, Nepal Submitted by Pro Public Kuleswore, Kathmandu P.O. Box: 14307 Telephone: +977-01-4283469 Email: [email protected] i Disclaimer: All these activities were made possible by the generous support of the American people through the United States Agency for International Development (USAID). The contents are the responsibility of Pro Public and do not necessarily reflect the views of USAID or the United States Government. ii Abbreviations CBO Community Based Organization CDO Chief District Officer C2P Combatants to Peacemakers CPN Communist Party of Nepal CSO Civil Society Organization DDC District Development Committee DE Dalit and Ethnic Communities DF Dialogue facilitation ECs Ex-Combatants FGD Focus Group Discussion GESI Gender and Social Inclusion GIZ Deutsche GesellschaftFür Internationale Zusammenarbeit (GIZ) GmbH KII Key Informant Interview LDO Local Development Office LPC Local Peace Committee NC Nepali Congress NPTF Nepal Peace Trust Fund PLA People Liberation Army Pro Public Forum for the Protection of Public Interest SDG Social Dialogue Group SM Social Mobilizer STPP Strengthening the Peace Process UCPN United Communist Party of Nepal UML United Marxist Leninist UNDP United Nations Development Program USAID United States Agency for International Development VDC Village Development Committee WCF Ward Citizen Forum iii Acknowledgement This report briefly summarizes the activity report of peace events organized by Pro Public under the 'Combatants to Peacemakers' Program (C2P) supported by United States Agency for International Development (USAID), during the period of September 2016 to May 2017. -

Japan International Cooperation Agency (JICA)
Chapter 3 Project Evaluation and Recommendations 3-1 Project Effect It is appropriate to implement the Project under Japan's Grant Aid Assistance, because the Project will have the following effects: (1) Direct Effects 1) Improvement of Educational Environment By replacing deteriorated classrooms, which are danger in structure, with rainwater leakage, and/or insufficient natural lighting and ventilation, with new ones of better quality, the Project will contribute to improving the education environment, which will be effective for improving internal efficiency. Furthermore, provision of toilets and water-supply facilities will greatly encourage the attendance of female teachers and students. Present(※) After Project Completion Usable classrooms in Target Districts 19,177 classrooms 21,707 classrooms Number of Students accommodated in the 709,410 students 835,820 students usable classrooms ※ Including the classrooms to be constructed under BPEP-II by July 2004 2) Improvement of Teacher Training Environment By constructing exclusive facilities for Resource Centres, the Project will contribute to activating teacher training and information-sharing, which will lead to improved quality of education. (2) Indirect Effects 1) Enhancement of Community Participation to Education Community participation in overall primary school management activities will be enhanced through participation in this construction project and by receiving guidance on various educational matters from the government. 91 3-2 Recommendations For the effective implementation of the project, it is recommended that HMG of Nepal take the following actions: 1) Coordination with other donors As and when necessary for the effective implementation of the Project, the DOE should ensure effective coordination with the CIP donors in terms of the CIP components including the allocation of target districts. -
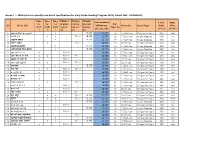
Annex 1 : - Srms Print Run Quantity and Detail Specifications for Early Grade Reading Program 2019 ( Cohort 1&2 : 16 Districts)
Annex 1 : - SRMs print run quantity and detail specifications for Early Grade Reading Program 2019 ( Cohort 1&2 : 16 Districts) Number Number Number Titles Titles Titles Total numbers Cover Inner for for for of print of print of print # of SN Book Title of Print run Book Size Inner Paper Print Print grade grade grade run for run for run for Inner Pg (G1, G2 , G3) (Color) (Color) 1 2 3 G1 G2 G3 1 अनारकल�को अꅍतरकथा x - - 15,775 15,775 24 17.5x24 cms 130 gms Art Paper 4X0 4x4 2 अनौठो फल x x - 16,000 15,775 31,775 28 17.5x24 cms 80 gms Maplitho 4X0 1x1 3 अमु쥍य उपहार x - - 15,775 15,775 40 17.5x24 cms 80 gms Maplitho 4X0 1x1 4 अत� र बु饍�ध x - 16,000 - 16,000 36 21x27 cms 130 gms Art Paper 4X0 4x4 5 अ쥍छ�को औषधी x - - 15,775 15,775 36 17.5x24 cms 80 gms Maplitho 4X0 1x1 6 असी �दनमा �व�व भ्रमण x - - 15,775 15,775 32 17.5x24 cms 80 gms Maplitho 4X0 1x1 7 आउ गन� १ २ ३ x 16,000 - - 16,000 20 17.5x24 cms 130 gms Art Paper 4X0 4x4 8 आज मैले के के जान� x x 16,000 16,000 - 32,000 16 17.5x24 cms 130 gms Art Paper 4X0 4x4 9 आ굍नो घर राम्रो घर x 16,000 - - 16,000 20 21x27 cms 130 gms Art Paper 4X0 4x4 10 आमा खुसी हुनुभयो x x 16,000 16,000 - 32,000 20 21x27 cms 130 gms Art Paper 4X0 4x4 11 उप配यका x - - 15,775 15,775 20 14.8x21 cms 130 gms Art Paper 4X0 4X4 12 ऋतु गीत x x 16,000 16,000 - 32,000 16 17.5x24 cms 130 gms Art Paper 4X0 4x4 13 क का �क क� x 16,000 - - 16,000 16 14.8x21 cms 130 gms Art Paper 4X0 4x4 14 क दे�ख � स륍म x 16,000 - - 16,000 20 17.5x24 cms 130 gms Art Paper 2X0 2x2 15 कता�तर छौ ? x 16,000 - - 16,000 20 17.5x24 cms 130 gms Art Paper 2X0 2x2